Clin Endosc.
2023 Nov;56(6):726-734. 10.5946/ce.2023.059.
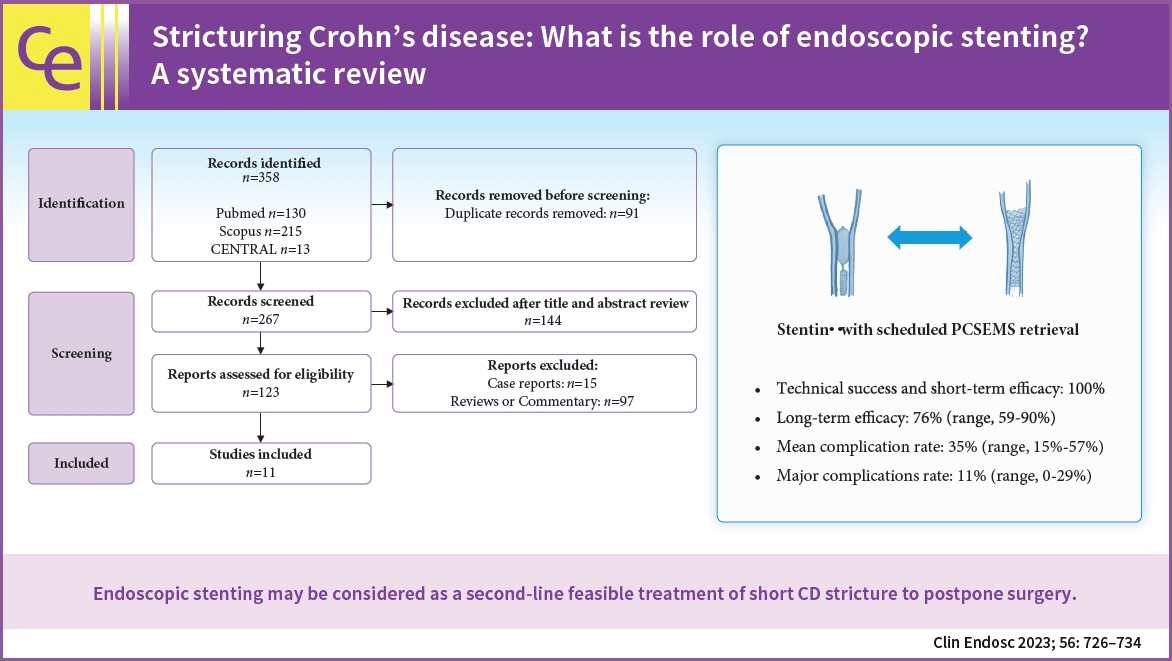
Stricturing Crohn's disease: what is the role of endoscopic stenting? A systematic review
- KMID: 2547892
- DOI: http://doi.org/10.5946/ce.2023.059
Abstract
- Background/Aims
Endoscopic stenting for stricturing Crohn's disease (CD) is an emerging treatment that achieves more persistent dilatation of the stricture over time than endoscopic balloon dilatation (EBD). We aimed to explore the efficacy and safety of stenting for the treatment of CD strictures.
Methods
A systematic electronic literature search was performed (PROSPERO; no. CRD42022308033). The primary outcomes were technical success, efficacy, complication rate, and the need for further interventions due to reobstruction. The outcomes of partially covered self-expanding metal stents (PCSEMS) with scheduled retrieval after seven days were also analyzed.
Results
Eleven eligible studies were included in the review. Overall, 173 patients with CD were included in this study. Mean percentage of technical success was 95% (range, 80%–100%), short-term efficacy was 100% in all studies, and long-term efficacy was 56% (range, 25%–90%). In patients with a scheduled PCSEMS retrieval, the long-term efficacy was 76% (range, 59%–90%), the mean complication rate was 35% (range, 15%–57%), and the major complication rate was 11% (range, 0%–29%).
Conclusions
Endoscopic stenting with scheduled PCSEMS retrieval may be considered a feasible second-line treatment for short CD strictures to postpone surgery. However, larger head-to-head prospective studies are needed to understand the role of stenting as an alternative or additional treatment to EBD in CD.
