Ann Rehabil Med.
2023 Aug;47(4):307-314. 10.5535/arm.23081.
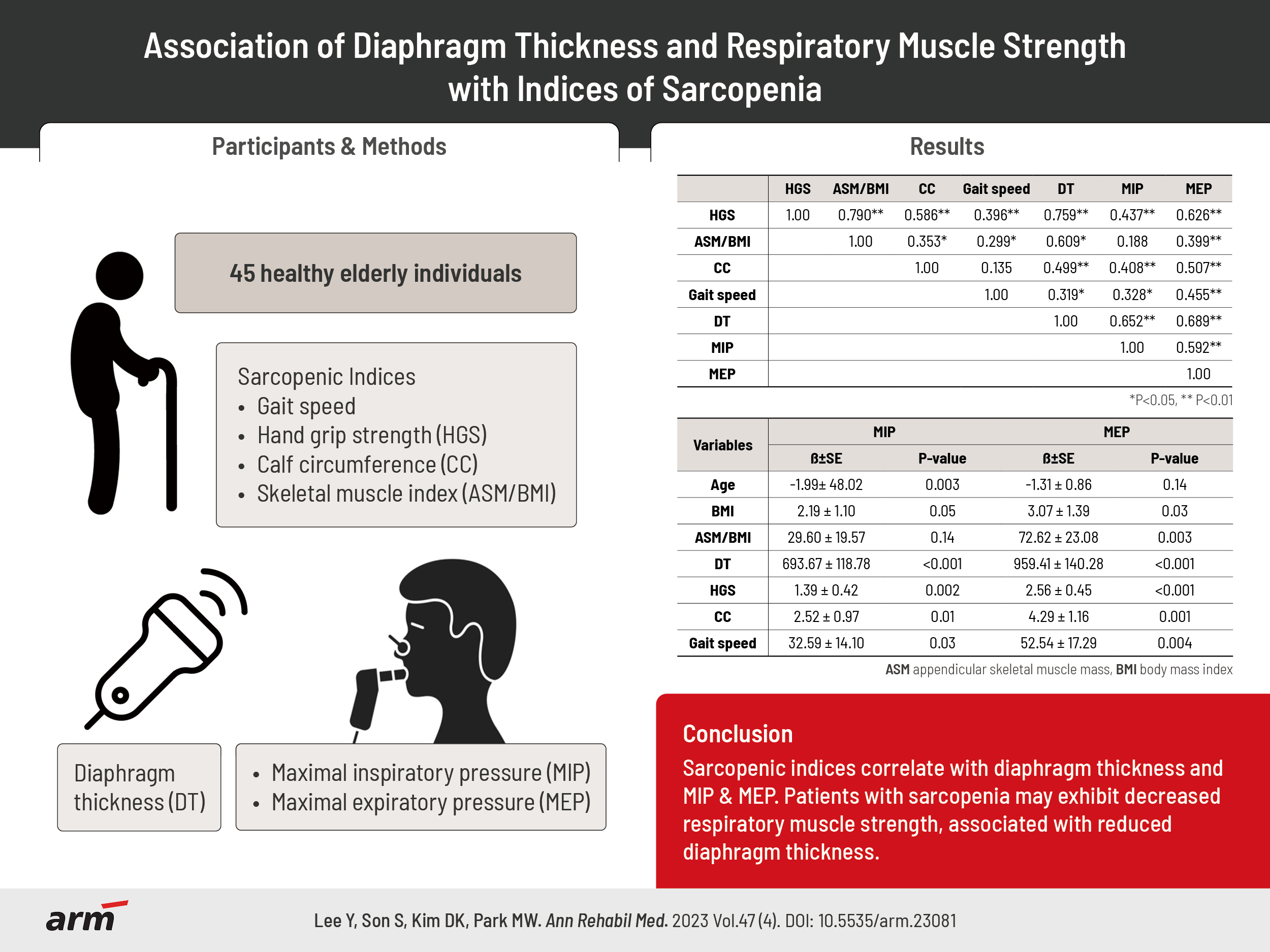
Association of Diaphragm Thickness and Respiratory Muscle Strength With Indices of Sarcopenia
- Affiliations
-
- 1Department of Physical and Rehabilitation Medicine, Chung-Ang University Gwangmyeong Hospital, Gwangmyeong, Korea
- 2Department of Physical and Rehabilitation Medicine, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea
- KMID: 2545327
- DOI: http://doi.org/10.5535/arm.23081
Abstract
Objective
To evaluate the relationship between respiratory muscle strength, diaphragm thickness (DT), and indices of sarcopenia.
