Acute Crit Care.
2023 Aug;38(3):298-307. 10.4266/acc.2022.01123.
Mechanically ventilated COVID-19 patients admitted to the intensive care unit in the United States with or without respiratory failure secondary to COVID-19 pneumonia: a retrospective comparison of characteristics and outcomes
- Affiliations
-
- 1Department of Medicine, Thomas Jefferson University, Philadelphia, PA, USA
- 2Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, PA, USA
- 3Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Medicine, Jane and Leonard Korman Respiratory Institute, Thomas Jefferson University, Philadelphia, PA, USA
- 4College of Population Health, Division of Biostatistics, Department of Pharmacology and Experimental Therapeutics, Thomas Jefferson University, Philadelphia, PA, USA
- KMID: 2547023
- DOI: http://doi.org/10.4266/acc.2022.01123
Abstract
- Background
There is increasing heterogeneity in the clinical phenotype of patients admitted to the intensive care unit (ICU) with coronavirus disease 2019 (COVID-19,) and reasons for mechanical ventilation are not limited to COVID pneumonia. We aimed to compare the characteristics and outcomes of intubated patients admitted to the ICU with the primary diagnosis of acute hypoxemic respiratory failure (AHRF) from COVID-19 pneumonia to those patients admitted for an alternative diagnosis.
Methods
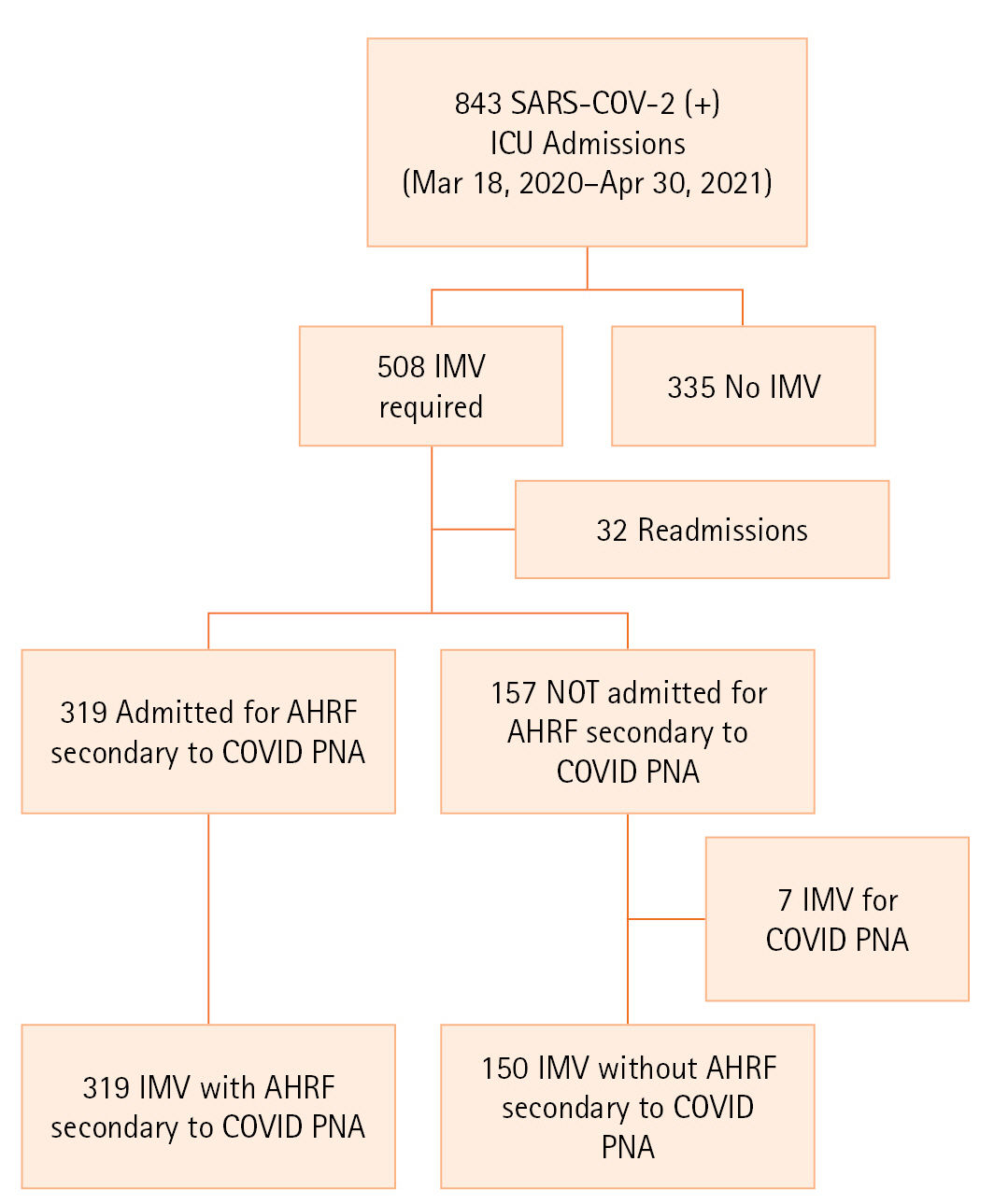
Retrospective cohort study of adults with confirmed SARS-CoV-2 infection admitted to nine ICUs between March 18, 2020, and April 30, 2021, at an urban university institution. We compared characteristics between the two groups using appropriate statistics. We performed logistic regression to identify risk factors for death in the mechanically ventilated COVID-19 population.
Results
After exclusions, the final sample consisted of 319 patients with respiratory failure secondary to COVID pneumonia and 150 patients intubated for alternative diagnoses. The former group had higher ICU and hospital mortality rates (57.7% vs. 36.7%, P<0.001 and 58.9% vs. 39.3%, P<0.001, respectively). Patients with AHRF secondary to COVID-19 pneumonia also had longer ICU and hospital lengths-of-stay (12 vs. 6 days, P<0.001 and 20 vs. 13.5 days, P=0.001). After risk-adjustment, these patients had 2.25 times higher odds of death (95% confidence interval, 1.42–3.56; P=0.001).
