Restor Dent Endod.
2022 Nov;47(4):e41. 10.5395/rde.2022.47.e41.
Evaluation of blood clot, plateletrich plasma, and platelet-rich fibrin– mediated regenerative endodontic procedures in teeth with periapical pathology: a CBCT study
- Affiliations
-
- 1Department of Conservative Dentistry and Endodontics, Dr. R. Ahmed Dental College and Hospital, Kolkata, India
- KMID: 2548145
- DOI: http://doi.org/10.5395/rde.2022.47.e41
Abstract
Objectives
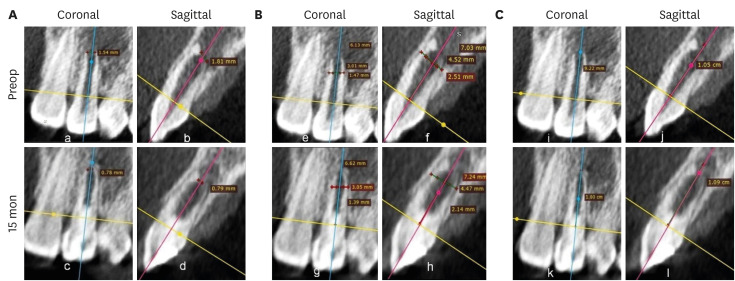
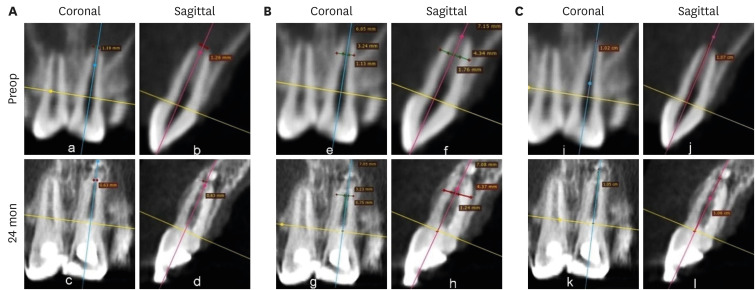
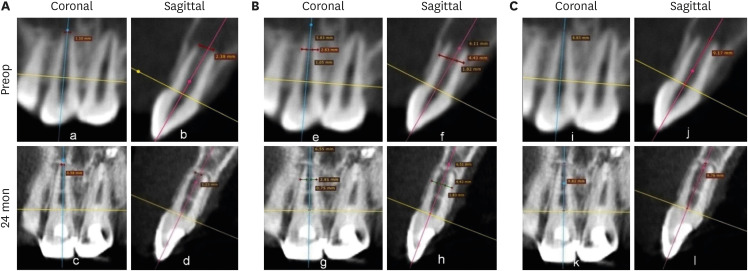
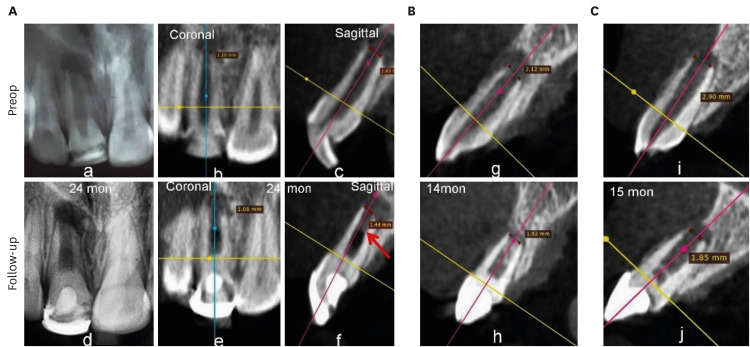
This study compared the clinical and radiological outcomes of regenerative endodontic procedures (REPs) using blood clots (BCs), platelet-rich plasma (PRP), and platelet-rich fibrin (PRF) through intraoral periapical radiography (IOPAR) and cone-beam computed tomography (CBCT).
