Neurointervention.
2023 Nov;18(3):195-199. 10.5469/neuroint.2023.00283.
Unilateral Oculomotor Nerve Palsy as a Rare Manifestation of Isolated Pre-Communicating Segment of Posterior Cerebral Artery Thrombosis
- Affiliations
-
- 1Section of Endovascular Neurosurgery, Department of Neurosurgery, Ghaem Hospital, Mashhad University of Medical Sciences, Mashhad, Iran
- 2Department of Neurosurgery, Mazandaran University of Medical Sciences, Sari, Iran
- 3Department of Interventional Neuroradiology, Rothschild Foundation Hospital, Paris, France
- KMID: 2547282
- DOI: http://doi.org/10.5469/neuroint.2023.00283
Abstract
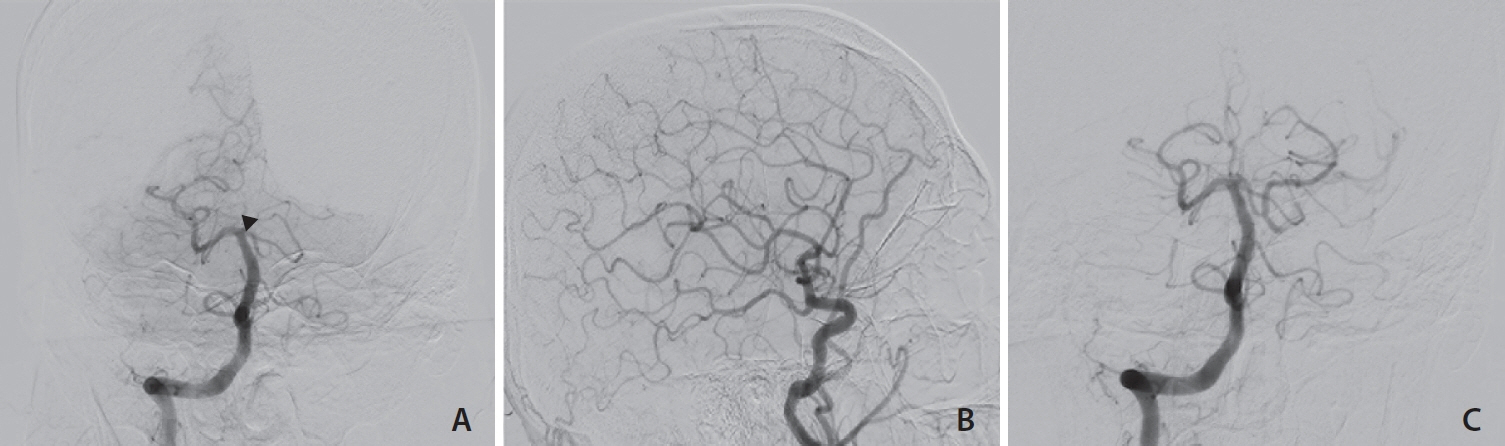
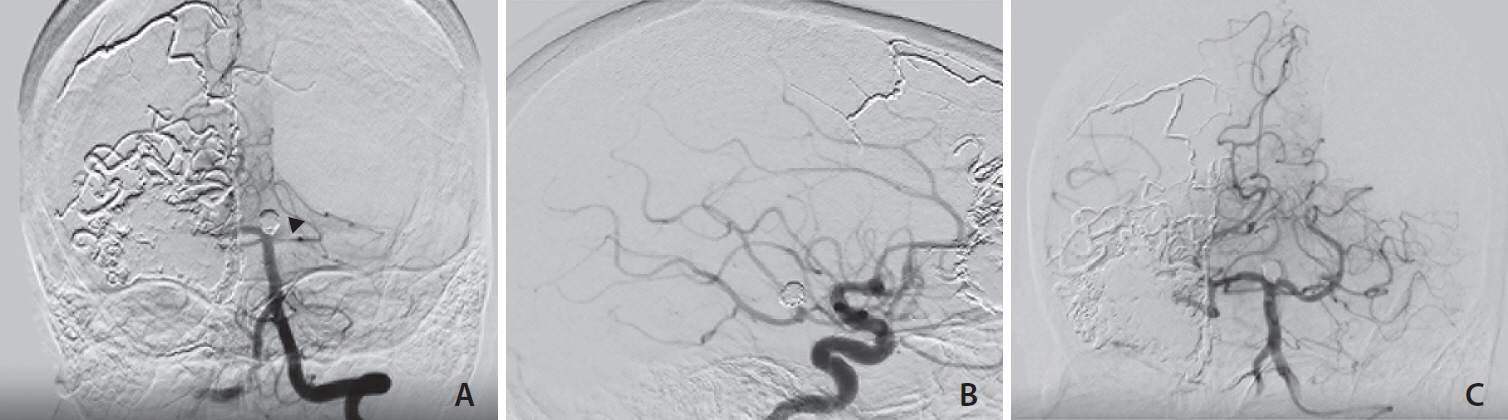
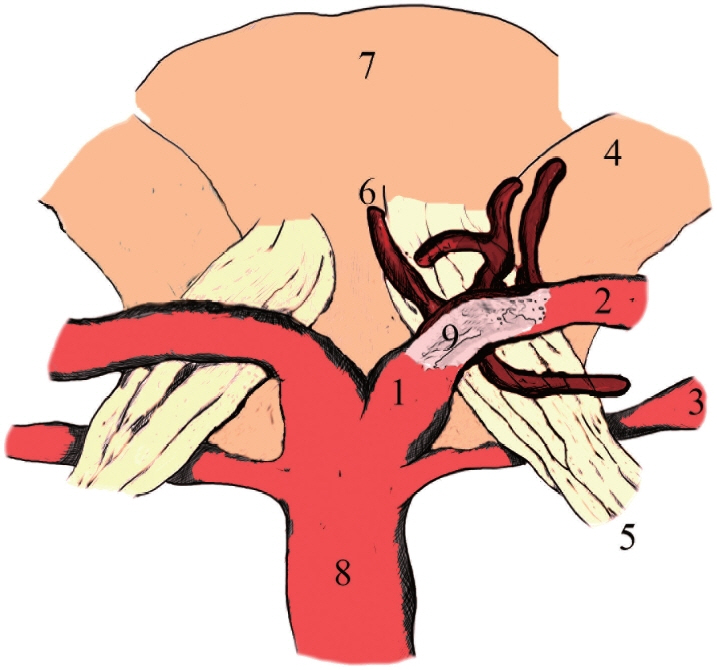
- Ipsilateral mydriasis (IM) is usually not acute. However, the acute occurrence of unilateral dilated pupil may result in acute ischemic stroke. Herein, we present 3 patients with IM, lateral eye deviation, ptosis, and contralateral hemiparesis due to isolated occlusion of the pre-communicating segment of the posterior cerebral artery with preservation of the posterior communicating artery, which was successfully treated by emergent mechanical thrombectomy. In a 3-month follow-up, all patients were independent without any neurological deficits.
Keyword
Figure
Reference
-
1. Lv X, Jiang C, Li Y, Yang X, Wu Z. Isolated oculomotor nerve palsy in interventional neuroradiology. Eur J Radiol. 2010; 74:441–444.
Article2. Clusmann H, Schaller C, Schramm J. Fixed and dilated pupils after trauma, stroke, and previous intracranial surgery: management and outcome. J Neurol Neurosurg Psychiatry. 2001; 71:175–181.
Article3. Hinduja A, Samant R, Feng D, Hannawi Y. Herniation despite decompressive hemicraniectomy in large hemispherical ischemic strokes. J Stroke Cerebrovasc Dis. 2018; 27:418–424.
