Korean J Gastroenterol.
2023 Aug;82(2):73-83. 10.4166/kjg.2023.079.
Impact of Diet on Colorectal Cancer Progression and Prevention: From Nutrients to Neoplasms
- Affiliations
-
- 1Department of Internal Medicine, Dongguk University Ilsan Hospital, Dongguk University College of Medicine, Goyang, Korea
- KMID: 2545331
- DOI: http://doi.org/10.4166/kjg.2023.079
Abstract
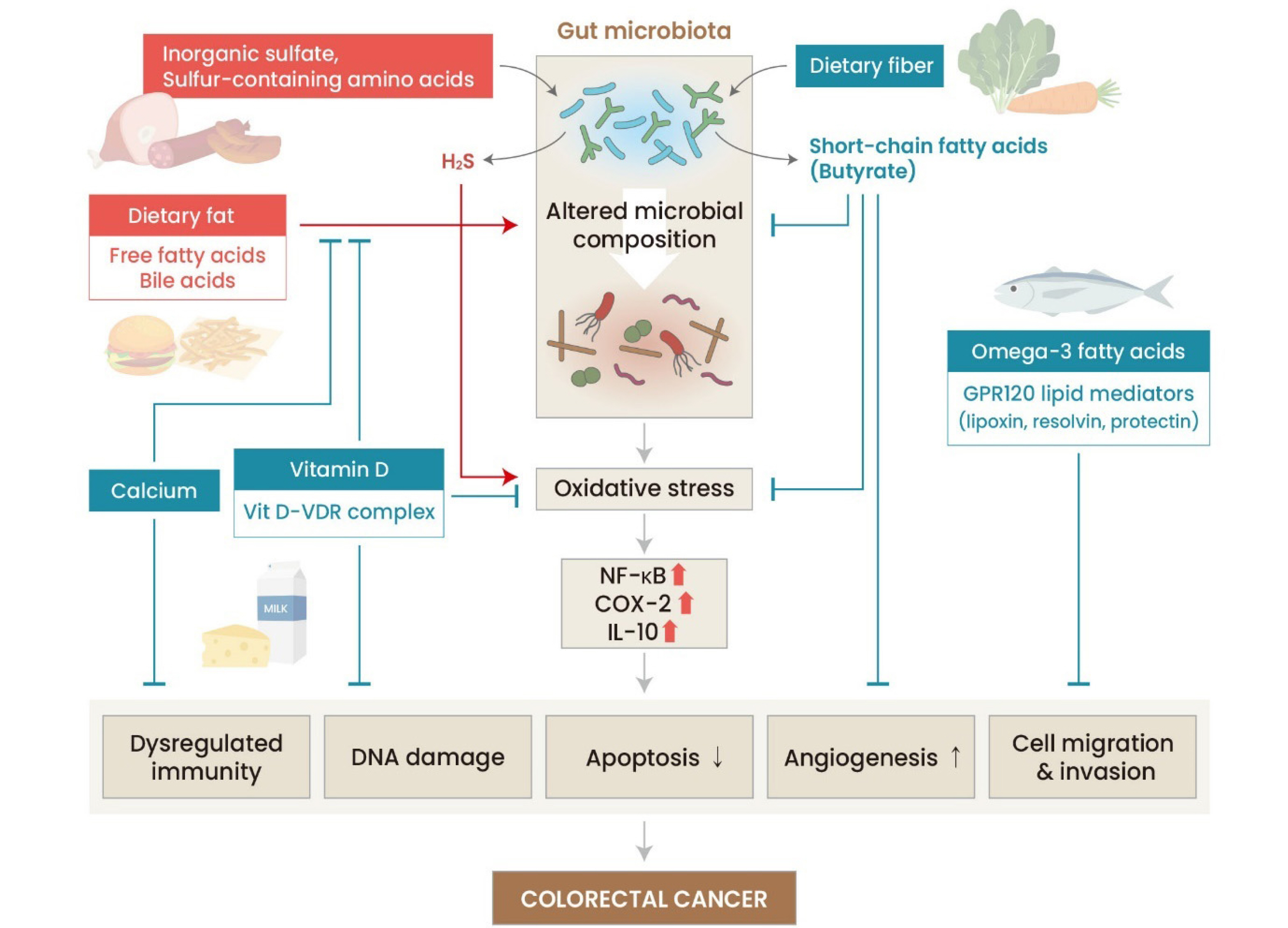
- Colorectal cancer (CRC), one of the most common cancers worldwide, continues to increase in incidence and mortality rates. This trend is closely linked to changes in dietary habits, which are major risk factors for colorectal cancer. The increase in the incidence of CRC in countries previously considered low-risk and with low socioeconomic status is most likely due to lifestyle and dietary changes. Understanding the influence of dietary factors on the onset of colorectal cancer is essential for prevention and treatment. This review explores the complex interplay between dietary factors and colorectal cancer, focusing on the key nutrients and dietary habits that influence disease onset and progression. The impact of diet on colorectal microbiota and the influence of diet on early-onset colorectal cancer are also reviewed, reviewing recent research on how dietary interventions affect the treatment and recurrence of colorectal cancer. Finally, the future research directions for developing and applying effective dietary intervention strategies are discussed.
