J Cerebrovasc Endovasc Neurosurg.
2023 Dec;25(4):411-419. 10.7461/jcen.2023.E2023.01.003.
Optochiasmatic cavernoma: Surgical treatment and outcomes
- Affiliations
-
- 1Department of Neurosurgery, N.N. Burdenko National Medical Research Center of Neurosurgery of the Ministry of Health of the Russian Federation (BNC), Moscow, Russia
- 2Department of Neurosurgery, Neurosurgery Clinic, Birgunj, Nepal
- KMID: 2549446
- DOI: http://doi.org/10.7461/jcen.2023.E2023.01.003
Abstract
Objective
Optochiasmatic cavernoma is an extremely rare cerebral lesion. They account for approximately 1% of all cavernomas of the central nervous system. Reports on this pathology are limited. Abrupt visual deterioration is a common symptom of the disease. Treatment strategy and visual outcomes after different treatment approaches remain a subject for discussion.
Methods
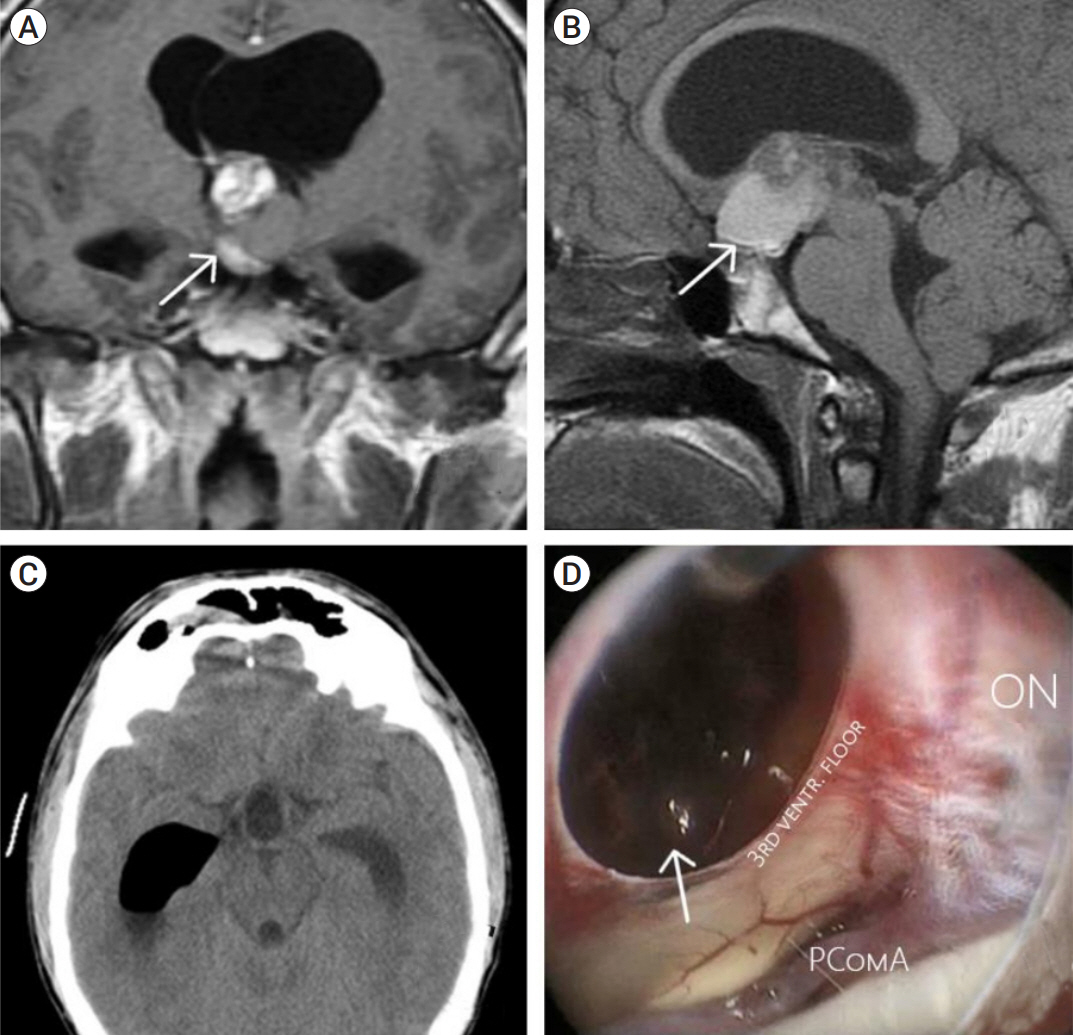
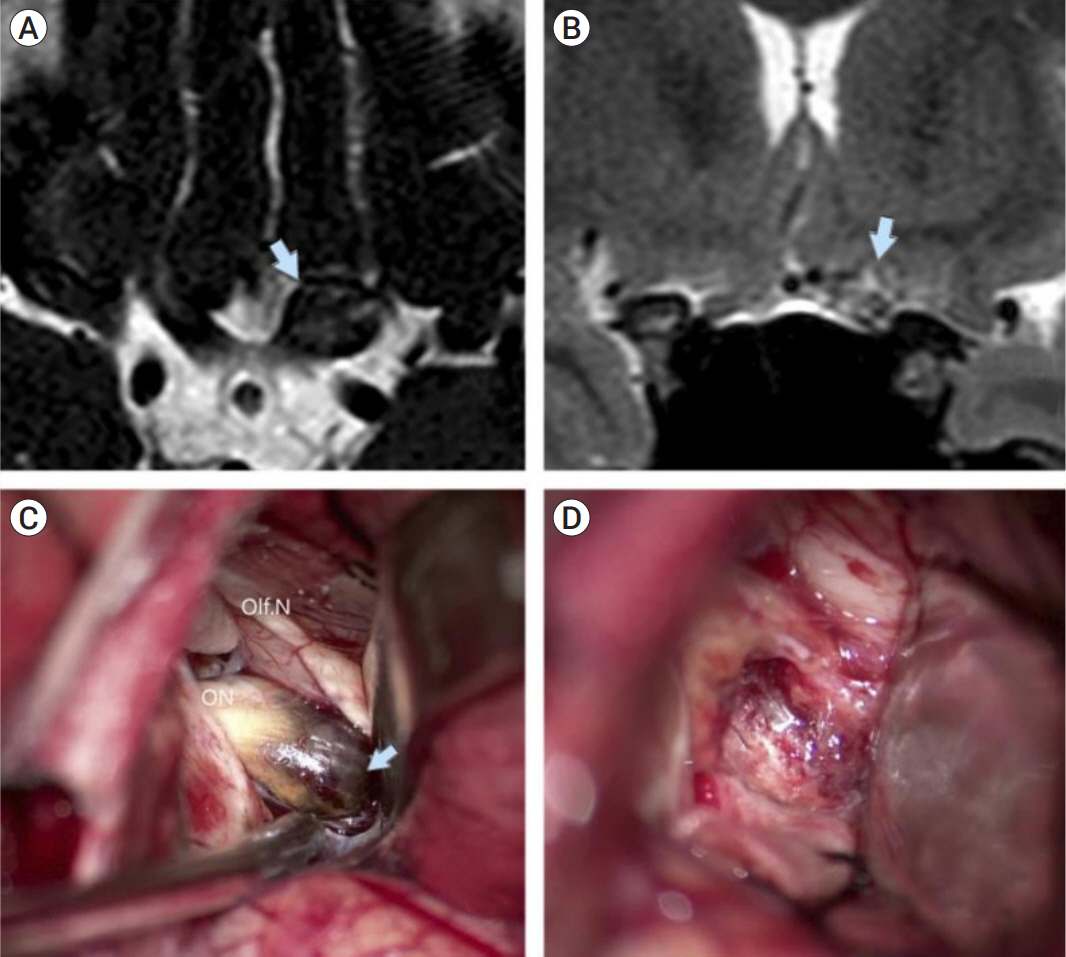
Patients operated in a period 2005-2021 were analyzed in this study. All patients preoperatively underwent computed tomography (CT) scan, CT-angiography, and magnetic resonance imaging (MRI). Visual function of the patients was assessed pre-op, post-op and at the follow-up. Duration of visual dysfunction was noted as well. Surgical details were also extracted from medical notes. All patients were followed up, and control MRI was performed one month after operation. We assessed surgical series of optochiasmatic cavernomas published for last 10 years. Further comparative analysis with our data was performed.