Conclusions
Mechanically ventilated COVID-19 patients admitted to the ICU with COVID-19-associated respiratory failure are at higher risk of hospital death and have worse ICU utilization outcomes than those whose reason for admission is unrelated to COVID pneumonia.
Figure
Reference
-
1. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382:1708–20.
Article2. Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA. 2002; 288:2151–62.
Article3. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009; 42:377–81.4. Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019; 95:103208.
Article5. Gupta S, Hayek SS, Wang W, Chan L, Mathews KS, Melamed ML, et al. Factors associated with death in critically ill patients with coronavirus disease 2019 in the US. JAMA Intern Med. 2020; 180:1436–47.6. ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012; 307:2526–33.7. King CS, Sahjwani D, Brown AW, Feroz S, Cameron P, Osborn E, et al. Outcomes of mechanically ventilated patients with COVID-19 associated respiratory failure. PLoS One. 2020; 15:e0242651.
Article8. Krause M, Douin DJ, Kim KK, Fernandez-Bustamante A, Bartels K. Characteristics and outcomes of mechanically ventilated COVID-19 patients: an observational cohort study. J Intensive Care Med. 2021; 36:271–6.
Article9. Sjoding MW, Admon AJ, Saha AK, Kay SG, Brown CA, Co I, et al. Comparing clinical features and outcomes in mechanically ventilated patients with COVID-19 and acute respiratory distress syndrome. Ann Am Thorac Soc. 2021; 18:1876–85.
Article10. Hodgson CL, Higgins AM, Bailey MJ, Mather AM, Beach L, Bellomo R, et al. Comparison of 6-month outcomes of survivors of COVID-19 versus non-COVID-19 critical illness. Am J Respir Crit Care Med. 2022; 205:1159–68.11. Todi S, Ghosh S. A comparative study on the outcomes of mechanically ventilated COVID-19 vs non-COVID-19 patients with acute hypoxemic respiratory failure. Indian J Crit Care Med. 2021; 25:1377–81.
