J Korean Med Sci.
2022 Feb;37(6):e47. 10.3346/jkms.2022.37.e47.
Pre-Hospital Delay in Patients With Acute Stroke During the Initial Phase of the Coronavirus Disease 2019 Outbreak
- Affiliations
-
- 1Department of Emergency Medical Service, College of Health and Nursing, Kongju National University, Gongju, Korea
- 2Department of Emergency Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Emergency Medicine, Incheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea
- KMID: 2526035
- DOI: http://doi.org/10.3346/jkms.2022.37.e47
Abstract
- Background
When a sudden outbreak of an infectious disease occurs, emergency medical services (EMS) response could be negatively affected. The poor prognosis of acute stroke may be largely attributed to delays in treatment. This study aimed to identify the impact of the sudden outbreak of coronavirus disease 2019 (COVID-19) on EMS response for patients with acute stroke.
Methods
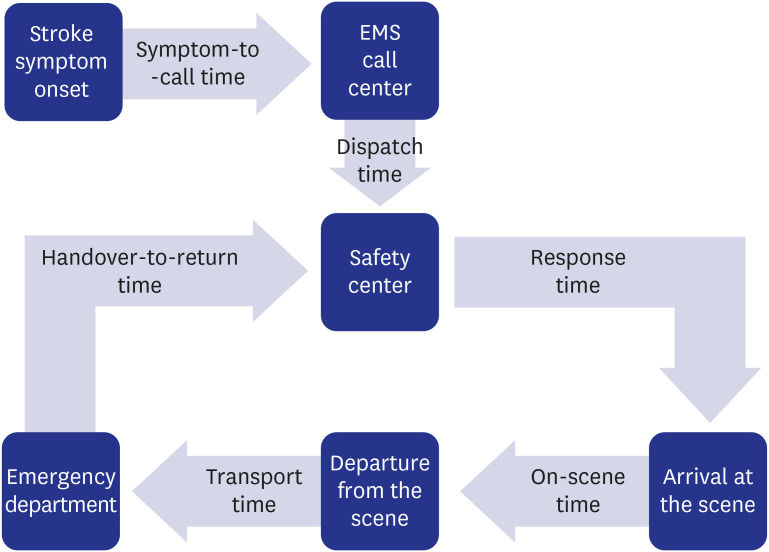
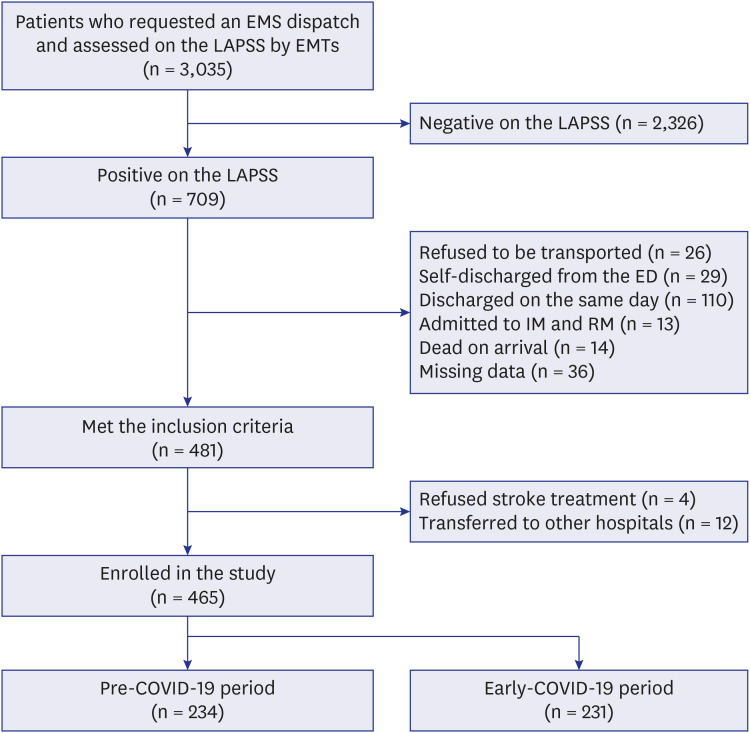
This comparative cross-sectional study was conducted in 25 safety centers in Seoul, Korea. We enrolled patients with acute stroke who were transferred to the emergency department by EMS. The study period was from February–April 2020 and the same period in 2019. Patients were divided into two groups, pre-COVID-19 period and early-COVID-19 period, and previously collected patient data were analyzed. We performed comparative analyses of EMS response and clinical outcomes between the groups.
Results
Of 465 patients, 231 (49.7%) had an acute stroke during the study period. There was no significant difference between clinical characteristics of patients with acute stroke before and after the COVID-19 outbreak. EMS response times increased significantly during the early COVID-19 outbreak. The intensive care unit admission rate and mortality rate increased during the early COVID-19 outbreak.
