J Korean Neurosurg Soc.
2023 Sep;66(5):582-590. 10.3340/jkns.2022.0024.
Predictors of Outcome in Management of Paediatric Head Trauma in a Tertiary Healthcare Institution in North-Central Nigeria
- Affiliations
-
- 1Division of Neurosurgery, Department of Surgery, Jos University Teaching Hospital, Jos, Nigeria
- 2Division of Paediatric Surgery, Department of Surgery, Jos University Teaching Hospital, Jos, Nigeria
- 3The Loyal and Edith Davis Neurosurgical Research Laboratory, Department of Neurosurgery, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, AZ, USA
- 4Division of Trauma Surgery, Department of Surgery, Jos University Teaching Hospital, Jos, Nigeria
- KMID: 2545349
- DOI: http://doi.org/10.3340/jkns.2022.0024
Abstract
Objective
: Trauma is a leading causes of death and disability in all ages. The aim of this study was to describe the demography and characteristics of paediatric head trauma in our institution and examine the predictors of outcome and incidence of injury related mortality.
Methods
: We examined our institutional Trauma Registry over a 2 year period.
Results
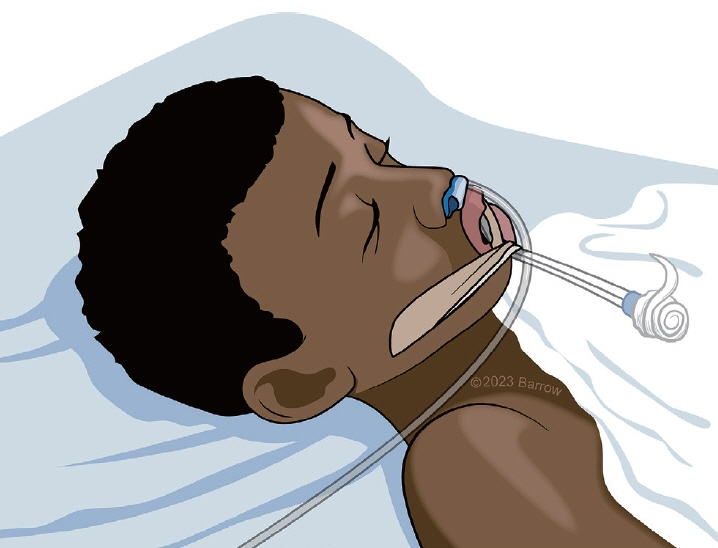
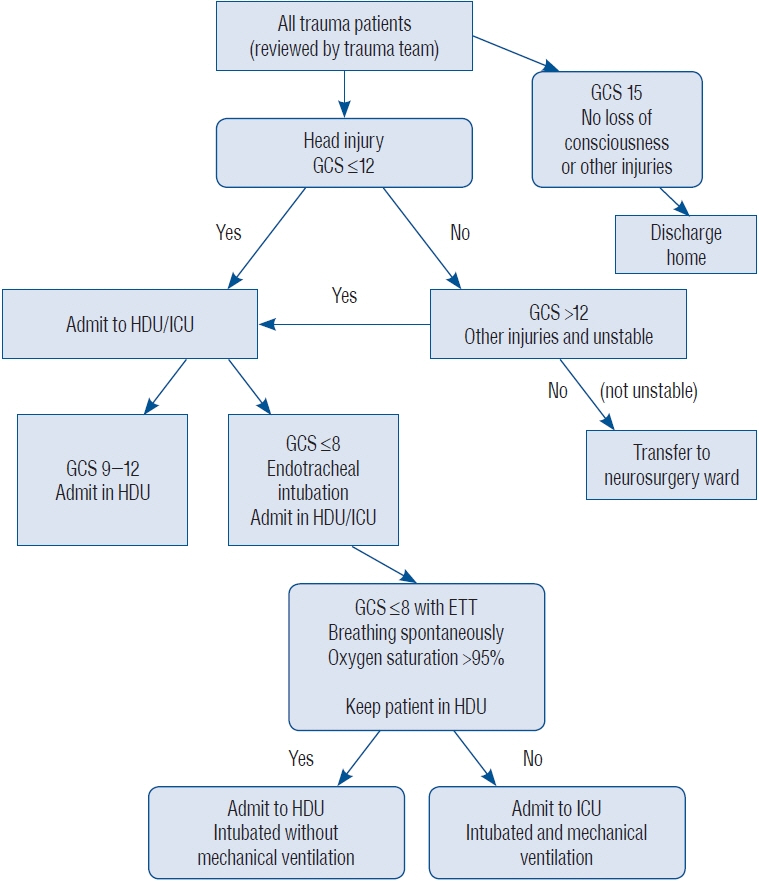
: A total of 1100 trauma patients were seen over the study period. Of the 579 patients who had head injury 99 were in the paediatric age group. Of the paediatric head trauma patients 79 had documented Glasgow coma score (GCS), 38 (48.1%), 17 (21.5%) and 24 (30.4%) had mild, moderate and severe head injury respectively. The percentage mortality of head injury in the paediatric age group was 6.06% (6/99). There is an association between mortality and GCS (p=0.008), necessity for intensive care unit (ICU) admission (p=0.0001), associated burns (p=0.0001) and complications such as aspiration pneumonia (p=0.0001). The significant predictors of outcome are aspiration (p=0.004), the need for ICU admission (p=0.0001) and associated burns (p=0.005) using logistic binary regression. During the study period 46 children underwent surgical intervention with extradural haematoma 16 (34.8%), depressed skull fracture 14 (30.4%) and chronic subdural haematoma five (10.9%) being the commonest indication for surgeries.