Materials and Methods
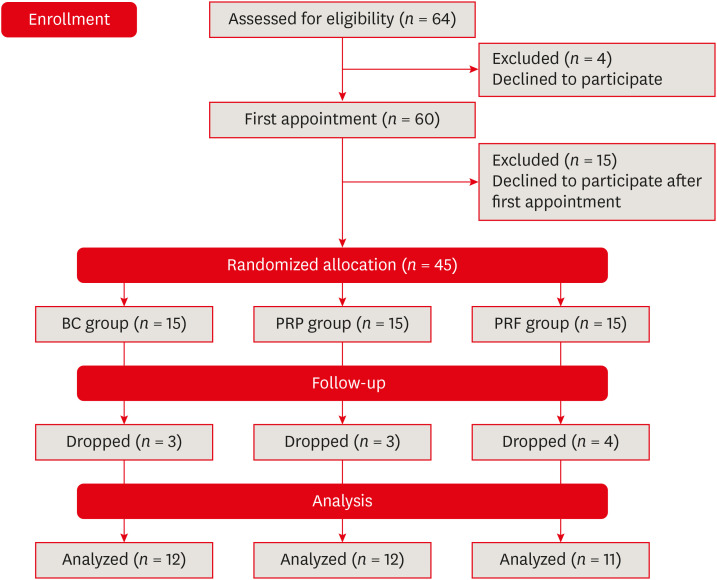
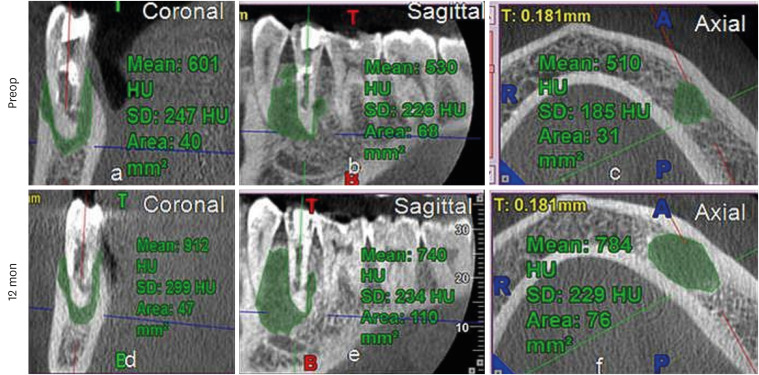
Forty-five single-rooted necrotic teeth with periapical pathology were randomly allocated to receive BC, PRP, or PRF as an individual scaffold. Outcomes were evaluated in 35 teeth in 23 patients with a follow-up period of 12–24 months through qualitative IOPAR scoring and quantitative CBCT measurements. Healing of periapical lesions and in immature teeth, changes in the apical foramen diameter (AFD), root wall thickness (RWT), and root length (RL) were assessed. A p value less than 0.05 was considered to indicate statistical significance.
Results
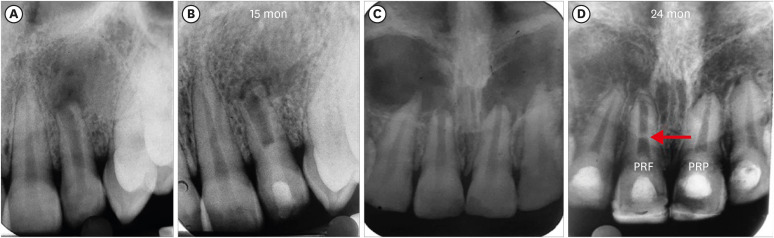
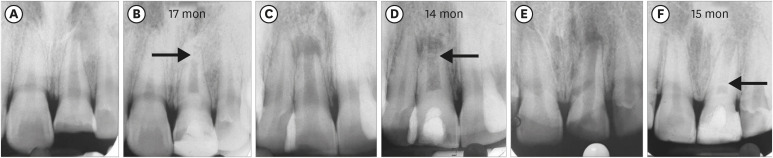
All teeth were asymptomatic except 1 in the PRP group. Periapical lesion healing was seen in all except 2 teeth in the BC group and 3 in the PRP group. Both IOPAR and CBCT revealed no significant differences in bone healing or changes in AFD, RWT, and RL among the 3 groups. A positive pulp sensibility response to the cold test was seen in 2 teeth in the BC group, but none to the electric pulp test. Intracanal calcification (ICC) was evident in more teeth in the BC group than in the PRP and PRF groups, and was also significantly higher in immature teeth.
Conclusions
Our results revealed that BC, PRP, and PRF have similar potential as scaffolds in REPs, and ICC may be a concern for long-term outcomes.
