Brain Tumor Res Treat.
2023 Oct;11(4):274-280. 10.14791/btrt.2023.0029.
Extensive Leptomeningeal Spreading of Ependymoma in an Adult: Case Report and Literature Review
- Affiliations
-
- 1Department of Neurosurgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2547417
- DOI: http://doi.org/10.14791/btrt.2023.0029
Abstract
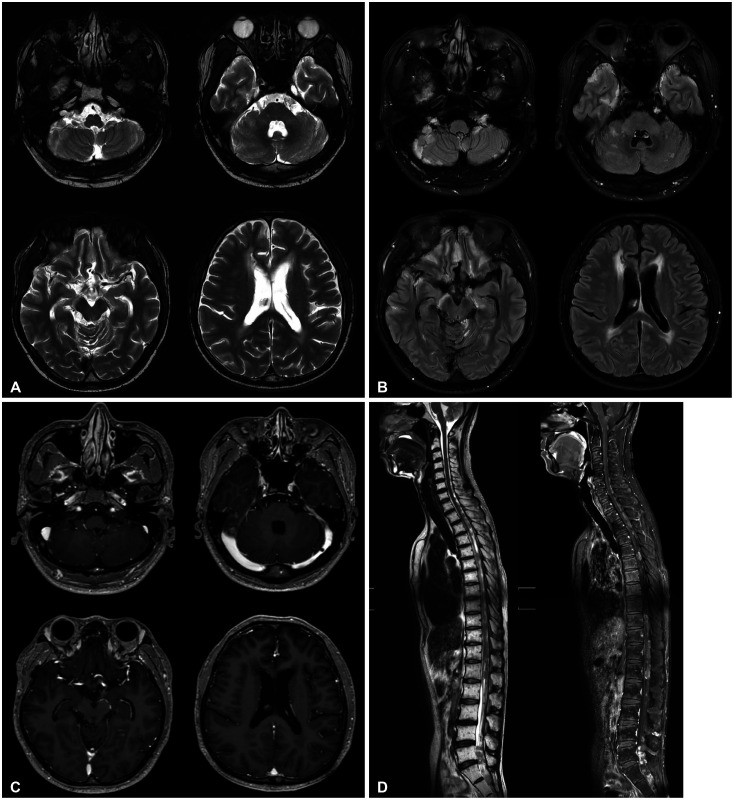
- Ependymoma is a rare adult tumor that originates from ependymal cells of the central nervous system, primarily occurring in the cerebral ventricles or the central canal of the spinal cord. In this paper, we report a case of extensive leptomeningeal seeding of ependymoma of a 39-year-old male patient, in whom the tumor was found incidentally after head trauma. The MRI exhibited diffuse leptomeningeal infiltrative lesions along with bilateral multiple cerebral sulci, basal cisterns, cerebellopontine angle, cerebellar folia. It also showed multinodular enhancing T1 low T2 high signal intensity lesions along the whole spinal cord. After the tumor biopsy at right temporal lesion, pathologic diagnosis was classic ependymoma (WHO grade 2). The patient has undergone radiation therapy and chemotherapy, and is currently maintaining a stable condition two years after surgery. This report suggests that when considering the differential diagnosis of extensive lesions both in the intracranial and intraspinal space, ependymoma should also be considered.
Keyword
Figure
Reference
-
1. McGuire CS, Sainani KL, Fisher PG. Incidence patterns for ependymoma: a surveillance, epidemiology, and end results study. J Neurosurg. 2009; 110:725–729. PMID: 19061350.
Article2. Berhili S, Aissa A, Kadiri S, Cherradi N, El Majjaoui S, El Kacemi H, et al. Extra-axial ependymoma of the cerebral convexity: a very rare intracranial adult tumor. Neuroradiol J. 2017; 30:281–285. PMID: 28059629.
Article3. Yuh EL, Barkovich AJ, Gupta N. Imaging of ependymomas: MRI and CT. Childs Nerv Syst. 2009; 25:1203–1213. PMID: 19360419.
