Korean Circ J.
2023 Dec;53(12):843-854. 10.4070/kcj.2023.0159.
Association Between Body Mass Index and Clinical Outcomes According to Diabetes in Patients Who Underwent Percutaneous Coronary Intervention
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea
- 2Division of Cardiology, Department of Internal Medicine, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea
- 3Division of Cardiology, Department of Internal Medicine, CHA Bundang Medical Center, CHA University College of Medicine, Seongnam, Korea
- KMID: 2548792
- DOI: http://doi.org/10.4070/kcj.2023.0159
Abstract
- Background and Objectives
We evaluated the effect of diabetes on the relationship between body mass index (BMI) and clinical outcomes in patients following percutaneous coronary intervention (PCI) with drug-eluting stent implantation.
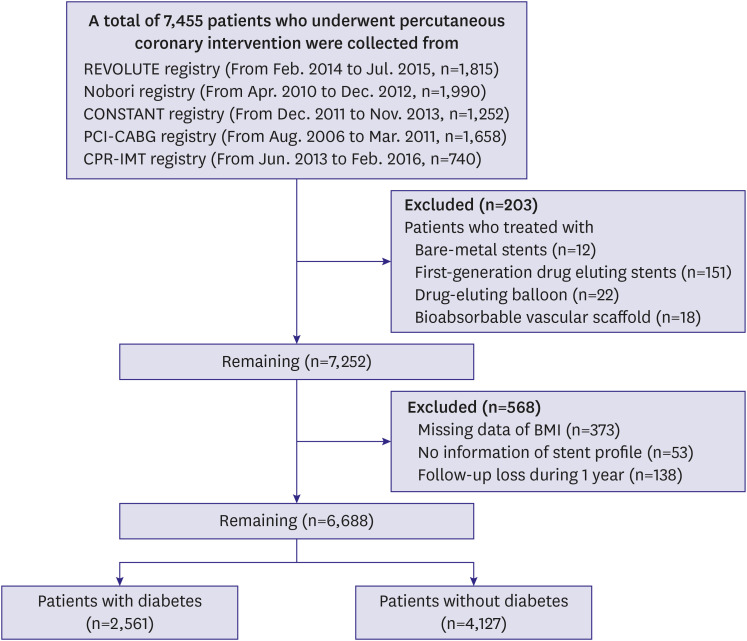
Methods
A total of 6,688 patients who underwent PCI were selected from five different registries led by Korean Multicenter Angioplasty Team. They were categorized according to their BMI into the following groups: underweight (<18.5 kg/m 2 ), normal weight (18.5–24.9 kg/m 2 ), overweight to obese (≥25.0 kg/m 2 ). Major adverse cardiac and cerebrovascular events (MACCE), defined as a composite of death, nonfatal myocardial infarction, stroke, and target-vessel revascularization, were compared according to the BMI categories (underweight, normal and overweight to obese group) and diabetic status. All subjects completed 1-year follow-up.
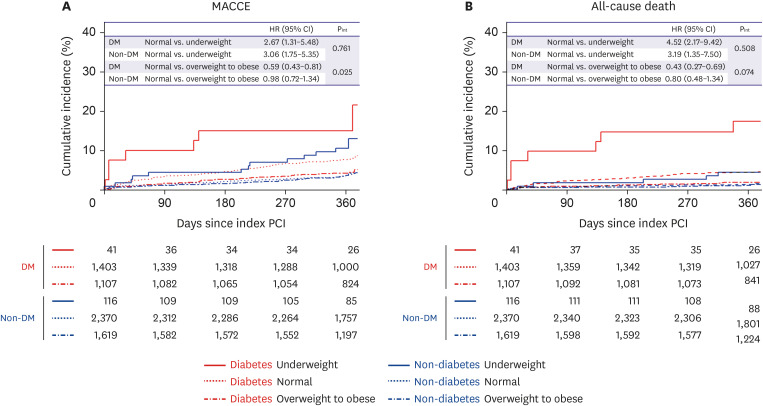
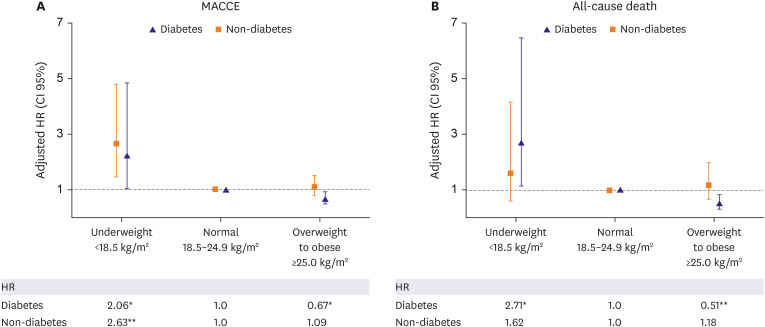
Results
Among the 6,688 patients, 2,561 (38%) had diabetes. The underweight group compared to normal weight group had higher 1-year MACCE rate in both non-diabetic (adjusted hazard ratio [HR], 2.24; 95% confidence interval [CI], 1.04–4.84; p=0.039) and diabetic patients (adjusted HR, 2.86; 95% CI, 1.61–5.07; p<0.001). The overweight to obese group had a lower MACCE rate than the normal weight group in diabetic patients (adjusted HR, 0.67 [0.49–0.93]) but not in non-diabetic patients (adjusted HR, 1.06 [0.77–1.46]), with a significant interaction (p-interaction=0.025).