Results
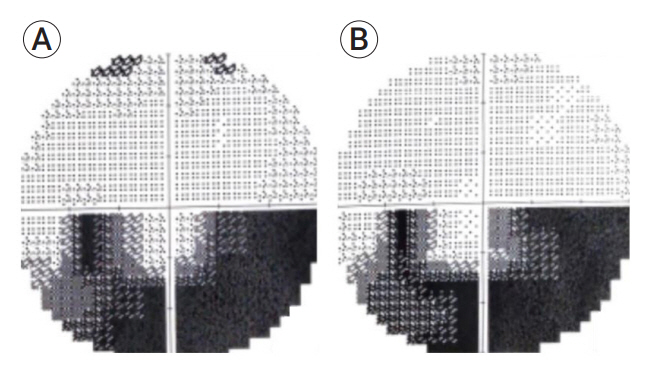
Five patients were included into this study. There were four men and one woman. Mean age comprised 33.8 years (range 20-48 years). Most patients were admitted to our hospital due to visual disturbances (80%). Visual function improved in four patients. Visual function was unchanged in one patient, lacking visual disturbancies pre-op. Complication developed in one patient.
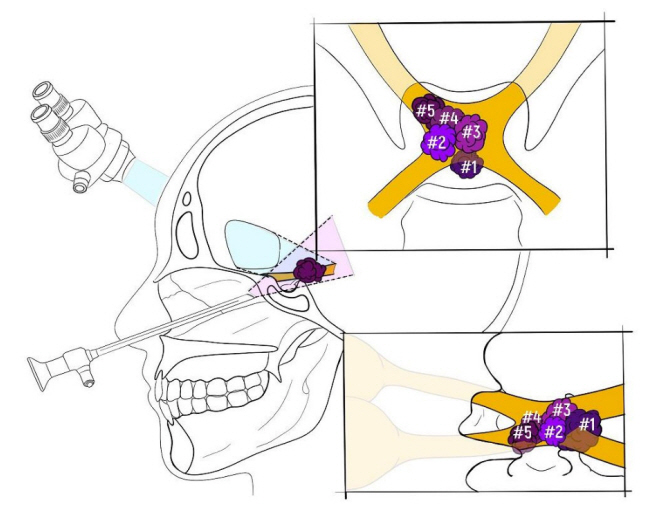
Conclusions
Optochiasmatic cavernomas are encountered extremely rare. Despite the use of contemporary diagnostic options, differential diagnosis remains challenging. Full diagnostic work-up is mandatory. After the diagnosis is made, surgical treatment should be considered first. Total microsurgical or endoscopic transsphenoidal removal of the optochiasmatic cavernoma is a relatively safe and effective treatment method facilitating improvement of visual function.
Figure
Cited by 1 articles
-
Giant cerebellar cavernous malformation in children: A case report and literature review
Olim Zaribovich Akramov, Lilia Aleksandrovna Nazarova, Fuat Mukadasavoch Kurbanov, Sukhrob Abdurashibovich Tashmatov, Ikrom Ismatovich Rakhimov, Odilkhon Ayubxanovich Usmankhanov, Bipin Chaurasia
J Cerebrovasc Endovasc Neurosurg. 2024;26(3):304-310. doi: 10.7461/jcen.2024.E2023.04.006.
Reference
-
1. Alam S, Chaurasia BK, Shalike N, Uddin AN, Chowdhury D, Khan AH, et al. Surgical management of clinoidal meningiomas: 10 cases analysis. Neuroimmunology and Neuroinflammation. 2018; May. 5:21.2. Alam S, Ferini G, Muhammad N, Ahmed N, Wakil AN, Islam KM, et al. Skull base approaches for tuberculum sellae meningiomas: Institutional experience in a series of 34 patients. Life (Basel). 2022; Mar. 12(4):492.3. Algoet M, Van Dyck-Lippens PJ, Casselman J, Sirimsi S, Fletcher CDM, Van Den Berghe I, et al. Intracanal optic nerve cavernous hemangioma: A case report and review of the literature. World Neurosurg. 2019; Jun. 126:428–33.4. Benedičič M, Bošnjak R. Intraoperative monitoring of the visual function using cortical potentials after electrical epidural stimulation of the optic nerve. Acta Neurochir (Wien). 2011; Oct. 153(10):1919–27.5. Bosnjak R, Benedicic M. Direct epidural electrical stimulation of the optic nerve: A new method for intraoperative assessment of function. J Neurosurg. 2008; Oct. 109(4):647–53.6. Brown AP, Thompson BG, Spetzler RF. The two-point method: Evaluating brain stem lesions. Barrow Q. 1996; 12:20–4.7. Cerase A, Franceschini R, Battistini S, Maria Vallone I, Penco S, Venturi C. Cavernous malformation of the optic nerve mimicking optic neuritis. J Neuroophthalmol. 2010; Jun. 30(2):126–31.8. Chaurasia B. Extended endonasal endoscopic approach for the resection of craniopharyngioma-an analysis of 40 cases. EC Neurology. 2018; 10:981–90.9. Chen Y, Tu Y, Chen B, Shi J, Yu B, Wu W. Endoscopic transnasal removal of cavernous hemangiomas of the optic canal. Am J Ophthalmol. 