Article4. Khatami D, Kasper EM, Bhadelia R, Rojas R. Radiologic characteristics of ependymomas: a case-based approach. J Neurosurg Sci. 2018; 62:38–45. PMID: 28945051.
Article5. Rudà R, Bruno F, Pellerino A, Soffietti R. Ependymoma: evaluation and management updates. Curr Oncol Rep. 2022; 24:985–993. PMID: 35384591.
Article6. Ostrom QT, Gittleman H, de Blank PM, Finlay JL, Gurney JG, McKean-Cowdin R, et al. American brain tumor association adolescent and young adult primary brain and central nervous system tumors diagnosed in the United States in 2008-2012. Neuro Oncol. 2016; 18(Suppl 1):i1–i50. PMID: 26705298.
Article7. Desandes E, Guissou S, Chastagner P, Lacour B. Incidence and survival of children with central nervous system primitive tumors in the French National Registry of Childhood Solid Tumors. Neuro Oncol. 2014; 16:975–983. PMID: 24470548.
Article8. Ostrom QT, Price M, Neff C, Cioffi G, Waite KA, Kruchko C, et al. CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2015-2019. Neuro Oncol. 2022; 24(Suppl 5):v1–v95. PMID: 36196752.
Article9. Schwartz TH, Kim S, Glick RS, Bagiella E, Balmaceda C, Fetell MR, et al. Supratentorial ependymomas in adult patients. Neurosurgery. 1999; 44:721–731. PMID: 10201296.
Article10. Aballa L, Chraa M, Louhab N, Kissani N. Extensive anaplastic multi-centric ependymoma in a young adult: case report and literature review. Egypt J Neurol Psychiatry Neurosurg. 2023; 59:67.
Article11. Lan Z, Richard SA, Zhang Y. Cerebellopontine angle ependymoma in a young adult: a case report. Medicine (Baltimore). 2019; 98:e15019. PMID: 30946332.12. Yust Katz S, Cachia D, Kamiya-Matsuoka C, Olar A, Theeler B, Penas Prado M, et al. Ependymomas arising outside of the central nervous system: a case series and literature review. J Clin Neurosci. 2018; 47:202–207. PMID: 29054328.
Article13. Sayegh ET, Aranda D, Kim JM, Oh T, Parsa AT, Oh MC. Prognosis by tumor location in adults with intracranial ependymomas. J Clin Neurosci. 2014; 21:2096–2101. PMID: 25037313.
Article14. Houjami M, Sahraoui S, Benchakroun N, Jouhadi H, Tawfiq N, Benider A. [Intracranial ependymomas: retrospective study of 16 cases]. Cancer Radiother. 2011; 15:136–139. French. PMID: 21256791.16. Dorfer C, Tonn J, Rutka JT. Ependymoma: a heterogeneous tumor of uncertain origin and limited therapeutic options. Handb Clin Neurol. 2016; 134:417–431. PMID: 26948369.17. Engelhard HH, Villano JL, Porter KR, Stewart AK, Barua M, Barker FG, et al. Clinical presentation, histology, and treatment in 430 patients with primary tumors of the spinal cord, spinal meninges, or cauda equina. J Neurosurg Spine. 2010; 13:67–77. PMID: 20594020.
Article18. Bertero L, Ricci AA, Tampieri C, Cassoni P, Modena P. Ependymomas. Pathologica. 2022; 114:436–446. PMID: 36534422.
Article19. Louis DN, Perry A, Wesseling P, Brat DJ, Cree IA, Figarella-Branger D, et al. The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro Oncol. 2021; 23:1231–1251. PMID: 34185076.
Article20. Pajtler KW, Witt H, Sill M, Jones DT, Hovestadt V, Kratochwil F, et al. Molecular classification of ependymal tumors across all CNS compartments, histopathological grades, and age groups. Cancer Cell. 2015; 27:728–743. PMID: 25965575.