Conclusion
: Paediatric head injury accounted for 9.0% (99/1100) of all trauma admissions. Majority of patients had mild or moderate injuries. Burns, aspiration pneumonitis and the need for ICU admission were important predictors of outcome in children with traumatic brain injury.
Keyword
Figure
Reference
-
References
1. Adelson PD, Kochanek PM. Head injury in children. J Child Neurol. 13:2–15. 1998.2. Agrawal A, Agrawal CS, Kumar A, Lewis O, Malla G, Khatiwada R, et al. Epidemiology and management of paediatric head injury in Eastern Nepal. Afr J Paediatr Surg. 5:15–18. 2008.3. Bell MJ, Adelson PD, Wisniewski SR; Investigators of the ADAPT Study. Challenges and opportunities for pediatric severe TBI-review of the evidence and exploring a way forward. Childs Nerv Syst. 33:1663–1667. 2017.4. Chinda JY, Abubakar AM, Umaru H, Tahir C, Adamu S, Wabada S. Epidemiology and management of head injury in paediatric age group in North-Eastern Nigeria. Afr J Paediatr Surg. 10:358–361. 2013.5. Coronado VG, Xu L, Basavaraju SV, McGuire LC, Wald MM, Faul MD, et al. Surveillance for traumatic brain injury-related deaths--United States, 1997-2007. MMWR Surveill Summ. 60:1–32. 2011.6. Dewan MC, Mummareddy N, Wellons JC 3rd, Bonfield CM. Epidemiology of global pediatric traumatic brain injury: qualitative review. World Neurosurg. 91:497–509.e1. 2016.7. Emejulu JK, Shokunbi MT. Aetiological patterns and management outcome of paediatric head trauma: one-year prospective study. Niger J Clin Pract. 13:276–279. 2010.8. Kochanek PM, Tasker RC, Bell MJ, Adelson PD, Carney N, Vavilala MS, et al. Management of pediatric severe traumatic brain injury: 2019 consensus and guidelines-based algorithm for first and second tier therapies. Pediatr Crit Care Med. 20:269–279. 2019.9. Nnadi MO, Bankole OB, Fente BG. Epidemiology and treatment outcome of head injury in children: a prospective study. J Pediatr Neurosci. 9:237–241. 2014.10. Odebode TO, Abubakar AM. Childhood head injury: causes, outcome, and outcome predictors. A Nigerian perspective. Pediatr Surg Int. 20:348–352. 2004.11. Osifo OD, Iribhogbe PE, Ugiagbe EE. Epidemiology and pattern of paediatric and adolescent trauma deaths in a level 1 trauma centre in Benin city, Nigeria. Injury. 43:1861–1864. 2012.12. Shi J, Xiang H, Wheeler K, Smith GA, Stallones L, Groner J, et al. Costs, mortality likelihood and outcomes of hospitalized US children with traumatic brain injuries. Brain Inj. 23:602–611. 2009.13. Stanley RM, Bonsu BK, Zhao W, Ehrlich PF, Rogers AJ, Xiang H. US estimates of hospitalized children with severe traumatic brain injury: implications for clinical trials. Pediatrics. 129:e24–e30. 2012.14. Udoh DO, Adeyemo AA. Traumatic brain injuries in children: a hospitalbased study in Nigeria. Afr J Paediatr Surg. 10:154–159. 2013.15. Vaghani G, Singh PK, Gupta DK, Agrawal D, Sinha S, Satyarthee G, et al. Outcome of patients with traumatic head injury in infants: an institutional experience at level 1 trauma center. J Pediatr Neurosci. 8:104–107. 2013.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence and materno-fetal outcomes of preeclampsia/eclampsia amongst pregnant women at a teaching hospital in northcentral Nigeria: a retrospective crosssectional study
- Polyethylene Glycol Plus Electrolytes with Stimulant Laxative in Paediatric Faecal Disimpaction: A Randomised Controlled Study
- Myositis ossificans of the platysma mimicking a malignancy: a case report with review of the literature
- Pattern and Predictors of Sexual Activity among Postmenopausal Women Attending a Family Medicine Clinic in Ilorin, North-Central Nigeria
- Blunt Trauma Pancreas in Children: Is Non-Operative Management Appropriate for All Grades?