Figure
Reference
-
1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021; 71:209–249. DOI: 10.3322/caac.21660. PMID: 33538338.
Article2. Siegel RL, Miller KD, Goding Sauer A, et al. 2020; Colorectal cancer statistics, 2020. CA Cancer J Clin. 70:145–164. DOI: 10.3322/caac.21601. PMID: 32133645.
Article3. Diet, nutrition, physical activity and cancer: a global perspective. Continuous Update Project Expert Report 2018. [Internet]. World Cancer Research Fund/American Institute for Cancer Research;2018. cited 2023 Jun 19. Available from: https://www.wcrf.org/wp-content/uploads/2021/02/Summary-of-Third-Expert-Report-2018.pdf.4. Doll R, Peto R. 1981; The causes of cancer: quantitative estimates of avoidable risks of cancer in the United States today. J Natl Cancer Inst. 66:1191–1308. DOI: 10.1093/jnci/66.6.1192. PMID: 7017215.
Article5. Keum N, Giovannucci E. 2019; Global burden of colorectal cancer: emerging trends, risk factors and prevention strategies. Nat Rev Gastroenterol Hepatol. 16:713–732. DOI: 10.1038/s41575-019-0189-8. PMID: 31455888.6. Song M, Garrett WS, Chan AT. 2015; Nutrients, foods, and colorectal cancer prevention. Gastroenterology. 148:1244–1260.e16. DOI: 10.1053/j.gastro.2014.12.035. PMID: 25575572. PMCID: PMC4409470.7. Newmark HL, Yang K, Kurihara N, Fan K, Augenlicht LH, Lipkin M. 2009; Western-style diet-induced colonic tumors and their modulation by calcium and vitamin D in C57Bl/6 mice: a preclinical model for human sporadic colon cancer. Carcinogenesis. 30:88–92. DOI: 10.1093/carcin/bgn229. PMID: 19017685. PMCID: PMC2722141.8. Fedirko V, Bostick RM, Long Q, et al. 2010; Effects of supplemental vitamin D and calcium on oxidative DNA damage marker in normal colorectal mucosa: a randomized clinical trial. Cancer Epidemiol Biomarkers Prev. 19:280–291. DOI: 10.1158/1055-9965.EPI-09-0448. PMID: 20056649. PMCID: PMC2805163.9. Ahearn TU, Shaukat A, Flanders WD, Rutherford RE, Bostick RM. 2012; A randomized clinical trial of the effects of supplemental calcium and vitamin D3 on the APC/β-catenin pathway in the normal mucosa of colorectal adenoma patients. Cancer Prev Res (Phila). 5:1247–1256. DOI: 10.1158/1940-6207.CAPR-12-0292. PMID: 22964475. PMCID: PMC3466388.
Article10. Cheng SX, Lightfoot YL, Yang T, et al. 2014; Epithelial CaSR deficiency alters intestinal integrity and promotes proinflammatory immune responses. FEBS Lett. 588:4158–4166. DOI: 10.1016/j.febslet.2014.05.007. PMID: 24842610. PMCID: PMC4234694.
Article11. Garland CF, Garland FC. 1980; Do sunlight and vitamin D reduce the likelihood of colon cancer? Int J Epidemiol. 9:227–231. DOI: 10.1093/ije/9.3.227. PMID: 7440046.
Article12. Jacobs ET, Hibler EA, Lance P, Sardo CL, Jurutka PW. 2013; Association between circulating concentrations of 25(OH)D and colorectal adenoma: a pooled analysis. Int J Cancer. 133:2980–2988. DOI: 10.1002/ijc.28316. PMID: 23754630. PMCID: PMC3797158.
