J Yeungnam Med Sci.
2023 Nov;40(Suppl):S125-S128. 10.12701/jyms.2023.00360.
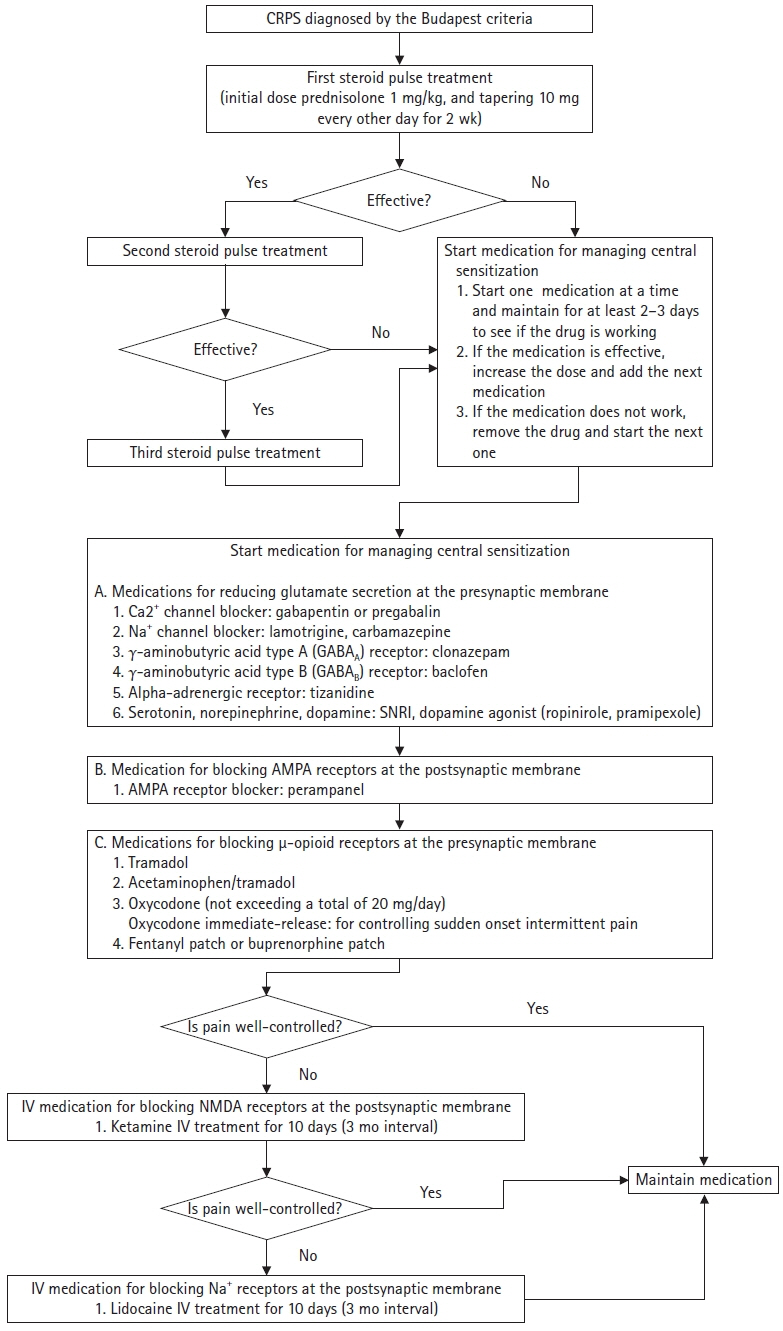
Algorithm for multimodal medication therapy in patients with complex regional pain syndrome
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Yeungnam University College of Medicine, Daegu, Korea
- 2Department of Rehabilitation Medicine, Daegu Fatima Hospital, Daegu, Korea
- KMID: 2548354
- DOI: http://doi.org/10.12701/jyms.2023.00360
Abstract
- Complex regional pain syndrome (CRPS), previously known as reflex sympathetic dystrophy and causalgia, is a clinical entity characterized by classic neuropathic pain, autonomic involvement, motor symptoms, and trophic changes in the skin, nails, and hair. Although various therapeutic modalities are used to control CRPS-related pain, severe pain due to CRPS often persists and progresses to the chronic phase. In this study, we constructed an algorithm for multimodal medication therapy for CRPS based on the established pathology of CRPS. Oral steroid pulse therapy is recommended for initial pain management in patients with CRPS. Oral steroid therapy can reduce peripheral and central neuroinflammation, contributing to the development of neuropathic pain during the acute and chronic phases. If steroid pulse therapy offers poor relief or is ineffective, treatment to control central sensitization in the chronic phase should be initiated. If pain persists despite all drug adjustments, ketamine with midazolam 2 mg before and after ketamine injection can be administered intravenously to inhibit the N-methyl D-aspartate receptor. If this treatment fails to achieve sufficient efficacy, intravenous lidocaine can be administered for 2 weeks. We hope that our proposed drug treatment algorithm to control CRPS pain will help clinicians appropriately treat patients with CRPS. Further clinical studies assessing patients with CRPS are warranted to establish this treatment algorithm in clinical practice.
