J Korean Med Sci.
2023 Sep;38(38):e294. 10.3346/jkms.2023.38.e294.
Multiple Antiplatelet Therapy in Ischemic Stroke Already on Antiplatelet Agents Based on the Linked Big Data for Stroke
- Affiliations
-
- 1Department of Neurology, Seoul National University Hospital, Seoul, Korea
- 2Department of Critical Care Medicine, Seoul National University Hospital, Seoul, Korea
- 3Department of Clinical Epidemiology and Biostatistics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 4Department of Neurology, Gangdong Sacred Heart Hospital, Seoul, Korea
- 5Department of Neurology, Hallym University Sacred Heart Hospital, Anyang, Korea
- 6Department of Neurology, Uijeongbu Eulji Medical Center, Uijeongbu, Korea
- KMID: 2546217
- DOI: http://doi.org/10.3346/jkms.2023.38.e294
Abstract
- Background
Optimal antiplatelet strategy for patients with ischemic stroke who were already on single antiplatelet therapy (SAPT) remains to be elucidated. This study aimed to evaluate the effect of different antiplatelet regimens on vascular and safety outcomes at 1 year after non-cardioembolic stroke in patients previously on SAPT.
Methods
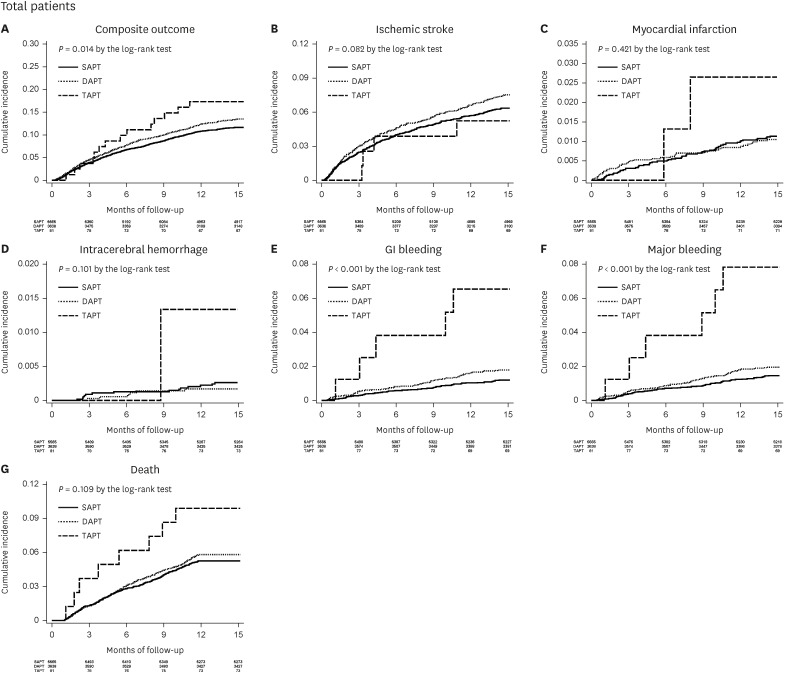
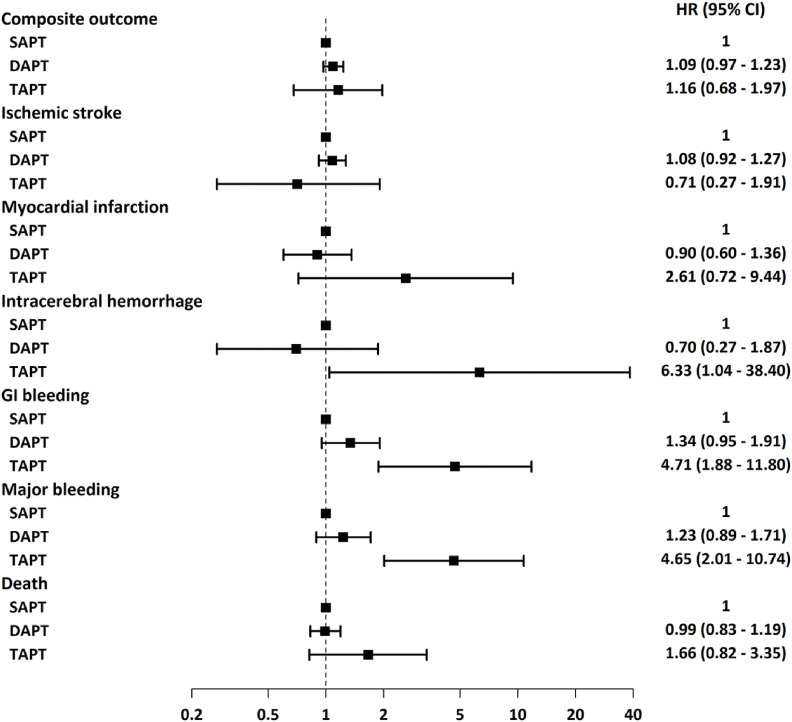
We identified 9,284 patients with acute non-cardioembolic ischemic stroke that occurred on SAPT using linked data. Patients were categorized into three groups according to antiplatelet strategy at discharge: 1) SAPT; 2) dual antiplatelet therapy (DAPT); and 3) triple antiplatelet therapy (TAPT). One-year outcomes included recurrent ischemic stroke, composite outcomes (recurrent ischemic stroke, myocardial infarction, intracerebral hemorrhage, and death), and major bleeding.
