J Cerebrovasc Endovasc Neurosurg.
2023 Sep;25(3):333-339. 10.7461/jcen.2022.E2022.06.011.
Endovascular recanalization therapy for patients with acute ischemic stroke with hidden aortic dissection: A case series
- Affiliations
-
- 1Department of Neurology, Daejeon-Chungnam Regional Cerebrovascular Center, Chungnam National University Hospital, Daejeon, Korea
- 2Department of Neurosurgery, Daejeon-Chungnam Regional Cerebrovascular Center, Chungnam National University Hospital, Daejeon, Korea
- KMID: 2546171
- DOI: http://doi.org/10.7461/jcen.2022.E2022.06.011
Abstract
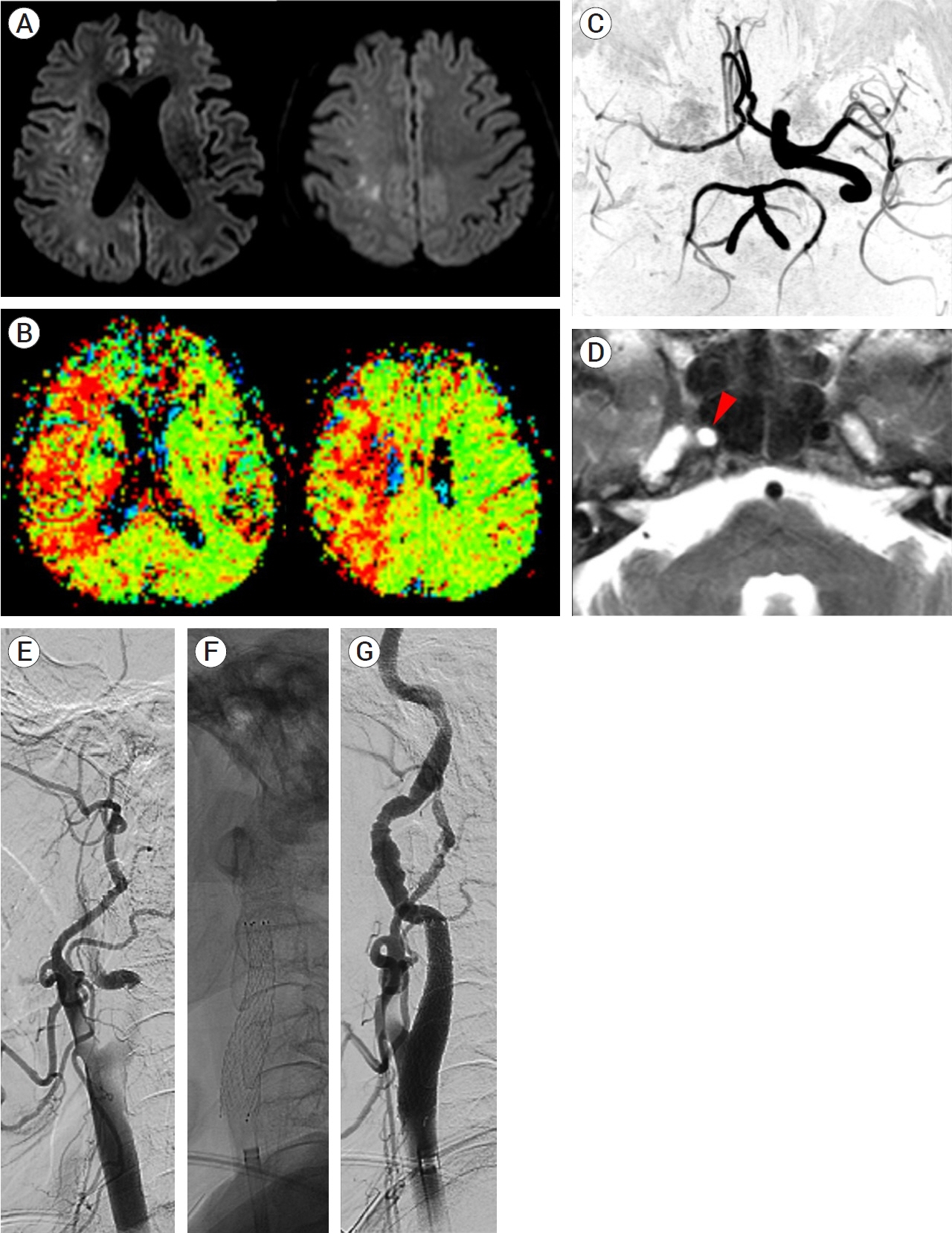
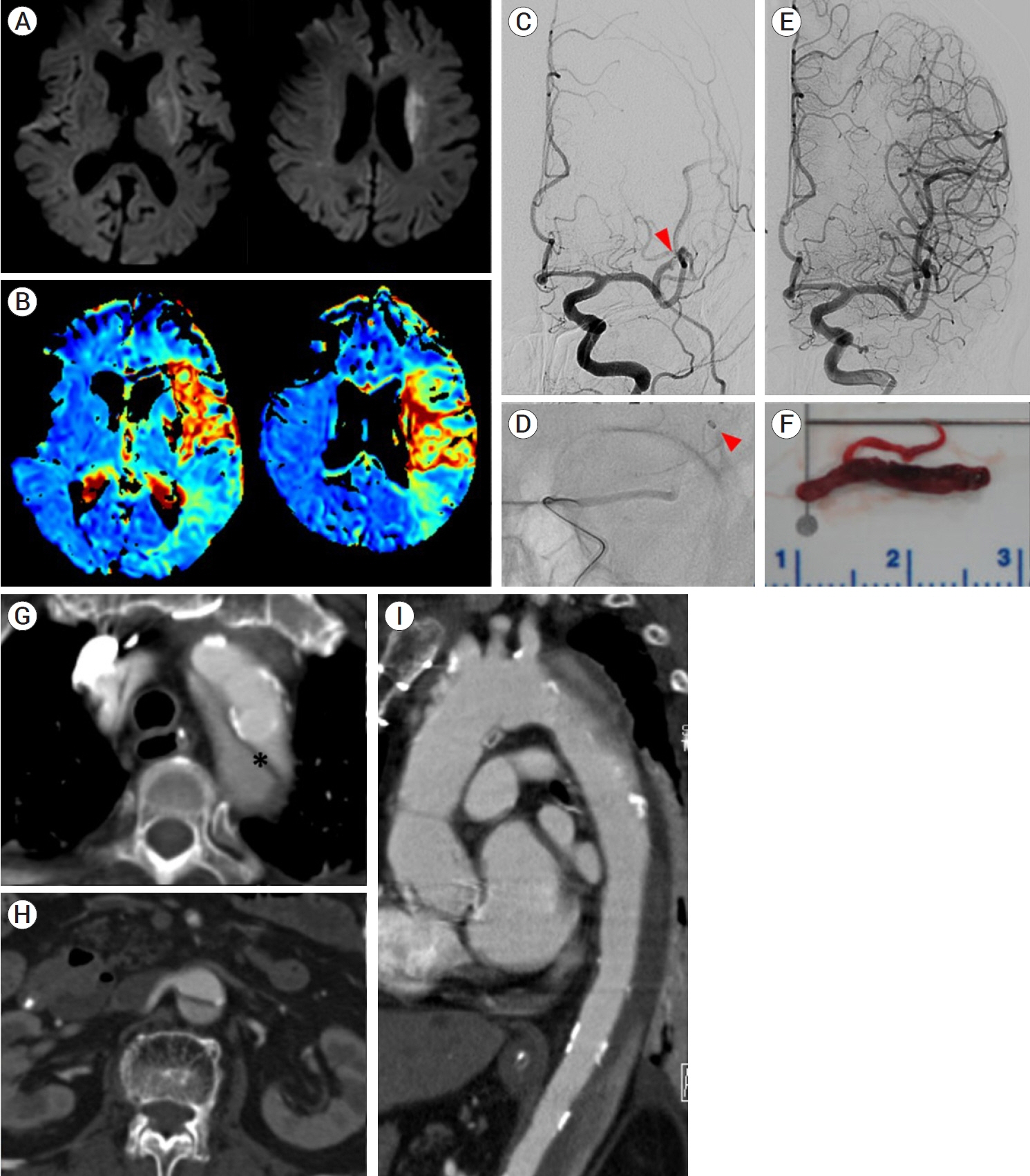
- Aortic dissection is one of the causes of acute ischemic stroke. Endovascular recanalization therapy (EVT) has emerged as an essential treatment for acute ischemic stroke due to large artery occlusion. However, it is rarely performed in the situation of hidden aortic dissection (AD). Two patients presented to the emergency room with focal neurologic deficits. The first patient was diagnosed with right internal carotid artery (ICA) occlusion. Angiography revealed that the ICA was occluded by the dissection flap. After a stent deployment in the proximal ICA, the antegrade flow was restored. The patient was diagnosed with AD on chest computed tomography (CT) after EVT. For the second patient, intraarterial thrombectomy was performed to treat left middle cerebral artery occlusion. AD was first detected on echocardiography, which was performed after EVT. Herein, we report successful endovascular recanalization therapy performed in two patients with acute ischemic stroke in the situation of undiagnosed aortic dissection. We also reviewed previous case reports and relevant literature.