Article13. Li M, Chen P, Li J, Chu R, Xie D, Wang H. 2014; Review: the impacts of circulating 25-hydroxyvitamin D levels on cancer patient outcomes: a systematic review and meta-analysis. J Clin Endocrinol Metab. 99:2327–2336. DOI: 10.1210/jc.2013-4320. PMID: 24780061.
Article14. Deeb KK, Trump DL, Johnson CS. 2007; Vitamin D signalling pathways in cancer: potential for anticancer therapeutics. Nat Rev Cancer. 7:684–700. DOI: 10.1038/nrc2196. PMID: 17721433.
Article15. Burkitt DP. 1971; Epidemiology of cancer of the colon and rectum. Cancer. 28:3–13. DOI: 10.1002/1097-0142(197107)28:1<3::AID-CNCR2820280104>3.0.CO;2-N. PMID: 5165022.
Article16. Bergman EN. 1990; Energy contributions of volatile fatty acids from the gastrointestinal tract in various species. Physiol Rev. 70:567–590. DOI: 10.1152/physrev.1990.70.2.567. PMID: 2181501.
Article17. Hamer HM, Jonkers D, Venema K, Vanhoutvin S, Troost FJ, Brummer RJ. 2008; Review article: the role of butyrate on colonic function. Aliment Pharmacol Ther. 27:104–119. DOI: 10.1111/j.1365-2036.2007.03562.x. PMID: 17973645.
Article18. Neish AS. 2009; Microbes in gastrointestinal health and disease. Gastroenterology. 136:65–80. DOI: 10.1053/j.gastro.2008.10.080. PMID: 19026645. PMCID: PMC2892787.
Article19. Manzi L, Costantini L, Molinari R, Merendino N. 2015; Effect of dietary ω-3 polyunsaturated fatty acid DHA on glycolytic enzymes and warburg phenotypes in cancer. Biomed Res Int. 2015:137097. DOI: 10.1155/2015/137097. PMID: 26339588. PMCID: PMC4538308.20. Lee JY, Sim TB, Lee JE, Na HK. 2017; Chemopreventive and chemotherapeutic effects of fish oil derived omega-3 polyunsaturated fatty acids on colon carcinogenesis. Clin Nutr Res. 6:147–160. DOI: 10.7762/cnr.2017.6.3.147. PMID: 28770178. PMCID: PMC5539209.
Article21. Zhao J, Dong JN, Wang HG, et al. 2017; Docosahexaenoic acid attenuated experimental chronic colitis in interleukin 10-deficient mice by enhancing autophagy through inhibition of the mTOR pathway. JPEN J Parenter Enteral Nutr. 41:824–829. DOI: 10.1177/0148607115609308. PMID: 26407598.
Article22. Simonetto M, Infante M, Sacco RL, Rundek T, Della-Morte D. 2019; A Novel anti-inflammatory role of omega-3 PUFAs in prevention and treatment of atherosclerosis and vascular cognitive impairment and dementia. Nutrients. 11:2279. DOI: 10.3390/nu11102279. PMID: 31547601. PMCID: PMC6835717.
Article23. Nguyen LH, Ma W, Wang DD, et al. 2020; Association between sulfur-metabolizing bacterial communities in stool and risk of distal colorectal cancer in men. Gastroenterology. 158:1313–1325. DOI: 10.1053/j.gastro.2019.12.029. PMID: 31972239. PMCID: PMC7384232.
Article24. Zhang W, An Y, Qin X, et al. 2021; Gut microbiota-derived metabolites in colorectal cancer: The bad and the challenges. Front Oncol. 11:739648. DOI: 10.3389/fonc.2021.739648. PMID: 34733783. PMCID: PMC8558397.
Article25. Prentice RL, Pettinger MB, Jackson RD, et al. 2013; Health risks and benefits from calcium and vitamin D supplementation: Women's Health Initiative clinical trial and cohort study. Osteoporos Int. 24:567–580. DOI: 10.1007/s00198-012-2224-2. PMID: 23208074. PMCID: PMC3557387.
Article26. Lee JE, Li H, Chan AT, et al. 2011; Circulating levels of vitamin D and colon and rectal cancer: the Physicians' Health Study and a meta-analysis of prospective studies. Cancer Prev Res (Phila). 4:735–743. DOI: 10.1158/1940-6207.CAPR-10-0289. PMID: 21430073. PMCID: PMC3412303.