Results
Of 9,284 patients, 5,565 (59.9%) maintained SAPT, 3,638 (39.2%) were treated with DAPT, and 81 (0.9%) were treated with TAPT. Multiple antiplatelet therapy did not reduce the risks of 1-year recurrent stroke (DAPT, hazard ratio [HR], 1.08, 95% confidence interval [CI], 0.92–1.27, P = 0.339; TAPT, HR, 0.71, 95% CI, 0.27–1.91, P = 0.500) and 1-year composite outcome (DAPT, HR, 1.09, 95% CI, 0.68–1.97, P = 0.592; TAPT, HR, 1.46, 95% CI, 0.68–1.97, P = 0.592). However, the TAPT groups showed an increased risk of major bleeding complications (DAPT, HR, 1.23, 95% CI, 0.89–1.71, P = 0.208; TAPT, HR, 4.65, 95% CI, 2.01–10.74, P < 0.001).
Conclusion
Additional use of antiplatelet agents in patients with non-cardioembolic ischemic stroke who were already on SAPT did not reduce the 1-year incidence of vascular outcomes, although it increased the risk of bleeding complications.
Figure
Reference
-
1. Burn J, Dennis M, Bamford J, Sandercock P, Wade D, Warlow C. Long-term risk of recurrent stroke after a first-ever stroke. The Oxfordshire Community Stroke Project. Stroke. 1994; 25(2):333–337. PMID: 8303740.
Article2. Mohan KM, Wolfe CD, Rudd AG, Heuschmann PU, Kolominsky-Rabas PL, Grieve AP. Risk and cumulative risk of stroke recurrence: a systematic review and meta-analysis. Stroke. 2011; 42(5):1489–1494. PMID: 21454819.3. Girotra T, Lowe F, Feng W, Ovbiagele B. Antiplatelet agents in secondary stroke prevention: selection, timing, and dose. Curr Treat Options Neurol. 2018; 20(8):32. PMID: 29936577.
Article4. Yang Y, Zhou M, Zhong X, Wang Y, Zhao X, Liu L, et al. Dual versus mono antiplatelet therapy for acute non-cardioembolic ischaemic stroke or transient ischaemic attack: a systematic review and meta-analysis. Stroke Vasc Neurol. 2018; 3(2):107–116. PMID: 30022798.
Article5. Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, et al. 2021 Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021; 52(7):e364–e467. PMID: 34024117.
Article6. Pugliese F, Arasaratnam P, Moellenberg M, Dani S. Short- vs. long-term dual antiplatelet therapy in secondary prevention for ischaemic stroke: a network metanalysis. Eur Heart J Qual Care Clin Outcomes. 2019; 5(4):298–309. PMID: 31050716.
Article7. Park HK, Ko SB, Jung KH, Jang MU, Kim DH, Kim JT, et al. 2022 Update of the Korean clinical practice guidelines for stroke: antithrombotic therapy for patients with acute ischemic stroke or transient ischemic attack. J Stroke. 2022; 24(1):166–175. PMID: 35135073.