2017; Jan. 173:1–6.10. Curran JG, O’Connor E. Imaging of craniopharyngioma. Childs Nerv Syst. 2005; Aug. 21(8-9):635–9.11. Garg K, Chaurasia B, Pahwa B, Arnaout MM, Zenonos GA, Piloto OL, et al. Geographic Disparities in the proliferation of minimally invasive approaches for sellar/parasellar lesions. World Neurosurgery. 2022; Dec. 168:e162–77.12. Gonçalves VM, Gonçalves V. Surgical management of cavernous malformation of the optic nerve with canalicular extension. Surg Neurol Int. 2014; Oct. 5(Suppl 12):S455–60.13. Meng X, Feng X, Wan J. Endoscopic endonasal transsphenoidal approach for the removal of optochiasmatic cavernoma: Case report and literature review. World Neurosurg. 2017; Oct. 106:1053.14. Murai Y, Adachi K, Koketsu K, Teramoto A. Indocyanine green videoangiography of optic cavernous angioma –case report–. Neurol Med Chir (Tokyo). 2011; 51(4):296–8.15. Muta D, Nishi T, Koga K, Yamashiro S, Fujioka S, Kuratsu J. Cavernous malformation of the optic chiasm: Case report. Br J Neurosurg. 2006; Oct. 20(5):312–5.16. Nawar RN, AbdelMannan D, Selman WR, Arafah BM. Pituitary tumor apoplexy: A review. J Intensive Care Med. 2008; Mar-Apr. 23(2):75–90.17. Ozer E, Kalemci O, Yücesoy K, Canda S. Optochiasmatic cavernous angioma: Unexpected diagnosis. Case report. Neurol Med Chir (Tokyo). 2007; Mar. 47(3):128–31.18. San-Juan D, Escanio Cortés M, Tena-Suck M, Orozco Garduño AJ, López Pizano JA, Villanueva Domínguez J, et al. Neurophysiological intraoperative monitoring during an optic nerve schwannoma removal. J Clin Monit Comput. 2017; Oct. 31(5):1059–64.19. Sbeih I, Darwazeh R, Shehadeh M, Nisah M, Sbeih A, Abu-Farsakh H, et al. Anterior interhemispheric approach for microsurgical resection of an optic chiasm cavernoma. Interdiscip Neurosurg. 2020; 21:100766.20. Srinivasan VM, Koester SW, Wang MS, Rahmani R, Ma KL, Catapano JS, et al. Cavernous malformations of the optic nerve and optic pathway: A case series and systematic review of the literature. Oper Neurosurg (Hagerstown). 2021; Oct. 21(5):291–302.21. Tan T, Tee JW, Trost N, McKelvie P, Wang YY. Anterior visual pathway cavernous malformations. J Clin Neurosci. 2015; Feb. 22(2):258–67.22. Venkataramana NK, Rao SA V, Arun LN, Krishna C. Cavernous malformation of the optic chiasm: Neuro-endoscopic removal. Asian J Neurosurg. 2016; Jan-Mar. 11(1):68–9.23. Zoia C, Bongetta D, Dorelli G, Luzzi S, Maestro M Del, Galzio RJ. Transnasal endoscopic removal of a retrochiasmatic cavernoma: A case report and review of literature. Surg Neurol Int. 2019; May. 10:76.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Portal cavernoma cholangiopathy: Update and recommendations on diagnosis and management
- Feasibility of laparoscopic cholecystectomy for symptomatic gallstone disease with portal cavernoma: Can prior portal vein decompression be avoided?
- Giant cerebellar cavernous malformation in children: A case report and literature review
- A Case of Spinal Cord Cavernoma Mimicking Transverse Myelitis
- Surgical Treatment of Intramedullary Spinal Cord Cavernous Malformation