Article27. Michels KB, Fuchs CS, Giovannucci E, et al. 2005; Fiber intake and incidence of colorectal cancer among 76,947 women and 47,279 men. Cancer Epidemiol Biomarkers Prev. 14:842–849. DOI: 10.1158/1055-9965.EPI-04-0544. PMID: 15824154.
Article28. Schatzkin A, Mouw T, Park Y, et al. 2007; Dietary fiber and whole-grain consumption in relation to colorectal cancer in the NIH-AARP Diet and Health Study. Am J Clin Nutr. 85:1353–1360. DOI: 10.1093/ajcn/85.5.1353. PMID: 17490973.
Article29. Park Y, Hunter DJ, Spiegelman D, et al. 2005; Dietary fiber intake and risk of colorectal cancer: a pooled analysis of prospective cohort studies. JAMA. 294:2849–2857. DOI: 10.1001/jama.294.22.2849. PMID: 16352792.30. Otani T, Iwasaki M, Ishihara J, Sasazuki S, Inoue M, Tsugane S. Japan Public Health Center-Based Prospective Study Group. 2006; Dietary fiber intake and subsequent risk of colorectal cancer: the Japan Public Health Center-based prospective study. Int J Cancer. 119:1475–1480. DOI: 10.1002/ijc.22007. PMID: 16642466.
Article31. Bonithon-Kopp C, Kronborg O, Giacosa A, Räth U, Faivre J. 2000; Calcium and fibre supplementation in prevention of colorectal adenoma recurrence: a randomised intervention trial. European Cancer Prevention Organisation Study Group. Lancet. 356:1300–1306. DOI: 10.1016/S0140-6736(00)02813-0. PMID: 11073017.
Article32. Alberts DS, Martínez ME, Roe DJ, et al. 2000; Lack of effect of a high-fiber cereal supplement on the recurrence of colorectal adenomas. Phoenix Colon Cancer Prevention Physicians' Network. N Engl J Med. 342:1156–1162. DOI: 10.1056/NEJM200004203421602. PMID: 10770980.
Article33. West NJ, Clark SK, Phillips RK, et al. 2010; Eicosapentaenoic acid reduces rectal polyp number and size in familial adenomatous polyposis. Gut. 59:918–925. DOI: 10.1136/gut.2009.200642. PMID: 20348368.
Article34. Aglago EK, Huybrechts I, Murphy N, et al. 2020; Consumption of fish and long-chain n-3 polyunsaturated fatty acids is associated with reduced risk of colorectal cancer in a large European cohort. Clin Gastroenterol Hepatol. 18:654–666.e6. DOI: 10.1016/j.cgh.2019.06.031. PMID: 31252190.
Article35. Hull MA, Sprange K, Hepburn T, et al. 2018; Eicosapentaenoic acid and aspirin, alone and in combination, for the prevention of colorectal adenomas (seAFOod Polyp Prevention trial): a multicentre, randomised, double-blind, placebo-controlled, 2 × 2 factorial trial. Lancet. 392:2583–2594. DOI: 10.1016/S0140-6736(18)31775-6. PMID: 30466866.
Article36. Cockbain AJ, Volpato M, Race AD, et al. 2014; Anticolorectal cancer activity of the omega-3 polyunsaturated fatty acid eicosapentaenoic acid. Gut. 63:1760–1768. DOI: 10.1136/gutjnl-2013-306445. PMID: 24470281.
Article37. Song M, Chan AT, Fuchs CS, et al. 2014; Dietary intake of fish, ω-3 and ω-6 fatty acids and risk of colorectal cancer: A prospective study in U.S. men and women. Int J Cancer. 135:2413–2423. DOI: 10.1002/ijc.28878. PMID: 24706410. PMCID: PMC4159425.
Article38. Chamberland JP, Moon HS. 2015; Down-regulation of malignant potential by alpha linolenic acid in human and mouse colon cancer cells. Fam Cancer. 14:25–30. DOI: 10.1007/s10689-014-9762-z. PMID: 25336096.
Article39. Magee EA, Richardson CJ, Hughes R, Cummings JH. 2000; Contribution of dietary protein to sulfide production in the large intestine: an in vitro and a controlled feeding study in humans. Am J Clin Nutr. 72:1488–1494. DOI: 10.1093/ajcn/72.6.1488. PMID: 11101476.