Figure
Reference
-
1. Cosnes J, Gower-Rousseau C, Seksik P, et al. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011; 140:1785–1794.
Article2. Speca S, Giusti I, Rieder F, et al. Cellular and molecular mechanisms of intestinal fibrosis. World J Gastroenterol. 2012; 18:3635–3661.
Article3. Rieder F, Zimmermann EM, Remzi FH, et al. Crohn’s disease complicated by strictures: a systematic review. Gut. 2013; 62:1072–1084.
Article4. Oberhuber G, Stangl PC, Vogelsang H, et al. Significant association of strictures and internal fistula formation in Crohn’s disease. Virchows Arch. 2000; 437:293–297.
Article5. El Ouali S, Click B, Holubar SD, et al. Natural history, diagnosis and treatment approach to fibrostenosing Crohn’s disease. United European Gastroenterol J. 2020; 8:263–270.
Article6. Fukumoto A, Tanaka S, Yamamoto H, et al. Diagnosis and treatment of small-bowel stricture by double balloon endoscopy. Gastrointest Endosc. 2007; 66(3 Suppl):S108–S112.
Article7. Rieder F, Latella G, Magro F, et al. European Crohn’s and Colitis Organisation topical review on prediction, diagnosis and management of fibrostenosing Crohn’s disease. J Crohns Colitis. 2016; 10:873–885.
Article8. Bernell O, Lapidus A, Hellers G. Risk factors for surgery and postoperative recurrence in Crohn’s disease. Ann Surg. 2000; 231:38–45.
Article9. Toh JW, Wang N, Young CJ, et al. Major abdominal and perianal surgery in Crohn’s disease: long-term follow-up of Australian patients with Crohn’s disease. Dis Colon Rectum. 2018; 61:67–76.
Article10. Limketkai BN, Parian AM, Shah ND, et al. Short bowel syndrome and intestinal failure in Crohn’s disease. Inflamm Bowel Dis. 2016; 22:1209–1218.
Article11. Gasche C, Scholmerich J, Brynskov J, et al. A simple classification of Crohn’s disease: report of the Working Party for the World Congresses of Gastroenterology, Vienna 1998. Inflamm Bowel Dis. 2000; 6:8–15.
Article12. Silverberg MS, Satsangi J, Ahmad T, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005; 19 Suppl A:5A–36A.
Article13. Rieder F, Bettenworth D, Ma C, et al. An expert consensus to standardise definitions, diagnosis and treatment targets for anti-fibrotic stricture therapies in Crohn’s disease. Aliment Pharmacol Ther. 2018; 48:347–357.
Article14. Aratari A, Papi C, Leandro G, et al. Early versus late surgery for ileo-caecal Crohn’s disease. Aliment Pharmacol Ther. 2007; 26:1303–1312.
Article15. Latella G, Cocco A, Angelucci E, et al. Clinical course of Crohn's disease first diagnosed at surgery for acute abdomen. Dig Liver Dis. 2009; 41:269–276.
Article16. Golovics PA, Lakatos L, Nagy A, et al. Is early limited surgery associated with a more benign disease course in Crohn’s disease? World J Gastroenterol. 2013; 19:7701–7710.
Article17. Bouhnik Y, Carbonnel F, Laharie D, et al. Efficacy of adalimumab in patients with Crohn’s disease and symptomatic small bowel stricture: a multicentre, prospective, observational cohort (CREOLE) study. Gut. 2018; 67:53–60.
Article18. Bettenworth D, Gustavsson A, Atreja A, et al. A pooled analysis of efficacy, safety, and long-term outcome of endoscopic balloon dilation therapy for patients with stricturing Crohn’s disease. Inflamm Bowel Dis. 2017; 23:133–142.
Article19. Hassan C, Zullo A, De Francesco V, et al. Systematic review: Endoscopic dilatation in Crohn’s disease. Aliment Pharmacol Ther. 2007; 26:1457–1464.
Article20. Morar PS, Faiz O, Warusavitarne J, et al. Systematic review with meta-analysis: endoscopic balloon dilatation for Crohn’s disease strictures. Aliment Pharmacol Ther. 2015; 42:1137–1148.
Article21. Mangiavillano B, Pagano N, Arena M, et al. Role of stenting in gastrointestinal benign and malignant diseases. World J Gastrointest Endosc. 2015; 7:460–480.