Conclusions
Between the underweight and normal weight groups, the association between the BMI and clinical outcomes was consistent regardless of the presence of diabetes. However, better outcomes in overweight to obese over normal weight were observed only in diabetic patients. These results suggest that the association between BMI and clinical outcomes may differ according to the diabetic status.
Figure
Reference
-
1. Wilson PW, D’Agostino RB, Sullivan L, Parise H, Kannel WB. Overweight and obesity as determinants of cardiovascular risk: the Framingham experience. Arch Intern Med. 2002; 162:1867–1872. PMID: 12196085.2. Vazquez G, Duval S, Jacobs DR Jr, Silventoinen K. Comparison of body mass index, waist circumference, and waist/hip ratio in predicting incident diabetes: a meta-analysis. Epidemiol Rev. 2007; 29:115–128. PMID: 17494056.3. Holroyd EW, Sirker A, Kwok CS, et al. The relationship of body mass index to percutaneous coronary intervention outcomes: does the obesity paradox exist in contemporary percutaneous coronary intervention cohorts? Insights from the British Cardiovascular Intervention Society Registry. JACC Cardiovasc Interv. 2017; 10:1283–1292. PMID: 28683933.4. Kaneko H, Yajima J, Oikawa Y, et al. Obesity paradox in Japanese patients after percutaneous coronary intervention: an observation cohort study. J Cardiol. 2013; 62:18–24. PMID: 23706354.5. Preis SR, Hwang SJ, Coady S, et al. Trends in all-cause and cardiovascular disease mortality among women and men with and without diabetes mellitus in the Framingham Heart Study, 1950 to 2005. Circulation. 2009; 119:1728–1735. PMID: 19307472.6. Kim YH, Her AY, Jeong MH, et al. Outcomes between prediabetes and type 2 diabetes mellitus in older adults with acute myocardial infarction in the era of newer-generation drug-eluting stents: a retrospective observational study. BMC Geriatr. 2021; 21:653. PMID: 34798819.7. Lee YJ, Cho JY, You SC, et al. Moderate-intensity statin with ezetimibe vs. high-intensity statin in patients with diabetes and atherosclerotic cardiovascular disease in the RACING trial. Eur Heart J. 2023; 44:972–983. PMID: 36529993.8. Kim BG, Hong SJ, Kim BK, et al. Association between body mass index and clinical outcomes after new-generation drug-eluting stent implantation: Korean multi-center registry data. Atherosclerosis. 2018; 277:155–162. PMID: 30216914.9. Cutlip DE, Windecker S, Mehran R, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007; 115:2344–2351. PMID: 17470709.10. Kim SH, Després JP, Koh KK. Obesity and cardiovascular disease: friend or foe? Eur Heart J. 2016; 37:3560–3568. PMID: 26685971.11. Powell-Wiley TM, Poirier P, Burke LE, et al. Obesity and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2021; 143:e984–1010. PMID: 33882682.12. Finucane MM, Stevens GA, Cowan MJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet. 2011; 377:557–567. PMID: 21295846.13. Folsom AR, Stevens J, Schreiner PJ, McGovern PG. Atherosclerosis Risk in Communities Study Investigators. Body mass index, waist/hip ratio, and coronary heart disease incidence in African Americans and whites. Am J Epidemiol. 1998; 148:1187–1194. PMID: 9867265.14. Abdelaal M, le Roux CW, Docherty NG. Morbidity and mortality associated with obesity. Ann Transl Med. 2017; 5:161. PMID: 28480197.15. Adams KF, Schatzkin A, Harris TB, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006; 355:763–778. PMID: 16926275.16. Yoon KH, Lee JH, Kim JW, et al. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006; 368:1681–1688. PMID: 17098087.17. Yang YS, Han BD, Han K, et al. Obesity fact sheet in Korea, 2021: trends in obesity prevalence and obesity-related comorbidity incidence stratified by age from 2009 to 2019. J Obes Metab Syndr. 