Figure
Reference
-
References
1. Kingery WS. A critical review of controlled clinical trials for peripheral neuropathic pain and complex regional pain syndromes. Pain. 1997; 73:123–39.
Article2. Park GY, Park JH, Lee B, Im S, Min JH. Comparison of short-term effect between bisphosphonate and steroid therapy in hemiplegic patients with CRPS type I. J Korean Acad Rehab Med. 2009; 33:103–7.3. Ji RR, Nackley A, Huh Y, Terrando N, Maixner W. Neuroinflammation and central sensitization in chronic and widespread pain. Anesthesiology. 2018; 129:343–66.
Article4. Tao YX. AMPA receptor trafficking in inflammation-induced dorsal horn central sensitization. Neurosci Bull. 2012; 28:111–20.
Article5. Chang MC, Park D. Effectiveness of perampanel in managing chronic pain caused by the complex regional pain syndrome: a case report. Medicine (Baltimore). 2021; 100:e27791.6. Gustin SM, Schwarz A, Birbaumer N, Sines N, Schmidt AC, Veit R, et al. NMDA-receptor antagonist and morphine decrease CRPS-pain and cerebral pain representation. Pain. 2010; 151:69–76.
Article7. Patel R, Dickenson AH. Mechanisms of the gabapentinoids and α 2 δ-1 calcium channel subunit in neuropathic pain. Pharmacol Res Perspect. 2016; 4:e00205.
Article8. Colombo G, Agabio R, Lobina C, Reali R, Gessa GL. Involvement of GABA(A) and GABA(B) receptors in the mediation of discriminative stimulus effects of gamma-hydroxybutyric acid. Physiol Behav. 1998; 64:293–302.
Article9. Takayanagi I, Konno F, Ishii C, Takemasa T, Yanagida Y, Shimizu M, et al. Actions of tizanidine on alpha 1- and alpha 2-adrenoceptors in the peripheral tissues. Gen Pharmacol. 1984; 15:239–41.10. Haddjeri N, Blier P, de Montigny C. Effect of the alpha-2 adrenoceptor antagonist mirtazapine on the 5-hydroxytryptamine system in the rat brain. J Pharmacol Exp Ther. 1996; 277:861–71.11. Brodie MJ. Sodium channel blockers in the treatment of epilepsy. CNS Drugs. 2017; 31:527–34.
Article12. Zarkowski PA. Relative prevalence of 10 types of pharmacodynamic interactions in psychiatric treatment. Int J Psychiatry Med. 2020; 55:82–104.
Article13. Park D. Pramipexole-induced limb dystonia and its associated complex regional pain syndrome in idiopathic Parkinson's disease: a case report. Medicine (Baltimore). 2017; 96:e7530.14. Bymaster FP, Dreshfield-Ahmad LJ, Threlkeld PG, Shaw JL, Thompson L, Nelson DL, et al. Comparative affinity of duloxetine and venlafaxine for serotonin and norepinephrine transporters in vitro and in vivo, human serotonin receptor subtypes, and other neuronal receptors. Neuropsychopharmacology. 2001; 25:871–80.
Article15. Chitneni A, Patil A, Dalal S, Ghorayeb JH, Pham YN, Grigoropoulos G. Use of ketamine infusions for treatment of complex regional pain syndrome: a systematic review. Cureus. 2021; 13:e18910.
Article16. Schwartzman RJ, Patel M, Grothusen JR, Alexander GM. Efficacy of 5-day continuous lidocaine infusion for the treatment of refractory complex regional pain syndrome. Pain Med. 2009; 10:401–12.
Article17. Carroll I, Clark JD, Mackey S. Sympathetic block with botulinum toxin to treat complex regional pain syndrome. Ann Neurol. 2009; 65:348–51.
Article18. Sahin F, Yilmaz F, Kotevoglu N, Kuran B. Efficacy of salmon calcitonin in complex regional pain syndrome (type 1) in addition to physical therapy. Clin Rheumatol. 2006; 25:143–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Contralateral Mirror Image Spreading in Post-Stroke Complex Regional Pain Syndrome
- Complex Regional Pain Syndrome
- Complex Regional Pain Syndrome Type I after Stroke
- The Effect of Epidural Ketamine in Complex Regional Pain Syndrome Occuring after Lumbar Epidural Block
- Spinal Cord Stimulation in Pain Management: A Review