Figure
Reference
-
1. Ulusoy AT, Turedi I, Cimen M, Cehreli ZC. Evaluation of blood clot, platelet-rich plasma, plateletrich fibrin, and platelet pellet as scaffolds in regenerative endodontic treatment: a prospective randomized trial. J Endod. 2019; 45:560–566. PMID: 30935618.
Article2. ElSheshtawy AS, Nazzal H, El Shahawy OI, El Baz AA, Ismail SM, Kang J, Ezzat KM. The effect of platelet-rich plasma as a scaffold in regeneration/revitalization endodontics of immature permanent teeth assessed using 2-dimensional radiographs and cone beam computed tomography: a randomized controlled trial. Int Endod J. 2020; 53:905–921. PMID: 32249441.
Article3. Egusa H, Sonoyama W, Nishimura M, Atsuta I, Akiyama K. Stem cells in dentistry--part I: stem cell sources. J Prosthodont Res. 2012; 56:151–165. PMID: 22796367.4. Wingard JR, Demetri GD. Clinical applications of cytokines and growth factors. New York, NY: Springer;1999.5. Zhao S, Sloan AJ, Murray PE, Lumley PJ, Smith AJ. Ultrastructural localisation of TGF-β exposure in dentine by chemical treatment. Histochem J. 2000; 32:489–494. PMID: 11095074.6. O’Brien FJ. Biomaterials & scaffolds for tissue engineering. Mater Today. 2011; 14:88–95.
Article7. American Association of Endodontists. Clinical considerations for a regenerative procedure. updated April 1, 2018. cited June 9, 2021. Available from: https://www.aae.org.8. Narang I, Mittal N, Mishra N. A comparative evaluation of the blood clot, platelet-rich plasma, and platelet-rich fibrin in regeneration of necrotic immature permanent teeth: a clinical study. Contemp Clin Dent. 2015; 6:63–68. PMID: 25684914.
Article9. Shivashankar VY, Johns DA, Maroli RK, Sekar M, Chandrasekaran R, Karthikeyan S, Renganathan SK. Comparison of the effect of PRP, PRF and induced bleeding in the revascularization of teeth with necrotic pulp and open apex: a triple blind randomized clinical trial. J Clin Diagn Res. 2017; 11:ZC34–ZC39.
Article10. Murray PE. Platelet-rich plasma and platelet-rich fibrin can induce apical closure more frequently than blood-clot revascularization for the regeneration of immature permanent teeth: a meta-analysis of clinical efficacy. Front Bioeng Biotechnol. 2018; 6:139. PMID: 30364277.
Article11. Prabhakar AR, Rani NS, Yavagal C. Revascularization of immature necrotic teeth with platelet- rich fibrin and blood clot. Int J Oral Health Sci. 2016; 6:4–10.
Article12. Lv H, Chen Y, Cai Z, Lei L, Zhang M, Zhou R, Huang X. The efficacy of platelet-rich fibrin as a scaffold in regenerative endodontic treatment: a retrospective controlled cohort study. BMC Oral Health. 2018; 18:139. PMID: 30103724.
Article13. Bezgin T, Yilmaz AD, Celik BN, Kolsuz ME, Sonmez H. Efficacy of platelet-rich plasma as a scaffold in regenerative endodontic treatment. J Endod. 2015; 41:36–44. PMID: 25459571.
Article14. Turky M, Kataia MA, Ali MMM, Hassan RE. Revascularization induced maturogenesis of human non-vital immature teeth via platelets- rich plasma (PRP): radiographic study. J Dent Oral Health. 2017; 3:097.15. Rizk HM, Al-Deen MS, Emam AA. Regenerative endodontic treatment of bilateral necrotic immature permanent maxillary central incisors with platelet-rich plasma versus blood clot: a split mouth double-blinded randomized controlled trial. Int J Clin Pediatr Dent. 2019; 12:332–339. PMID: 31866720.
Article16. Rizk HM, Salah Al-Deen MS, Emam AA. Comparative evaluation of platelet rich plasma (PRP) versus platelet rich fibrin (PRF) scaffolds in regenerative endodontic treatment of immature necrotic permanent maxillary central incisors: a double blinded randomized controlled trial. Saudi Dent J. 2020; 32:224–231. PMID: 32647469.