Conclusion
In the initial phase after the sudden COVID-19 outbreak, EMS response times for acute stroke were delayed and the clinical outcomes of patients with acute stroke deteriorated.
Figure
Reference
-
1. World Health Organization. The top 10 causes of death. Updated 2020. Accessed March 1, 2020. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death .2. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015; 131(4):e29–322. PMID: 25520374.3. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018; 49(3):e46–110. PMID: 29367334.4. Gu HQ, Rao ZZ, Yang X, Wang CJ, Zhao XQ, Wang YL, et al. Use of emergency medical services and timely treatment among ischemic stroke. Stroke. 2019; 50(4):1013–1016. PMID: 30841820.5. Romano JG, Muller N, Merino JG, Forteza AM, Koch S, Rabinstein AA. In-hospital delays to stroke thrombolysis: paradoxical effect of early arrival. Neurol Res. 2007; 29(7):664–666. PMID: 18173904.6. Fassbender K, Balucani C, Walter S, Levine SR, Haass A, Grotta J. Streamlining of prehospital stroke management: the golden hour. Lancet Neurol. 2013; 12(6):585–596. PMID: 23684084.7. Mohammad YM. Mode of arrival to the emergency department of stroke patients in the United States. J Vasc Interv Neurol. 2008; 1(3):83–86. PMID: 22518229.8. Bersano A, Kraemer M, Touzé E, Weber R, Alamowitch S, Sibon I, et al. Stroke care during the COVID-19 pandemic: experience from three large European countries. Eur J Neurol. 2020; 27(9):1794–1800. PMID: 32492764.9. Zhao J, Li H, Kung D, Fisher M, Shen Y, Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. 2020; 51(7):1996–2001. PMID: 32432997.10. Pop R, Quenardelle V, Hasiu A, Mihoc D, Sellal F, Dugay MH, et al. Impact of the COVID-19 outbreak on acute stroke pathways - insights from the Alsace region in France. Eur J Neurol. 2020; 27(9):1783–1787. PMID: 32399995.11. Kim JY, Lee KJ, Kang J, Kim BJ, Kim SE, Oh H, et al. Acute stroke care in Korea in 2013–2014: national averages and disparities. J Korean Med Sci. 2020; 35(20):e167. PMID: 32449325.12. Cha WC, Ahn KO, Shin SD, Park JH, Cho JS. Emergency department crowding disparity: a nationwide cross-sectional study. J Korean Med Sci. 2016; 31(8):1331–1336. PMID: 27478347.13. Kidwell CS, Starkman S, Eckstein M, Weems K, Saver JL. Identifying stroke in the field. Prospective validation of the Los Angeles Prehospital Stroke Screen (LAPSS). Stroke. 2000; 31(1):71–76. PMID: 10625718.14. American College of Surgeons Committee on Trauma. Advanced Trauma Life Support Course Instructor Manual: 1997. Chicago, IL, USA: American College of Surgeons;1997.15. Kothari R, Hall K, Brott T, Broderick J. Early stroke recognition: developing an out-of-hospital NIH Stroke Scale. Acad Emerg Med. 1997; 4(10):986–990. PMID: 9332632.16. Fassbender K, Walter S, Grunwald IQ, Merzou F, Mathur S, Lesmeister M, et al. Prehospital stroke management in the thrombectomy era. Lancet Neurol. 2020; 19(7):601–610. PMID: 32562685.17. Gonzalez-Aquines A, Cordero-Pérez AC, Cristobal-Niño M, Pérez-Vázquez G, Góngora-Rivera F; GECEN Investigators. Contribution of onset-to-alarm time to prehospital delay in patients with ischemic stroke. J Stroke Cerebrovasc Dis. 2019; 28(11):104331. PMID: 31519457.18. Fladt J, Meier N, Thilemann S, Polymeris A, Traenka C, Seiffge DJ, et al. Reasons for prehospital delay in acute ischemic stroke. J Am Heart Assoc. 2019; 8(20):e013101. PMID: 31576773.19. Seo AR, Song H, Lee WJ, Park KN, Moon J, Kim D. Factors associated with delay of emergency medical services activation in patients with acute stroke. J Stroke Cerebrovasc Dis. 2021; 30(1):105426. PMID: 33161352.20. Teo KC, Leung WC, Wong YK, Liu RK, Chan AH, Choi OM, et al. Delays in stroke onset to hospital arrival time during COVID-19. Stroke. 2020; 51(7):2228–2231. PMID: 32432998.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical and Epidemiological Characteristics of Coronavirus Disease 2019 in the Early Stage of Outbreak
- The proposed algorithm for emergency endoscopy during the coronavirus disease 2019 outbreak
- Care Process of Recanalization Therapy for Acute Stroke during the COVID-19 Outbreak in South Korea
- Characteristics of Acute Stroke in Patients with Coronavirus Disease 2019 and Challenges in Stroke Management during an Epidemic
- Epidemiology, Virology, and Clinical Features of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2; Coronavirus Disease-19)