Article12. Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016; 315:788–800.
Article13. Tzotzos SJ, Fischer B, Fischer H, Zeitlinger M. Incidence of ARDS and outcomes in hospitalized patients with COVID-19: a global literature survey. Crit Care. 2020; 24:516.
Article14. Armstrong RA, Kane AD, Cook TM. Outcomes from intensive care in patients with COVID-19: a systematic review and meta-analysis of observational studies. Anaesthesia. 2020; 75:1340–9.
Article15. Saha S, Al-Rifai RH, Saha S. Diabetes prevalence and mortality in COVID-19 patients: a systematic review, meta-analysis, and meta-regression. J Diabetes Metab Disord. 2021; 20:939–50.
Article16. Lim S, Bae JH, Kwon HS, Nauck MA. COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol. 2021; 17:11–30.
Article17. Nguyen NT, Chinn J, Nahmias J, Yuen S, Kirby KA, Hohmann S, et al. Outcomes and mortality among adults hospitalized with COVID-19 at US medical centers. JAMA Netw Open. 2021; 4:e210417.
Article18. Dongelmans DA, Termorshuizen F, Brinkman S, Bakhshi-Raiez F, Arbous MS, de Lange DW, et al. Characteristics and outcome of COVID-19 patients admitted to the ICU: a nationwide cohort study on the comparison between the first and the consecutive upsurges of the second wave of the COVID-19 pandemic in the Netherlands. Ann Intensive Care. 2022; 12:5.19. Lambermont B, Rousseau AF, Seidel L, Thys M, Cavalleri J, Delanaye P, et al. Outcome improvement between the first two waves of the coronavirus disease 2019 pandemic in a single tertiary-care hospital in Belgium. Crit Care Explor. 2021; 3:e0438.
Article20. Maslo C, Friedland R, Toubkin M, Laubscher A, Akaloo T, Kama B. Characteristics and outcomes of hospitalized patients in south africa during the COVID-19 Omicron wave compared with previous waves. JAMA. 2022; 327:583–4.
Article21. Carbonell R, Urgelés S, Rodríguez A, Bodí M, Martín-Loeches I, Solé-Violán J, et al. Mortality comparison between the first and second/third waves among 3,795 critical COVID-19 patients with pneumonia admitted to the ICU: a multicentre retrospective cohort study. Lancet Reg Health Eur. 2021; 11:100243.
Article22. Sartini M, Del Puente F, Oliva M, Carbone A, Blasi Vacca E, Parisini A, et al. Riding the COVID waves: clinical trends, outcomes, and remaining pitfalls of the SARS-CoV-2 pandemic: an analysis of two high-incidence periods at a hospital in Northern Italy. J Clin Med. 2021; 10:5239.
Article23. Hoogenboom WS, Pham A, Anand H, Fleysher R, Buczek A, Soby S, et al. Clinical characteristics of the first and second COVID-19 waves in the Bronx, New York: a retrospective cohort study. Lancet Reg Health Am. 2021; 3:100041.
Article24. Cowling BJ, Aiello AE. Public health measures to slow community spread of coronavirus disease 2019. J Infect Dis. 2020; 221:1749–51.
Article25. Worldometer. Coronavirus cases [Internet]. Worldometer;2022. [cited 2022 May 20]. Available from: https://www.worldometers.info/coronavirus/#countries.26. Ren SY, Wang WB, Gao RD, Zhou AM. Omicron variant (B.1.1.529) of SARS-CoV-2: mutation, infectivity, transmission, and vaccine resistance. World J Clin Cases. 2022; 10:1–11.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Outcomes of patients with COVID-19 requiring extracorporeal membrane oxygenation and continuous renal replacement therapy in the United States
- Comparison of critically ill COVID-19 and influenza patients with acute respiratory failure
- Point-of-Care Ultrasound for COVID-19 Pneumonia Patients in the ICU
- New-Onset Seizures in Patients With COVID-19: A Case Series From a Single Public Hospital in Korea
- Airway pressure release ventilation in mechanically ventilated patients with COVID-19: a multicenter observational study