Article22. Lamazza A, Fiori E, De Masi E, et al. Self-expanding metal stents for treatment of anastomotic complications after colorectal resection. Endoscopy. 2013; 45:493–495.
Article23. Matsuhashi N, Nakajima A, Suzuki A, et al. Nonsurgical strictureplasty for intestinal strictures in Crohn’s disease: preliminary report of two cases. Gastrointest Endosc. 1997; 45:176–178.
Article24. Rejchrt S, Kopacova M, Brozik J, et al. Biodegradable stents for the treatment of benign stenoses of the small and large intestines. Endoscopy. 2011; 43:911–917.
Article25. Branche J, Attar A, Vernier-Massouille G, et al. Extractible self-expandable metal stent in the treatment of Crohn’s disease anastomotic strictures. Endoscopy. 2012; 44 Suppl 2 UCTN:E325–E326.
Article26. Levine RA, Wasvary H, Kadro O. Endoprosthetic management of refractory ileocolonic anastomotic strictures after resection for Crohn’s disease: report of nine-year follow-up and review of the literature. Inflamm Bowel Dis. 2012; 18:506–512.
Article27. Attar A, Maunoury V, Vahedi K, et al. Safety and efficacy of extractible self-expandable metal stents in the treatment of Crohn’s disease intestinal strictures: a prospective pilot study. Inflamm Bowel Dis. 2012; 18:1849–1854.
Article28. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021; 372:n71.29. National Heart, Lung and Blood Institute. Study quality assessment tools [Internet]. National Heart, Lung and Blood Institute;2021. [cited 2022 Dec 20]. Available from: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.30. Hedenström P, Stotzer PO. Endoscopic treatment of Crohn-related strictures with a self-expandable stent compared with balloon dilation: a prospective, randomised, controlled study. BMJ Open Gastroenterol. 2021; 8:e000612.
Article31. Loras C, Andújar X, Gornals JB, et al. Self-expandable metal stents versus endoscopic balloon dilation for the treatment of strictures in Crohn’s disease (ProtDilat study): an open-label, multicentre, randomised trial. Lancet Gastroenterol Hepatol. 2022; 7:332–341.
Article32. Loras C, Pérez-Roldan F, Gornals JB, et al. Endoscopic treatment with self-expanding metal stents for Crohn’s disease strictures. Aliment Pharmacol Ther. 2012; 36:833–839.
Article33. Karstensen JG, Christensen KR, Brynskov J, et al. Biodegradable stents for the treatment of bowel strictures in Crohn’s disease: technical results and challenges. Endosc Int Open. 2016; 4:E296–E300.
Article34. Das R, Singh R, Din S, et al. Therapeutic resolution of focal, predominantly anastomotic Crohn's disease strictures using removable stents: outcomes from a single-center case series in the United Kingdom. Gastrointest Endosc. 2020; 92:344–352.
Article35. Lamazza A, Fiori E, Carati MV, et al. Self-expandable metal stents for refractory complete rectal obstruction in patients with Crohn's disease. Inflamm Bowel Dis. 2021; 27:e136–e137.36. Attar A, Branche J, Coron E, et al. An anti-migration self-expandable and removable metal stent for Crohn’s disease strictures: a nationwide study from GETAID and SFED. J Crohns Colitis. 2021; 15:521–528.
Article37. van Halsema EE, van Hooft JE, Small AJ, et al. Perforation in colorectal stenting: a meta-analysis and a search for risk factors. Gastrointest Endosc. 2014; 79:970–982.
Article38. Chandan S, Dhindsa BS, Khan SR, et al. Endoscopic stenting in Crohn’s disease-related strictures: a systematic review and meta-analysis of outcomes. Inflamm Bowel Dis. 2023; 29:1145–1152.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Update of endoscopic management of Crohn’s disease strictures
- Efficacy and Safety of Endoscopic Stenting for Crohn's Disease Related Strictures: A Systematic Review and Meta-analysis
- Rates of Early Surgery and Associated Risk Factors in Crohn's Disease
- A Case of Crohn's Disease of the Duodenum
- Inflammation and tissue remodeling contribute to fibrogenesis in stricturing Crohn’s disease: image processing and analysis study