Figure
Reference
-
1. Funakoshi Y, Imamura H, Tokunaga S, Murakami Y, Tani S, Adachi H, et al. Carotid artery stenting before surgery for carotid artery occlusion associated with acute type A aortic dissection: two case reports. Interv Neuroradiol. 2020; Dec. 26(6):814–20.2. Grupper M, Eran A, Shifrin A. Ischemic stroke, aortic dissection, and thrombolytic therapy-the importance of basic clinical skills. J Gen Intern Med. 2007; Sep. 22(9):1370–2.3. Howard DP, Banerjee A, Fairhead JF, Perkins J, Silver LE, Rothwell PM, et al. Population-based study of incidence and outcome of acute aortic dissection and premorbid risk factor control: 10-year results from the Oxford Vascular Study. Circulation. 2013; May. 127(20):2031–7.4. Koga M, Iguchi Y, Ohara T, Tahara Y, Fukuda T, Noguchi T, et al. Acute ischemic stroke as a complication of Stanford type A acute aortic dissection: a review and proposed clinical recommendations for urgent diagnosis. Gen Thorac Cardiovasc Surg. 2018; Aug. 66(8):439–45.5. Lee JY, Park JH, Jeon HJ, Yoon DY, Park SW, Cho BM. Transcervical access via direct neck exposure for neurointerventional procedures in the hybrid angiosuite. Neuroradiology. 2018; May. 60(5):565–73.6. Lu C, Lin Y, Chu H, Tang S, Lee C. Safety and efficacy of the transbrachial approach for endovascular thrombectomy in patients with acute large vessel occlusion stroke. J Formos Med Assoc. 2021; Jan. 120(1 Pt 3):705–12.7. Mendes A, Mendonça T, Sousa A, Moreira G, Carvalho M. Stroke secondary to aortic dissection treated with a thrombolytic: a successful case. Neurol Sci. 2012; Feb. 33(1):107–10.8. Mészáros I, Mórocz J, Szlávi J, Schmidt J, Tornóci L, Nagy L, et al. Epidemiology and clinicopathology of aortic dissection. Chest. 2000; May. 117(5):1271–8.9. Reznik ME, Espinosa-Morales AD, Jumaa MA, Zaidi S, Ducruet AF, Jadhav AP. Endovascular thrombectomy in the setting of aortic dissection. J Neurointerv Surg. 2017; Jan. 9(1):17–20.10. Sakamoto Y, Koga M, Ohara T, Ohyama S, Matsubara S, Minatoya K, et al. Frequency and detection of Stanford type a aortic dissection in hyperacute stroke management. Cerebrovasc Dis. 2016; 42(1-2):110–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Update of Recent Guideline for the Endovascular Recanalization Therapy in Acute Ischemic Stroke
- Previous and Recent Evidence of Endovascular Therapy in Acute Ischemic Stroke
- Painless Aortic Dissection Presenting as Acute Ischemic Stroke: Administ-ra-tion of Tissue lasminogen Activator
- Recanalization Outcomes and Procedural Complications in Patients With Acute Ischemic Stroke and COVID-19 Receiving Endovascular Treatment
- Placement of Endovascular Stent Graft in Acute Malperfusion Syndrome After Acute Type II Aortic Dissection