Article4. Santos T, Morais H, Oliveira G, Barros P. Isolated oculomotor nerve palsy: a rare manifestation of internal carotid artery dissection. BMJ Case Rep. 2014; 2014:bcr2014205413.
Article5. Voss YL, Weber R, Nordmeyer H, Chapot R. Acute- onset oculomotor paresis attributed to isolated P1 occlusion successfully treated by mechanical thrombectomy. Stroke Vasc Interv Neurol. 2023; 3:e000682.
Article6. Maus V, Rogozinski S, Borggrefe J, Barnikol UB, Saklak M, Mpotsaris A. Clinical presentation of posterior cerebral artery occlusions - clinical rationale for a more aggressive therapeutic strategy? eNeurologicalSci. 2021; 25:100368.
Article7. Altenbernd J, Forsting M, Weber W, Fischer S. Thrombectomy of symptomatic isolated occlusions of posterior cerebral arteries in segment P1 and P2 in acute stroke treatment. Acta Radiol. 2022; 63:802–809.
Article8. Kaya AH, Dagcinar A, Ulu MO, Topal A, Bayri Y, Ulus A, et al. The perforating branches of the P1 segment of the posterior cerebral artery. J Clin Neurosci. 2010; 17:80–84.
Article9. Hendrix P, Griessenauer CJ, Foreman P, Shoja MM, Tubbs RS. Blood supply of the cranial nerves. In: Tubbs RS, Rizk E, Shoja MM, Loukas M, Barbaro N, Spinner RJ. Nerves and nerve injuries. Vol. 1, History, embryology, anatomy, imaging, and diagnostics. Academic Press, 2015;427-438.10. Krisht A, Barnett DW, Barrow DL, Bonner G. The blood supply of the intracavernous cranial nerves: an anatomic study. Neurosurgery. 1994; 34:275–279; discussion 279.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pituitary Apoplexy Presenting as Isolated Oculomotor Nerve Palsy
- Oculomotor Nerve Palsy in Internal Carotid-Posterior Communicating Artery Aneurysm
- Improvement of Unilateral Oculomotor Nerve Palsy after Clipping of Internal Carotid-posterior Communicating Artery Aneurysm
- Oculomotor Nerve Palsy Associated with Rupture of Middle Cerebral Artery Aneurysm
- Ruptured Anterior Communicating Artery Aneurysm Causing Bilateral Oculomotor Nerve Palsy: A Case Report