Methods
This study included 45 healthy elderly volunteers (21 male and 24 female) aged 65 years or older. Sarcopenia indices, including hand grip strength (HGS) and body mass index-adjusted appendicular skeletal muscle (ASM/BMI), were measured using a hand grip dynamometer and bioimpedance analysis, respectively. Calf circumference (CC) and gait speed were also measured. Maximal inspiratory pressure (MIP) and maximal expiratory pressure (MEP) were obtained using a spirometer, as a measure of respiratory muscle strength. DT was evaluated through ultrasonography. The association between indices of sarcopenia, respiratory muscle strength, and DT was evaluated using Spearman’s rank correlation test, and univariate and multiple regression analysis.
Results
ASM/BMI (r=0.609, p<0.01), CC (r=0.499, p<0.01), HGS (r=0.759, p<0.01), and gait speed (r=0.319, p<0.05) were significantly correlated with DT. In the univariate linear regression analysis, MIP was significantly associated with age (p=0.003), DT (p<0.001), HGS (p=0.002), CC (p=0.013), and gait speed (p=0.026). MEP was significantly associated with sex (p=0.001), BMI (p=0.033), ASM/BMI (p=0.003), DT (p<0.001), HGS (p<0.001), CC (p=0.001) and gait speed (p=0.004). In the multiple linear regression analysis, age (p=0.001), DT (p<0.001), and ASM/BMI (p=0.008) showed significant association with MIP. DT (p<0.001) and gait speed (p=0.050) were associated with MEP.
Conclusion
Our findings suggest that respiratory muscle strength is associated with DT and indices of sarcopenia. Further prospective studies with larger sample sizes are needed to confirm these findings.
Keyword
Figure
Reference
-
1. Cruz-Jentoft AJ, Landi F, Topinková E, Michel JP. Understanding sarcopenia as a geriatric syndrome. Curr Opin Clin Nutr Metab Care. 2010; 13:1–7.
Article2. Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet 2019;393:2636-46. Erratum in: Lancet. 2019; 393:2590.3. Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019;48:16-31. Erratum in: Age Ageing. 2019; 48:601.4. Sheean PM, Peterson SJ, Gomez Perez S, Troy KL, Patel A, Sclamberg JS, et al. The prevalence of sarcopenia in patients with respiratory failure classified as normally nourished using computed tomography and subjective global assessment. JPEN J Parenter Enteral Nutr. 2014; 38:873–9.
Article5. Jeon YK, Shin MJ, Kim MH, Mok JH, Kim SS, Kim BH, et al. Low pulmonary function is related with a high risk of sarcopenia in community-dwelling older adults: the Korea National Health and Nutrition Examination Survey (KNHANES) 2008-2011. Osteoporos Int. 2015; 26:2423–9.
Article6. Okazaki T, Suzukamo Y, Miyatake M, Komatsu R, Yaekashiwa M, Nihei M, et al. Respiratory muscle weakness as a risk factor for pneumonia in older people. Gerontology. 2021; 67:581–90.
Article7. Menezes KK, Nascimento LR, Ada L, Polese JC, Avelino PR, Teixeira-Salmela LF. Respiratory muscle training increases respiratory muscle strength and reduces respiratory complications after stroke: a systematic review. J Physiother 2016;62:138-44. Erratum in: J Physiother. 2018; 64:73.
