Korean Circ J.
2023 Oct;53(10):693-707. 10.4070/kcj.2023.0083.
Clinical and Genetic Features of Korean Inherited Arrhythmia Probands
- Affiliations
-
- 1Division of Cardiology, Korea University College of Medicine and Korea University Medical Center, Seoul, Korea
- 2Department of Internal Medicine, Gachon University Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 3Department of Internal Medicine, Chungnam National University Hospital, Chungnam National University College of Medicine, Daejeon, Korea
- 4Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 5Department of Internal Medicine, Wonkwang University Hospital, Wonkwang University School of Medicine, Iksan, Korea
- 6Department of Internal Medicine, Severance Cardiovascular Hospital, Yonsei University College of Medicine, Seoul, Korea
- 7Department of Internal Medicine, Heart Vascular and Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 8Department of Cardiology, Chonnam National University Hospital, Chonnam National University School of Medicine, Gwangju, Korea
- 9Department of Cardiology, Ajou University School of Medicine, Suwon, Korea
- 10Department of Internal Medicine, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea
- 11Department of Internal Medicine, Keimyung University Dongsan Medical Center, Keimyung University College of Medicine, Daegu, Korea
- 12Department of Internal Medicine, Kyungpook National University Hospital, Daegu, Korea
- 13Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2546993
- DOI: http://doi.org/10.4070/kcj.2023.0083
Abstract
- Background and Objectives
Inherited arrhythmia (IA) is a more common cause of sudden cardiac death in Asian population, but little is known about the genetic background of Asian IA probands. We aimed to investigate the clinical characteristics and analyze the genetic underpinnings of IA in a Korean cohort.
Methods
This study was conducted in a multicenter cohort of the Korean IA Registry from 2014 to 2017. Genetic testing was performed using a next-generation sequencing panel including 174 causative genes of cardiovascular disease.
Results
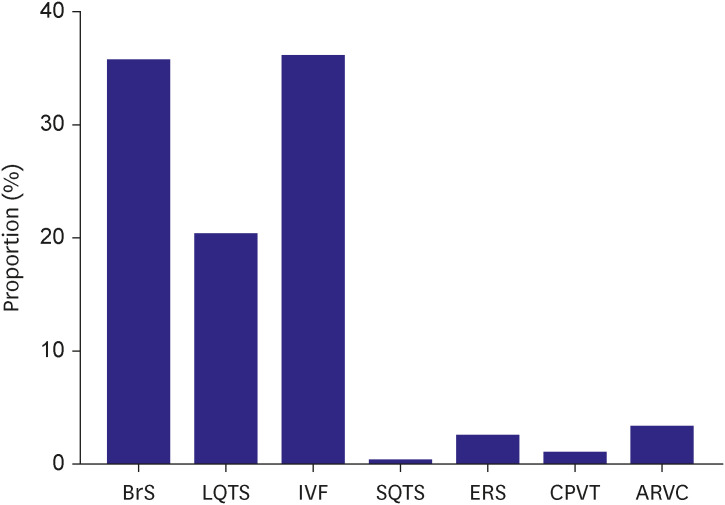
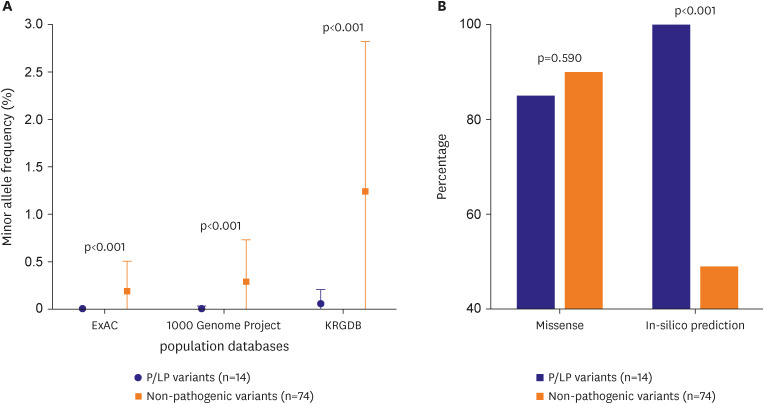
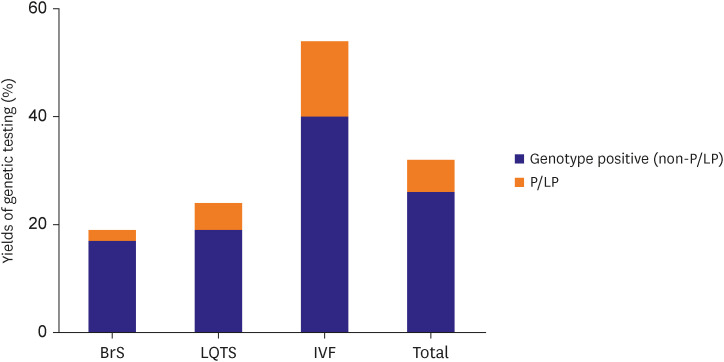