Article17. Adhikari HD, Sujith R, Gupta A, Markandey S. Comparative evaluation of platelet rich plasma and platelet rich fibrin as a scaffold for regenerative endodontic procedure: a clinical study. IOSR J Dent Med Sci. 2021; 20:51–58.18. Alagl A, Bedi S, Hassan K, AlHumaid J. Use of platelet-rich plasma for regeneration in non-vital immature permanent teeth: clinical and cone-beam computed tomography evaluation. J Int Med Res. 2017; 45:583–593. PMID: 28415948.
Article19. Farhad Mollashahi N, Saberi E, Karkehabadi H. Evaluation of cytotoxic effects of various endodontic irrigation solutions on the survival of stem cell of human apical papilla. Iran Endod J. 2016; 11:293–297. PMID: 27790258.20. Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 101:e37–e44. PMID: 16504849.
Article21. Amable PR, Carias RB, Teixeira MV, da Cruz Pacheco I, Corrêa do Amaral RJ, Granjeiro JM, Borojevic R. Platelet-rich plasma preparation for regenerative medicine: optimization and quantification of cytokines and growth factors. Stem Cell Res Ther. 2013; 4:67. PMID: 23759113.
Article22. Tanomaru-FIlho M, Jorge ÉG, Guerreiro-Tanomaru JM, Reis JM, Spin-Neto R, Gonçalves M. Two- and tridimensional analysis of periapical repair after endodontic surgery. Clin Oral Investig. 2015; 19:17–25.
Article23. Sherrard JF, Rossouw PE, Benson BW, Carrillo R, Buschang PH. Accuracy and reliability of tooth and root lengths measured on cone-beam computed tomographs. Am J Orthod Dentofacial Orthop. 2010; 137:S100–S108. PMID: 20381750.
Article24. Ashwinirani SR, Suragimath G, Jaishankar HP, Kulkarni P, Bijjaragi SC, Sangle VA. Comparison of diagnostic accuracy of conventional intraoral periapical and direct digital radiographs in detecting interdental bone loss. J Clin Diagn Res. 2015; 9:ZC35–ZC38.25. Kahler B, Kahler SL, Lin LM. Revascularization-associated Intracanal calcification: a case report with an 8-year review. J Endod. 2018; 44:1792–1795. PMID: 30487078.
Article26. Lin J, Zeng Q, Wei X, Zhao W, Cui M, Gu J, Lu J, Yang M, Ling J. Regenerative endodontics versus apexification in immature permanent teeth with apical periodontitis: a prospective randomized controlled study. J Endod. 2017; 43:1821–1827. PMID: 28864219.
Article27. Torabinejad M, Turman M. Revitalization of tooth with necrotic pulp and open apex by using platelet-rich plasma: a case report. J Endod. 2011; 37:265–268. PMID: 21238815.
Article28. Huang GT. Dental pulp and dentin tissue engineering and regeneration: advancement and challenge. Front Biosci (Elite Ed). 2011; 3:788–800. PMID: 21196351.
Article29. Andreasen FM, Kahler B. Pulpal response after acute dental injury in the permanent dentition: clinical implications-a review. J Endod. 2015; 41:299–308. PMID: 25601716.
Article30. Song M, Cao Y, Shin SJ, Shon WJ, Chugal N, Kim RH, Kim E, Kang MK. Revascularization- associated intracanal calcification: assessment of prevalence and contributing factors. J Endod. 2017; 43:2025–2033. PMID: 28965774.
Article31. Adhikari HD, Gupta A. Report of a case of platelet-rich fibrin-mediated revascularization of immature 12 with histopathological evaluation. J Conserv Dent. 2018; 21:691–695. PMID: 30546220.
Article32. Austah O, Joon R, Fath WM, Chrepa V, Diogenes A, Ezeldeen M, Couve E, Ruparel NB. Comprehensive characterization of 2 immature teeth treated with regenerative endodontic procedures. J Endod. 2018; 44:1802–1811. PMID: 30477666.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Platelet rich fibrin - a novel acumen into regenerative endodontic therapy
- The use of platelet rich plasma in the treatment of immature tooth with periapical lesion: a case report
- Regenerating the Pulp–Dentine Complex Using Autologous Platelet Concentrates: A Critical Appraisal of the Current Histological Evidence
- Fibrin Clot Delivery System for Meniscal Repair
- Effect of Platelet-rich Plasma on Burn Wounds according to Time of Application: An Experimental Study on Rats