Article8. Goligher EC, Dres M, Fan E, Rubenfeld GD, Scales DC, Herridge MS, et al. Mechanical ventilation-induced diaphragm atrophy strongly impacts clinical outcomes. Am J Respir Crit Care Med. 2018; 197:204–13.
Article9. Deniz O, Coteli S, Karatoprak NB, Pence MC, Varan HD, Kizilarslanoglu MC, et al. Diaphragmatic muscle thickness in older people with and without sarcopenia. Aging Clin Exp Res. 2021; 33:573–80.
Article10. Cavayas YA, Eljaiek R, Rodrigue É, Lamarche Y, Girard M, Wang HT, et al. Preoperative diaphragm function is associated with postoperative pulmonary complications after cardiac surgery. Crit Care Med. 2019; 47:e966–74.
Article11. Sato S, Miyazaki S, Tamaki A, Yoshimura Y, Arai H, Fujiwara D, et al. Respiratory sarcopenia: a position paper by four professional organizations. Geriatr Gerontol Int. 2023; 23:5–15.
Article12. Le Neindre A, Philippart F, Luperto M, Wormser J, Morel-Sapene J, Aho SL, et al. Diagnostic accuracy of diaphragm ultrasound to predict weaning outcome: a systematic review and meta-analysis. Int J Nurs Stud. 2021; 117:103890.
Article13. Martínez-Arnau FM, Buigues C, Fonfría-Vivas R, Cauli O. Respiratory muscle strengths and their association with lean mass and handgrip strengths in older institutionalized individuals. J Clin Med. 2020; 9:2727.
Article14. Walter-Kroker A, Kroker A, Mattiucci-Guehlke M, Glaab T. A practical guide to bioelectrical impedance analysis using the example of chronic obstructive pulmonary disease. Nutr J. 2011; 10:35.
Article15. Cawthon PM, Peters KW, Shardell MD, McLean RR, Dam TT, Kenny AM, et al. Cutpoints for low appendicular lean mass that identify older adults with clinically significant weakness. J Gerontol A Biol Sci Med Sci. 2014; 69:567–75.
Article16. Bonnefoy M, Jauffret M, Kostka T, Jusot JF. Usefulness of calf circumference measurement in assessing the nutritional state of hospitalized elderly people. Gerontology. 2002; 48:162–9.
Article17. Innes E. Handgrip strength testing: a review of the literature. Aust Occup Ther J. 1999; 46:120–40.
Article18. Bianchi L, Ferrucci L, Cherubini A, Maggio M, Bandinelli S, Savino E, et al. The predictive value of the EWGSOP definition of sarcopenia: results from the InCHIANTI study. J Gerontol A Biol Sci Med Sci. 2016; 71:259–64.
Article19. Gomes-Neto M, Saquetto MB, Silva CM, Carvalho VO, Ribeiro N, Conceição CS. Effects of respiratory muscle training on respiratory function, respiratory muscle strength, and exercise tolerance in patients poststroke: a systematic review with meta-analysis. Arch Phys Med Rehabil. 2016; 97:1994–2001.
Article20. Bambra G, Jalota L, Kapoor C, Mills PK, Vempilly JJ, Jain VV. Office spirometry correlates with laboratory spirometry in patients with symptomatic asthma and COPD. Clin Respir J. 2017; 11:805–11.
Article21. American Thoracic Society (ATS)/European Respiratory Society (ERS). ATS/ERS statement on respiratory muscle testing. Am J Respir Crit Care Med. 2002; 166:518–624.22. De Bruin PF, Ueki J, Bush A, Khan Y, Watson A, Pride NB. Diaphragm thickness and inspiratory strength in patients with Duchenne muscular dystrophy. Thorax. 1997; 52:472–5.
