J Korean Med Sci.
2023 Oct;38(42):e317. 10.3346/jkms.2023.38.e317.
The Impact of the COVID-19 Outbreak on Emergency Medical Service: An Analysis of Patient Transportations and Time Intervals
- Affiliations
-
- 1Department of Emergency Medicine, Seoul National University College of Medicine and Seoul National University Hospital, Seoul, Korea
- 2Laboratory of Emergency Medical Services, Biomedical Research Institute, Seoul National University Hospital, Seoul, Korea
- 3119 EMS Division, National Fire Agency, Sejong, Korea
- 4Department of Emergency Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea
- 5Yeongnam 119 Special Rescue Service, National 119 Rescue Headquarter, Daegu, Korea
- KMID: 2547558
- DOI: http://doi.org/10.3346/jkms.2023.38.e317
Abstract
- Background
This study aimed to investigate the impact of the coronavirus disease 2019 (COVID-19) outbreak on the Emergency Medical Service (EMS) system in South Korea. The study focused on the differences in EMS time intervals following the COVID-19 outbreak, particularly for patients with fever.
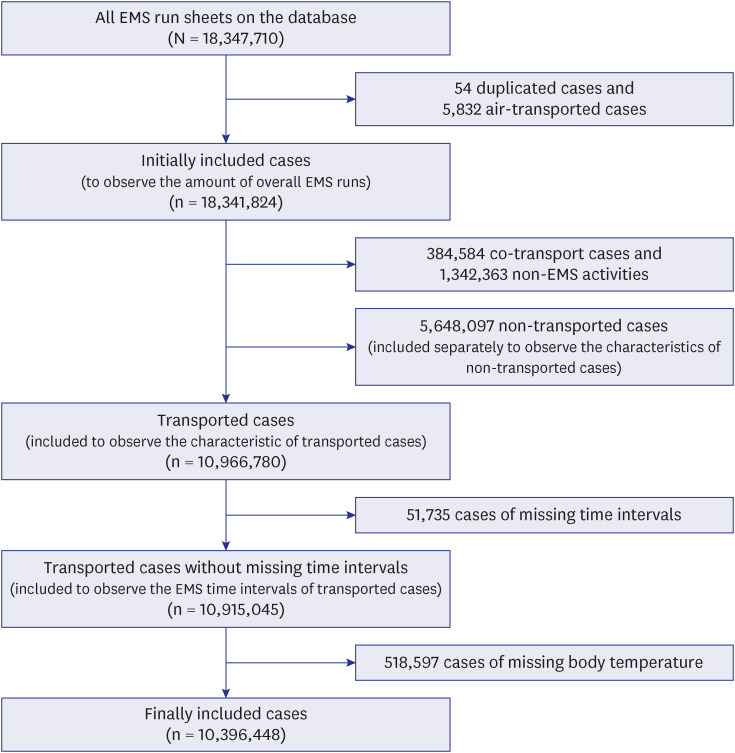
Methods
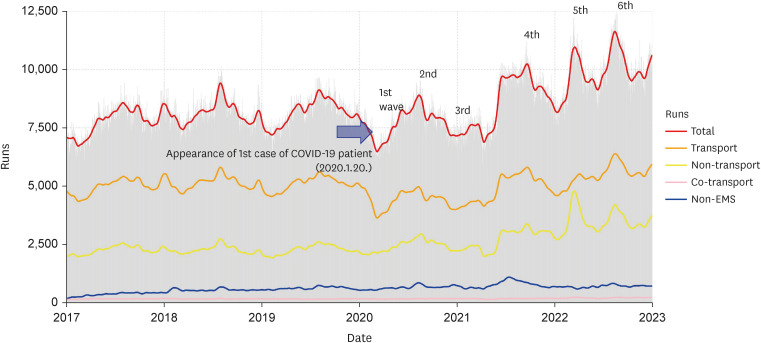
A retrospective analysis of EMS patient transportation data from 2017 to 2022 was conducted using the national EMS database.