Among the 265 IA probands, idiopathic ventricular fibrillation (IVF) and Brugada Syndrome (BrS) was the most prevalent diseases (96 and 95 cases respectively), followed by long QT syndrome (LQTS, n=54). Two-hundred-sixteen probands underwent genetic testing, and 69 probands (31.9%) were detected with genetic variant, with yield of pathogenic or likely pathogenic variant as 6.4%. Left ventricular ejection fraction was significantly lower in genotype positive probands (54.7±11.3 vs. 59.3±9.2%, p=0.005). IVF probands showed highest yield of positive genotype (54.0%), followed by LQTS (23.8%), and BrS (19.5%).
Conclusions
There were significant differences in clinical characteristics and genetic yields among BrS, LQTS, and IVF. Genetic testing did not provide better yield for BrS and LQTS. On the other hand, in IVF, genetic testing using multiple gene panel might enable the molecular diagnosis of concealed genotype, which may alter future clinical diagnosis and management strategies.
Figure
Cited by 1 articles
-
Multicenter Cohort Analysis Unveil Inherited Arrhythmia in Korea
Il-young Oh
Korean Circ J. 2023;53(10):708-709. doi: 10.4070/kcj.2023.0214.
Reference
-
1. Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2018; 72:1677–1749. PMID: 29097294.2. Roh SY, Choi JI, Park SH, et al. The 10-year trend of out-of-hospital cardiac arrests: a Korean nationwide population-based study. Korean Circ J. 2021; 51:866–874. PMID: 34595855.
Article3. Roh SY, Choi JI, Kim MS, et al. Incidence and etiology of sudden cardiac arrest in Koreans: A cohort from the national health insurance service database. PLoS One. 2020; 15:e0242799. PMID: 33237971.
Article4. Roh SY, Choi JI, Kim MS, et al. Trends in the use of implantable cardioverter-defibrillators for prevention of sudden cardiac arrest: a South Korean nationwide population-based study. Pacing Clin Electrophysiol. 2019; 42:1086–1094. PMID: 31197835.
Article5. Murakoshi N, Aonuma K. Epidemiology of arrhythmias and sudden cardiac death in Asia. Circ J. 2013; 77:2419–2431. PMID: 24067274.
Article6. Kim YG, Oh SK, Choi HY, Choi JI. Inherited arrhythmia syndrome predisposing to sudden cardiac death. Korean J Intern Med. 2021; 36:527–538. PMID: 33092314.
Article7. Priori SG, Wilde AA, Horie M, et al. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm. 2013; 10:1932–1963. PMID: 24011539.
Article8. Oliver GR, Hart SN, Klee EW. Bioinformatics for clinical next generation sequencing. Clin Chem. 2015; 61:124–135. PMID: 25451870.
Article9. Richards S, Aziz N, Bale S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015; 17:405–424. PMID: 25741868.