2022; 31:169–177. PMID: 35770450.18. Neeland IJ, Das SR, Simon DN, et al. The obesity paradox, extreme obesity, and long-term outcomes in older adults with ST-segment elevation myocardial infarction: results from the NCDR. Eur Heart J Qual Care Clin Outcomes. 2017; 3:183–191. PMID: 28838094.19. Das SR, Alexander KP, Chen AY, et al. Impact of body weight and extreme obesity on the presentation, treatment, and in-hospital outcomes of 50,149 patients with ST-Segment elevation myocardial infarction results from the NCDR (National Cardiovascular Data Registry). J Am Coll Cardiol. 2011; 58:2642–2650. PMID: 22152950.20. Ali ZA, Maehara A, Généreux P, et al. Optical coherence tomography compared with intravascular ultrasound and with angiography to guide coronary stent implantation (ILUMIEN III: OPTIMIZE PCI): a randomised controlled trial. Lancet. 2016; 388:2618–2628. PMID: 27806900.21. Hossain P, Kawar B, El Nahas M. Obesity and diabetes in the developing world--a growing challenge. N Engl J Med. 2007; 356:213–215. PMID: 17229948.22. Hartemink N, Boshuizen HC, Nagelkerke NJ, Jacobs MA, van Houwelingen HC. Combining risk estimates from observational studies with different exposure cutpoints: a meta-analysis on body mass index and diabetes type 2. Am J Epidemiol. 2006; 163:1042–1052. PMID: 16611666.23. Pagidipati NJ, Zheng Y, Green JB, et al. Association of obesity with cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease: Insights from TECOS. Am Heart J. 2020; 219:47–57. PMID: 31707324.24. Kwon Y, Kim HJ, Park S, Park YG, Cho KH. Body mass index-related mortality in patients with type 2 diabetes and heterogeneity in obesity paradox studies: a dose-response meta-analysis. PLoS One. 2017; 12:e0168247. PMID: 28046128.25. Salehidoost R, Mansouri A, Amini M, Yamini SA, Aminorroaya A. Body mass index and the all-cause mortality rate in patients with type 2 diabetes mellitus. Acta Diabetol. 2018; 55:569–577. PMID: 29546575.26. Dangas GD, Maehara A, Evrard SM, et al. Coronary artery calcification is inversely related to body morphology in patients with significant coronary artery disease: a three-dimensional intravascular ultrasound study. Eur Heart J Cardiovasc Imaging. 2014; 15:201–209. PMID: 23904334.27. Giustino G, Dangas GD. Surgical revascularization versus percutaneous coronary intervention and optimal medical therapy in diabetic patients with multi-vessel coronary artery disease. Prog Cardiovasc Dis. 2015; 58:306–315. PMID: 26255239.28. Horwich TB, Fonarow GC, Hamilton MA, MacLellan WR, Woo MA, Tillisch JH. The relationship between obesity and mortality in patients with heart failure. J Am Coll Cardiol. 2001; 38:789–795. PMID: 11527635.29. Steinberg BA, Cannon CP, Hernandez AF, Pan W, Peterson ED, Fonarow GC. Medical therapies and invasive treatments for coronary artery disease by body mass: the “obesity paradox” in the Get With The Guidelines database. Am J Cardiol. 2007; 100:1331–1335. PMID: 17950785.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diabetes Mellitus and Coronary Angiography
- Risk Factors of Restenosis after Percutaneous Coronary Intervention in Type 2 Diabetes Mellitus Patients
- Incidence, Predictors, and Clinical Outcomes of New-Onset Diabetes Mellitus after Percutaneous Coronary Intervention with Drug-Eluting Stent
- A Case of Right Coronary Artery Hematoma Detected by Echocardiography after Percutaneous Coronary Intervention
- Recent Advances in Percutaneous Coronary Intervention in Coronary Artery Disease