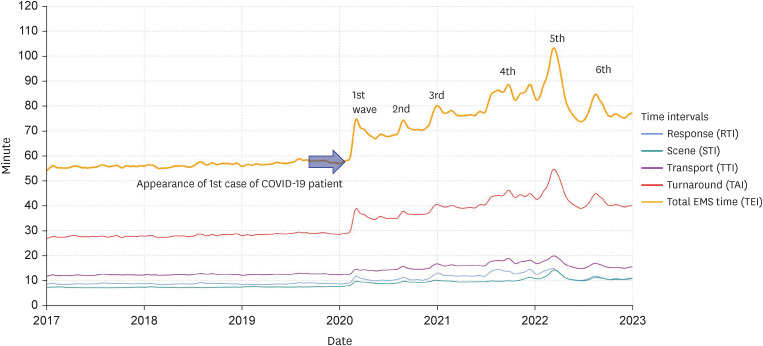
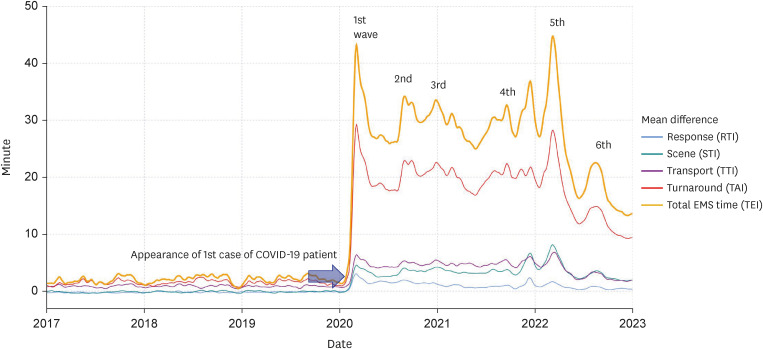
Results
Starting from the year 2020, coinciding with the COVID-19 outbreak, all EMS time intervals experienced an increase. For the years 2017 to 2022, the mean response time interval values were 8.6, 8.6, 8.6, 10.2, 12.8, and 11.4 minutes, and the mean scene time interval values were 7.1, 7.2, 7.4, 9.0, 9.8, and 10.9 minutes. The mean transport time interval (TTI) values were 12.1, 12.3, 12.4, 14.2, 16.9, and 16.2 minutes, and the mean turnaround time interval values were 27.6, 27.9, 28.7, 35.2, 42.0, and 43.1 minutes. Fever (≥ 37.5°C) patients experienced more pronounced prolongations in EMS time intervals compared to non-fever patients and had a higher probability of being non-transported. The mean differences in TTI between fever and non-fever patients were 0.8, 0.8, 0.8, 4.3, 4.8, and 3.2 minutes, respectively, from 2017 to 2022. Furthermore, the odds ratios for fever patients being transported to the emergency department were 2.7, 2.9, 2.8, 1.1, 0.8, and 0.7, respectively, from 2017 to 2022.
Conclusion
The study findings highlight the significant impact of the COVID-19 outbreak on the EMS system and emphasize the importance of ongoing monitoring to evaluate the burden on the EMS system.
Keyword
Figure
Reference
-
1. Ministry of Health and Welfare. COVID-19, changes in the response to infectious diseases over the past 3 years. Updated 2023. Accessed March 1, 2023. https://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=374685 .2. Seoul National University Hospital. COVID-19 white paper. Update 2022. Accessed March 1, 2023. http://www.snuh.org/m/board/B003/view.do?bbs_no=5963 .3. National Fire Agency. COVID-19 white paper. Updated 2022. Accessed March 1, 2023. https://www.korea.kr/archive/expDocView.do?docId=40137 .4. Satty T, Ramgopal S, Elmer J, Mosesso VN, Martin-Gill C. EMS responses and non-transports during the COVID-19 pandemic. Am J Emerg Med. 2021; 42:1–8. PMID: 33429185.5. Rollins MK, Nelson AR, Boyd J, Couturier K, Joseph D, Burns K, et al. Early changes in patient access interval during the COVID-19 pandemic. Prehosp Emerg Care. 2022; 26(5):641–651. PMID: 34669556.6. Lim YJ, Park SY. Increased prehospital emergency medical service time interval and nontransport rate of patients with fever using emergency medical services before and after COVID-19 in Busan, Korea. J Korean Med Sci. 2023; 38(9):e69. PMID: 36880110.7. National Fire Agency. 2022 statistical yearbook of emergency services. Updated 2022. Accessed March 1, 2023. https://www.nfa.go.kr/nfa/releaseinformation/statisticalinformation/ .8. Korea Center for Disease Control and Prevention. COVID-19 response guideline for healthcare facility (1-2 edition). Updated 2020. Accessed March 1, 2023. https://ncov.kdca.go.kr/duBoardList.do .9. Spaite DW, Valenzuela TD, Meislin HW, Criss EA, Hinsberg P. Prospective validation of a new model for evaluating emergency medical services systems by in-field observation of specific time intervals in prehospital care. Ann Emerg Med. 1993; 22(4):638–645. PMID: 8457088.10. Cone DC, Davidson SJ, Nguyen Q. A time-motion study of the emergency medical services turnaround interval. Ann Emerg Med. 1998; 31(2):241–246.11. Cleveland