Article8. Bath PM, Woodhouse LJ, Appleton JP, Beridze M, Christensen H, Dineen RA, et al. Antiplatelet therapy with aspirin, clopidogrel, and dipyridamole versus clopidogrel alone or aspirin and dipyridamole in patients with acute cerebral ischaemia (TARDIS): a randomised, open-label, phase 3 superiority trial. Lancet. 2018; 391(10123):850–859. PMID: 29274727.9. Diener HC, Bogousslavsky J, Brass LM, Cimminiello C, Csiba L, Kaste M, et al. Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo-controlled trial. Lancet. 2004; 364(9431):331–337. PMID: 15276392.
Article10. SPS3 Investigators. Benavente OR, Hart RG, McClure LA, Szychowski JM, Coffey CS, et al. Effects of clopidogrel added to aspirin in patients with recent lacunar stroke. N Engl J Med. 2012; 367(9):817–825. PMID: 22931315.
Article11. Tsivgoulis G, Safouris A, Kim DE, Alexandrov AV. Recent advances in primary and secondary prevention of atherosclerotic stroke. J Stroke. 2018; 20(2):145–166. PMID: 29886715.
Article12. Hong KS, Lee SH, Kim EG, Cho KH, Chang DI, Rha JH, et al. Recurrent ischemic lesions after acute atherothrombotic stroke: clopidogrel plus aspirin versus aspirin alone. Stroke. 2016; 47(9):2323–2330. PMID: 27418597.
Article13. Naqvi IA, Kamal AK, Rehman H. Multiple versus fewer antiplatelet agents for preventing early recurrence after ischaemic stroke or transient ischaemic attack. Cochrane Database Syst Rev. 2020; 8(8):CD009716. PMID: 32813275.
Article14. Amarenco P. Steering Committee and Investigators of the TIAregistry.org Project. Five-year risk of stroke after TIA or minor ischemic stroke. N Engl J Med. 2018; 379(16):1580–1581.
Article15. Flach C, Muruet W, Wolfe CD, Bhalla A, Douiri A. Risk and secondary prevention of stroke recurrence: a population-base cohort study. Stroke. 2020; 51(8):2435–2444. PMID: 32646337.16. Wang IK, Yen TH, Guo YC, Sun Y, Lien LM, Chang WL, et al. Antiplatelet agents for the secondary prevention of ischaemic stroke in patients with or without renal dysfunction. Eur J Neurol. 2020; 27(3):572–578. PMID: 31693249.
Article17. Hackam DG, Spence JD. Antiplatelet therapy in ischemic stroke and transient ischemic attack: an overview of major trials and meta-analyses. Stroke. 2019; 50(3):773–778. PMID: 30626286.
Article18. Albright KC, Howard VJ, Howard G. Selecting an optimal antiplatelet agent for secondary stroke prevention. Neurol Clin Pract. 2021; 11(2):e121–e128. PMID: 33842080.
Article19. Kim JT, Park MS, Choi KH, Cho KH, Kim BJ, Han MK, et al. Different antiplatelet strategies in patients with new ischemic stroke while taking aspirin. Stroke. 2016; 47(1):128–134. PMID: 26604247.
Article20. Kim TJ, Lee JS, Kim JW, Oh MS, Mo H, Lee CH, et al. Building linked big data for stroke in Korea: linkage of stroke registry and national health insurance claims data. J Korean Med Sci. 2018; 33(53):e343. PMID: 30595684.
Article21. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24(1):35–41. PMID: 7678184.
Article22. Lee SR, Lee HJ, Choi EK, Han KD, Jung JH, Cha MJ, et al. Direct oral anticoagulants in patients with atrial fibrillation and liver disease. J Am Coll Cardiol. 2019; 73(25):3295–3308. PMID: 31248551.
Article23. Lee SR, Choi EK, Park CS, Han KD, Jung JH, Oh S, et al. Direct oral anticoagulants in patients with nonvalvular atrial fibrillation and low body weight. J Am Coll Cardiol. 2019; 73(8):919–931. PMID: 30819360.
Article24. Lee SR, Choi EK, Kwon S, Jung JH, Han KD, Cha MJ, et al. Oral anticoagulation in Asian patients with atrial fibrillation and a history of intracranial hemorrhage. Stroke. 2020; 51(2):416–423. PMID: 31813363.
Article25. Johnston SC, Easton JD, Farrant M, Barsan W, Conwit RA, Elm JJ, et al. Clopidogrel and aspirin in Acute ischemic stroke and high-risk TIA. N Engl J Med. 2018; 379(3):215–225. PMID: 29766750.