Article21. Swanson AA, Raghunathan A, Jenkins RB, Messing-Jünger M, Pietsch T, Clarke MJ, et al. Spinal cord ependymomas with MYCN amplification show aggressive clinical behavior. J Neuropathol Exp Neurol. 2019; 78:791–797. PMID: 31373367.
Article22. Raffeld M, Abdullaev Z, Pack SD, Xi L, Nagaraj S, Briceno N, et al. High level MYCN amplification and distinct methylation signature define an aggressive subtype of spinal cord ependymoma. Acta Neuropathol Commun. 2020; 8:101. PMID: 32641156.
Article23. Thorp N, Gandola L. Management of ependymoma in children, adolescents and young adults. Clin Oncol (R Coll Radiol). 2019; 31:162–170. PMID: 30616927.
Article24. Chan MD, McMullen KP. Multidisciplinary management of intracranial ependymoma. Curr Probl Cancer. 2012; 36:6–19. PMID: 22325305.
Article25. Rudà R, Reifenberger G, Frappaz D, Pfister SM, Laprie A, Santarius T, et al. EANO guidelines for the diagnosis and treatment of ependymal tumors. Neuro Oncol. 2018; 20:445–456. PMID: 29194500.
Article26. Abdu AM, Alshoabi SA, Alshoaibi AM, Hamid AM, Jhaveri MD. Myxopapillary ependymoma with interval postoperative CSF seeding: a report of an unusual case. Radiol Case Rep. 2021; 16:3838–3843. PMID: 34691347.
Article27. Merchant TE, Bendel AE, Sabin ND, Burger PC, Shaw DW, Chang E, et al. Conformal radiation therapy for pediatric ependymoma, chemotherapy for incompletely resected ependymoma, and observation for completely resected, supratentorial ependymoma. J Clin Oncol. 2019; 37:974–983. PMID: 30811284.
Article28. Koshy M, Rich S, Merchant TE, Mahmood U, Regine WF, Kwok Y. Post-operative radiation improves survival in children younger than 3 years with intracranial ependymoma. J Neurooncol. 2011; 105:583–590. PMID: 21637963.
Article29. Merchant TE, Li C, Xiong X, Kun LE, Boop FA, Sanford RA. Conformal radiotherapy after surgery for paediatric ependymoma: a prospective study. Lancet Oncol. 2009; 10:258–266. PMID: 19274783.
Article30. Indelicato DJ, Ioakeim-Ioannidou M, Bradley JA, Mailhot-Vega RB, Morris CG, Tarbell NJ, et al. Proton therapy for pediatric ependymoma: mature results from a bicentric study. Int J Radiat Oncol Biol Phys. 2021; 110:815–820. PMID: 33508372.
Article31. Grill J, Le Deley MC, Gambarelli D, Raquin MA, Couanet D, Pierre-Kahn A, et al. Postoperative chemotherapy without irradiation for ependymoma in children under 5 years of age: a multicenter trial of the French Society of Pediatric Oncology. J Clin Oncol. 2001; 19:1288–1296. PMID: 11230470.
Article32. Garvin JH Jr, Selch MT, Holmes E, Berger MS, Finlay JL, Flannery A, et al. Phase II study of pre-irradiation chemotherapy for childhood intracranial ependymoma. Children’s Cancer Group protocol 9942: a report from the Children’s Oncology Group. Pediatr Blood Cancer. 2012; 59:1183–1189. PMID: 22949057.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acute Paraplegia as a Result of Hemorrhagic Spinal Ependymoma Masked by Spinal Anesthesia: Case Report and Review of Literature
- A Case of Subcutaneous Sacrococcygeal Myxopapillary Ependymoma: A Case Report
- A Case of Myxopapillary Ependymoma in the Cauda Equina: Case Report
- Post-traumatic leptomeningeal cyst in adult
- Ependymoma Containing Cartilage: A case report