WS. LOWESS: a program for smoothing scatterplots by robust locally weighted regression. Am Stat. 1981; 35(1):54.12. Bezanson J, Edelman A, Karpinski S, Shah VB. Julia: a fresh approach to numerical computing. SIAM Rev. 2017; 59(1):65–98.13. Korea Center for Disease Control and Prevention. Information for adverse effect of COVID-19 vaccination. Updated 2021. Accessed March 1, 2023. https://ncv.kdca.go.kr/menu.es?mid=a10118040000 .14. Korea Center for Disease Control and Prevention. Symptoms that may appear after COVID-19 vaccination. How to deal with it? Updated 2021. Accessed March 1, 2023. https://www.kdca.go.kr/gallery.es?mid=a20503010000$bid=0002&act=view&list_no=145007 .15. Korea Center for Disease Control and Prevention. Operation guideline for the respiratory disease clinics (first edition). Updated 2022. Accessed March 1, 2023. https://ncov.kdca.go.kr/duBoardList.do .16. Ministry of Health and Welfare. The transitional plan for home treatment of COVID-19. Updated December 2021. Accessed March 1, 2023. https://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=368669 .17. Ministry of Health and Welfare. Social distancing is lifted after 2 years and 1 month. Updated April 2022. Accessed March 1, 2023. https://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=371078 .18. Eckstein M, Isaacs SM, Slovis CM, Kaufman BJ, Loflin JR, O’Connor RE, et al. Facilitating EMS turnaround intervals at hospitals in the face of receiving facility overcrowding. Prehosp Emerg Care. 2005; 9(3):267–275. PMID: 16147474.19. Cooney DR, Millin MG, Carter A, Lawner BJ, Nable JV, Wallus HJ. Ambulance diversion and emergency department offload delay: resource document for the National Association of EMS Physicians position statement. Prehosp Emerg Care. 2011; 15(4):555–561. PMID: 21870947.20. Cone DC, Middleton PM, Marashi Pour S. Analysis and impact of delays in ambulance to emergency department handovers. Emerg Med Australas. 2012; 24(5):525–533. PMID: 23039294.21. Backer HD, D'Arcy NT, Davis AJ, Barton B, Sporer KA. Statewide method of measuring ambulance patient offload times. Prehosp Emerg Care. 2019; 23(3):319–326. PMID: 30257596.22. Li M, Vanberkel P, Carter AJE. A review on ambulance offload delay literature. Health Care Manag Sci. 2019; 22(4):658–675. PMID: 29982911.23. Carter AJ, Overton J, Terashima M, Cone DC. Can emergency medical services use turnaround time as a proxy for measuring ambulance offload time? J Emerg Med. 2014; 47(1):30–35. PMID: 24373216.24. Lee YJ, Shin SD, Lee EJ, Cho JS, Cha WC. Emergency department overcrowding and ambulance turnaround time. PLoS One. 2015; 10(6):e0130758. PMID: 26115183.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of regional COVID-19 outbreak to emergency department response on acute myocardial infarction: a multicenter retrospective study
- Pre-Hospital Delay in Patients With Acute Stroke During the Initial Phase of the Coronavirus Disease 2019 Outbreak
- Changes in Clinical Characteristics among Febrile Patients Visiting the Emergency Department before and after the COVID-19 Outbreak
- Cardiovascular Imaging Asia in the Era of the COVID-19 Outbreak
- The impact of the COVID-19 pandemic on in-hospital mortality in patients admitted through the emergency department