Article40. Jowett SL, Seal CJ, Pearce MS, et al. 2004; Influence of dietary factors on the clinical course of ulcerative colitis: a prospective cohort study. Gut. 53:1479–1484. DOI: 10.1136/gut.2003.024828. PMID: 15361498. PMCID: PMC1774231.
Article41. Pitcher MC, Beatty ER, Cummings JH. 2000; The contribution of sulphate reducing bacteria and 5-aminosalicylic acid to faecal sulphide in patients with ulcerative colitis. Gut. 46:64–72. DOI: 10.1136/gut.46.1.64. PMID: 10601057. PMCID: PMC1727787.
Article42. Attene-Ramos MS, Wagner ED, Gaskins HR, Plewa MJ. 2007; Hydrogen sulfide induces direct radical-associated DNA damage. Mol Cancer Res. 5:455–459. DOI: 10.1158/1541-7786.MCR-06-0439. PMID: 17475672.
Article43. Untereiner AA, Oláh G, Módis K, Hellmich MR, Szabo C. 2017; H2S-induced S-sulfhydration of lactate dehydrogenase a (LDHA) stimulates cellular bioenergetics in HCT116 colon cancer cells. Biochem Pharmacol. 136:86–98. DOI: 10.1016/j.bcp.2017.03.025. PMID: 28404377. PMCID: PMC5494970.
Article44. Rose P, Moore PK, Ming SH, Nam OC, Armstrong JS, Whiteman M. 2005; Hydrogen sulfide protects colon cancer cells from chemopreventative agent beta-phenylethyl isothiocyanate induced apoptosis. World J Gastroenterol. 11:3990–3997. DOI: 10.3748/wjg.v11.i26.3990. PMID: 15996021. PMCID: PMC4502092.
Article45. Milner JA. 1996; Garlic: its anticarcinogenic and antitumorigenic properties. Nutr Rev. 54(11 Pt 2):S82–86. DOI: 10.1111/j.1753-4887.1996.tb03823.x. PMID: 9110580.
Article46. Knowles LM, Milner JA. 2001; Possible mechanism by which allyl sulfides suppress neoplastic cell proliferation. J Nutr. 131(3s):1061S–1066S. DOI: 10.1093/jn/131.3.1061S. PMID: 11238817.
Article47. Smith TK, Lund EK, Johnson IT. 1998; Inhibition of dimethylhydrazineinduced aberrant crypt foci and induction of apoptosis in rat colon following oral administration of the glucosinolate sinigrin. Carcinogenesis. 19:267–273. DOI: 10.1093/carcin/19.2.267. PMID: 9498275.
Article48. Sender R, Fuchs S, Milo R. 2016; Are we really vastly outnumbered? revisiting the ratio of bacterial to host cells in humans. Cell. 164:337–340. DOI: 10.1016/j.cell.2016.01.013. PMID: 26824647.
Article49. Kau AL, Ahern PP, Griffin NW, Goodman AL, Gordon JI. 2011; Human nutrition, the gut microbiome and the immune system. Nature. 474:327–336. DOI: 10.1038/nature10213. PMID: 21677749. PMCID: PMC3298082.
Article50. Park CH, Eun CS, Han DS. 2018; Intestinal microbiota, chronic inflammation, and colorectal cancer. Intest Res. 16:338–345. DOI: 10.5217/ir.2018.16.3.338. PMID: 30090032. PMCID: PMC6077304.
Article51. Gagnière J, Raisch J, Veziant J, et al. 2016; Gut microbiota imbalance and colorectal cancer. World J Gastroenterol. 22:501–518. DOI: 10.3748/wjg.v22.i2.501. PMID: 26811603. PMCID: PMC4716055.
Article52. Yu LC, Wei SC, Ni YH. 2018; Impact of microbiota in colorectal carcinogenesis: lessons from experimental models. Intest Res. 16:346–357. DOI: 10.5217/ir.2018.16.3.346. PMID: 30090033. PMCID: PMC6077307.
Article53. Feng Q, Liang S, Jia H, et al. 2015; Gut microbiome development along the colorectal adenoma-carcinoma sequence. Nat Commun. 6:6528. DOI: 10.1038/ncomms7528. PMID: 25758642.