Article26. Wang Y, Wang Y, Zhao X, Liu L, Wang D, Wang C, et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N Engl J Med. 2013; 369(1):11–19. PMID: 23803136.
Article27. Firth D. Bias reduction of maximum likelihood estimates. Biometrika. 1993; 80(1):27–38.
Article28. Heinze G, Schemper M. A solution to the problem of monotone likelihood in Cox regression. Biometrics. 2001; 57(1):114–119. PMID: 11252585.
Article29. Trifan G, Gorelick PB, Testai FD. Efficacy and safety of using dual versus monotherapy antiplatelet agents in secondary stroke prevention: systematic review and meta-analysis of randomized controlled clinical trials. Circulation. 2021; 143(25):2441–2453. PMID: 33926204.
Article30. Johnston SC, Amarenco P, Denison H, Evans SR, Himmelmann A, James S, et al. Ticagrelor and aspirin or aspirin alone in acute ischemic stroke or TIA. N Engl J Med. 2020; 383(3):207–217. PMID: 32668111.
Article31. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50(12):e344–e418. PMID: 31662037.
Article32. Moussouttas M, Papamitsakis NI. Critique on the use of early short-term dual antiplatelet therapy following minor acute cerebral ischemic events. Cerebrovasc Dis. 2020; 49(3):237–243. PMID: 32369825.
Article33. Wang Y, Pan Y, Zhao X, Li H, Wang D, Johnston SC, et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack (CHANCE) trial: one-year outcomes. Circulation. 2015; 132(1):40–46. PMID: 25957224.
Article34. Wang X, Zhao X, Johnston SC, Xian Y, Hu B, Wang C, et al. Effect of clopidogrel with aspirin on functional outcome in TIA or minor stroke: CHANCE substudy. Neurology. 2015; 85(7):573–579. PMID: 26283758.
Article35. Markus HS, Droste DW, Kaps M, Larrue V, Lees KR, Siebler M, et al. Dual antiplatelet therapy with clopidogrel and aspirin in symptomatic carotid stenosis evaluated using doppler embolic signal detection: the Clopidogrel and Aspirin for Reduction of Emboli in Symptomatic Carotid Stenosis (CARESS) trial. Circulation. 2005; 111(17):2233–2240. PMID: 15851601.
Article36. Toyoda K, Uchiyama S, Yamaguchi T, Easton JD, Kimura K, Hoshino H, et al. Dual antiplatelet therapy using cilostazol for secondary prevention in patients with high-risk ischaemic stroke in Japan: a multicentre, open-label, randomised controlled trial. Lancet Neurol. 2019; 18(6):539–548. PMID: 31122494.
Article37. Pan Y, Elm JJ, Li H, Easton JD, Wang Y, Farrant M, et al. Outcomes associated with clopidogrel-aspirin use in minor stroke or transient ischemic attack: a pooled analysis of Clopidogrel in High-Risk Patients With Acute Non-Disabling Cerebrovascular Events (CHANCE) and Platelet-Oriented Inhibition in New TIA and Minor Ischemic Stroke (POINT) Trials. JAMA Neurol. 2019; 76(12):1466–1473. PMID: 31424481.
Article38. Liu L, Wong KS, Leng X, Pu Y, Wang Y, Jing J, et al. Dual antiplatelet therapy in stroke and ICAS: subgroup analysis of CHANCE. Neurology. 2015; 85(13):1154–1162. PMID: 26330567.39. Amarenco P, Denison H, Evans SR, Himmelmann A, James S, Knutsson M, et al. Ticagrelor added to aspirin in acute nonsevere ischemic stroke or transient ischemic attack of atherosclerotic origin. Stroke. 2020; 51(12):3504–3513. PMID: 33198608.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antiplatelet Therapy for Secondary Stroke Prevention in Patients with Ischemic Stroke or Transient Ischemic Attack
- Dual Antiplatelet Therapy after Noncardioembolic Ischemic Stroke or Transient Ischemic Attack: Pros and Cons
- Pharmacological Secondary Prevention of Ischemic Stroke
- Discontinuation of antiplatelet therapy after stent-assisted coil embolization for cerebral aneurysms
- Early Neurological Deterioration and Time to Start Dual Antiplatelet Therapy in Patients With Acute Mild-to-Moderate Ischemic Stroke: A Pre-Specified Post Hoc Analysis of the ATAMIS Trial