Article10. Musunuru K, Hershberger RE, Day SM, et al. Genetic testing for inherited cardiovascular diseases: a scientific statement from the American Heart Association. Circ Genom Precis Med. 2020; 13:e000067. PMID: 32698598.
Article11. Kalia SS, Adelman K, Bale SJ, et al. Recommendations for reporting of secondary findings in clinical exome and genome sequencing, 2016 update (ACMG SF v2.0): a policy statement of the American College of Medical Genetics and Genomics. Genet Med. 2017; 19:249–255. PMID: 27854360.12. Isbister JC, Nowak N, Butters A, et al. “Concealed cardiomyopathy” as a cause of previously unexplained sudden cardiac arrest. Int J Cardiol. 2021; 324:96–101. PMID: 32931854.
Article13. Bagnall RD, Weintraub RG, Ingles J, et al. A prospective study of sudden cardiac death among children and young adults. N Engl J Med. 2016; 374:2441–2452. PMID: 27332903.
Article14. Cirino AL, Harris S, Lakdawala NK, et al. Role of genetic testing in inherited cardiovascular disease: a review. JAMA Cardiol. 2017; 2:1153–1160. PMID: 28793145.
Article15. Sturm AC, Hershberger RE. Genetic testing in cardiovascular medicine: current landscape and future horizons. Curr Opin Cardiol. 2013; 28:317–325. PMID: 23571470.16. Hosseini SM, Kim R, Udupa S, et al. Reappraisal of reported genes for sudden arrhythmic death: evidence-based evaluation of gene validity for Brugada syndrome. Circulation. 2018; 138:1195–1205. PMID: 29959160.
Article17. Ackerman MJ, Priori SG, Willems S, et al. HRS/EHRA expert consensus statement on the state of genetic testing for the channelopathies and cardiomyopathies this document was developed as a partnership between the Heart Rhythm Society (HRS) and the European Heart Rhythm Association (EHRA). Heart Rhythm. 2011; 8:1308–1339. PMID: 21787999.
Article18. Shimizu W. Clinical impact of genetic studies in lethal inherited cardiac arrhythmias. Circ J. 2008; 72:1926–1936. PMID: 18981593.
Article19. Lee YS, Kwon BS, Kim GB, et al. Long QT syndrome: a Korean single center study. J Korean Med Sci. 2013; 28:1454–1460. PMID: 24133349.
Article20. Ahn KJ, Song MK, Lee SY, et al. The outcome of long QT syndrome, a Korean single center study. korean circ j. 2022; 52:771–781. PMID: 36217598.
Article21. Adler A, Novelli V, Amin AS, et al. An international, multicentered, evidence-based reappraisal of genes reported to cause congenital long QT syndrome. Circulation. 2020; 141:418–428. PMID: 31983240.
Article22. Bains S, Neves R, Bos JM, Giudicessi JR, MacIntyre C, Ackerman MJ. Phenotypes of overdiagnosed long QT syndrome. J Am Coll Cardiol. 2023; 81:477–486. PMID: 36725176.
Article23. Neves R, Tester DJ, Simpson MA, Behr ER, Ackerman MJ, Giudicessi JR. Exome sequencing highlights a potential role for concealed cardiomyopathies in youthful sudden cardiac death. Circ Genom Precis Med. 2022; 15:e003497. PMID: 34949102.
Article24. Grondin S, Davies B, Cadrin-Tourigny J, et al. Importance of genetic testing in unexplained cardiac arrest. Eur Heart J. 2022; 43:3071–3081. PMID: 35352813.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Value of next‑generation sequencing in inherited arrhythmia syndromes
- Clinical role of genetic testing for the Brugada syndrome overlapping with arrhythmogenic cardiomyopathy
- Inherited arrhythmia syndrome predisposing to sudden cardiac death
- Genetic Diseases Associated with Diabetes Mellitus
- Genetics and genomics of bone marrow failure syndrome