Article54. Arthur JC, Perez-Chanona E, Mühlbauer M, et al. 2012; Intestinal inflammation targets cancer-inducing activity of the microbiota. Science. 338:120–123. DOI: 10.1126/science.1224820. PMID: 22903521. PMCID: PMC3645302.
Article55. De Filippo C, Cavalieri D, Di Paola M, et al. 2010; Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc Natl Acad Sci U S A. 107:14691–14696. DOI: 10.1073/pnas.1005963107. PMID: 20679230. PMCID: PMC2930426.
Article56. Turnbaugh PJ, Ridaura VK, Faith JJ, Rey FE, Knight R, Gordon JI. 2009; The effect of diet on the human gut microbiome: a metagenomic analysis in humanized gnotobiotic mice. Sci Transl Med. 1:6ra14. DOI: 10.1126/scitranslmed.3000322. PMID: 20368178. PMCID: PMC2894525.
Article57. Kim SH, Lim YJ. 2022; The role of microbiome in colorectal carcinogenesis and its clinical potential as a target for cancer treatment. Intest Res. 20:31–42. DOI: 10.5217/ir.2021.00034. PMID: 34015206. PMCID: PMC8831768.
Article58. Stoffel EM, Murphy CC. 2020; Epidemiology and mechanisms of the increasing incidence of colon and rectal cancers in young adults. Gastroenterology. 158:341–353. DOI: 10.1053/j.gastro.2019.07.055. PMID: 31394082. PMCID: PMC6957715.
Article59. Chang DT, Pai RK, Rybicki LA, et al. 2012; Clinicopathologic and molecular features of sporadic early-onset colorectal adenocarcinoma: an adenocarcinoma with frequent signet ring cell differentiation, rectal and sigmoid involvement, and adverse morphologic features. Mod Pathol. 25:1128–1139. DOI: 10.1038/modpathol.2012.61. PMID: 22481281.
Article60. Connell LC, Mota JM, Braghiroli MI, Hoff PM. 2017; The rising incidence of younger patients with colorectal cancer: Questions about screening, biology, and treatment. Curr Treat Options Oncol. 18:23. DOI: 10.1007/s11864-017-0463-3. PMID: 28391421.
Article61. Zhang Q, Wang Y, Fu L. 2020; Dietary advanced glycation end-products: Perspectives linking food processing with health implications. Compr Rev Food Sci Food Saf. 19:2559–2587. DOI: 10.1111/1541-4337.12593. PMID: 33336972.
Article62. Albracht-Schulte K, Islam T, Johnson P, Moustaid-Moussa N. 2021; Systematic review of beef protein effects on gut microbiota: Implications for health. Adv Nutr. 12:102–114. DOI: 10.1093/advances/nmaa085. PMID: 32761179. PMCID: PMC7850003.
Article63. Zheng X, Hur J, Nguyen LH, et al. 2021; Comprehensive assessment of diet quality and risk of precursors of early-onset colorectal cancer. J Natl Cancer Inst. 113:543–552. DOI: 10.1093/jnci/djaa164. PMID: 33136160. PMCID: PMC8096368.
Article64. Krebs-Smith SM, Pannucci TE, Subar AF, et al. 2018; Update of the healthy eating index: HEI-2015. J Acad Nutr Diet. 118:1591–1602. DOI: 10.1016/j.jand.2018.05.021. PMID: 30146071. PMCID: PMC6719291.
Article65. Nguyen S, Li H, Yu D, et al. 2020; Adherence to dietary recommendations and colorectal cancer risk: results from two prospective cohort studies. Int J Epidemiol. 49:270–280. DOI: 10.1093/ije/dyz118. PMID: 31203367. PMCID: PMC7124505.
Article66. Morisseau C, Hammock BD. 2013; Impact of soluble epoxide hydrolase and epoxyeicosanoids on human health. Annu Rev Pharmacol Toxicol. 53:37–58. DOI: 10.1146/annurev-pharmtox-011112-140244. PMID: 23020295. PMCID: PMC3578707.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Corrigendum: Impact of Diet on Colorectal Cancer Progression and Prevention: From Nutrients to Neoplasms
- Dietary Intervention for Preventing Colorectal Cancer: A Practical Guide for Physicians
- Association between Diet-related Behaviour and Risk of Colorectal Cancer: A Scoping Review
- Nutritional Issues for Colorectal Cancer Prevention
- Gut Microbiome and Colorectal Cancer