Article23. Santana PV, Cardenas LZ, Albuquerque ALP, Carvalho CRR, Caruso P. Diaphragmatic ultrasound: a review of its methodological aspects and clinical uses. J Bras Pneumol. 2020; 46:e20200064.24. Kim M, Won CW. Sarcopenia in Korean community-dwelling adults aged 70 years and older: application of screening and diagnostic tools from the Asian Working Group for Sarcopenia 2019 update. J Am Med Dir Assoc. 2020; 21:752–8.25. Polla B, D'Antona G, Bottinelli R, Reggiani C. Respiratory muscle fibres: specialisation and plasticity. Thorax. 2004; 59:808–17.
Article26. Greising SM, Mantilla CB, Gorman BA, Ermilov LG, Sieck GC. Diaphragm muscle sarcopenia in aging mice. Exp Gerontol. 2013; 48:881–7.
Article27. Pollock RD, Rafferty GF, Moxham J, Kalra L. Respiratory muscle strength and training in stroke and neurology: a systematic review. Int J Stroke. 2013; 8:124–30.
Article28. Berlowitz DJ, Tamplin J. Respiratory muscle training for cervical spinal cord injury. Cochrane Database Syst Rev. 2013; (7):CD008507.
Article29. Silva IS, Pedrosa R, Azevedo IG, Forbes AM, Fregonezi GA, Dourado Junior ME, et al. Respiratory muscle training in children and adults with neuromuscular disease. Cochrane Database Syst Rev. 2019; 9:CD011711.
Article30. Shin HI, Kim DK, Seo KM, Kang SH, Lee SY, Son S. Relation between respiratory muscle strength and skeletal muscle mass and hand grip strength in the healthy elderly. Ann Rehabil Med. 2017; 41:686–92.
Article31. Ohara DG, Pegorari MS, Oliveira Dos Santos NL, de Fátima Ribeiro Silva C, Monteiro RL, Matos AP, et al. Respiratory muscle strength as a discriminator of sarcopenia in community-dwelling elderly: a cross-sectional study. J Nutr Health Aging. 2018; 22:952–8.
Article32. Summerhill EM, Angov N, Garber C, McCool FD. Respiratory muscle strength in the physically active elderly. Lung. 2007; 185:315–20.
Article33. Souza H, Rocha T, Pessoa M, Rattes C, Brandão D, Fregonezi G, et al. Effects of inspiratory muscle training in elderly women on respiratory muscle strength, diaphragm thickness and mobility. J Gerontol A Biol Sci Med Sci. 2014; 69:1545–53.
Article34. Sharma G, Goodwin J. Effect of aging on respiratory system physiology and immunology. Clin Interv Aging. 2006; 1:253–60.35. Ro HJ, Kim DK, Lee SY, Seo KM, Kang SH, Suh HC. Relationship between respiratory muscle strength and conventional sarcopenic indices in young adults: a preliminary study. Ann Rehabil Med. 2015; 39:880–7.36. Lear SA, Kohli S, Bondy GP, Tchernof A, Sniderman AD. Ethnic variation in fat and lean body mass and the association with insulin resistance. J Clin Endocrinol Metab. 2009; 94:4696–702.37. Hegewald MJ. Impact of obesity on pulmonary function: current understanding and knowledge gaps. Curr Opin Pulm Med. 2021; 27:132–40.38. Buckinx F, Reginster JY, Dardenne N, Croisiser JL, Kaux JF, Beaudart C, et al. Concordance between muscle mass assessed by bioelectrical impedance analysis and by dual energy X-ray absorptiometry: a cross-sectional study. BMC Musculoskelet Disord. 2015; 16:60.39. Nagano A, Wakabayashi H, Maeda K, Kokura Y, Miyazaki S, Mori T, et al. Respiratory sarcopenia and sarcopenic respiratory disability: concepts, diagnosis, and treatment. J Nutr Health Aging. 2021; 25:507–15.40. Yamada Y, Nishizawa M, Uchiyama T, Kasahara Y, Shindo M, Miyachi M, et al. Developing and validating an age-independent equation using multi-frequency bioelectrical impedance analysis for estimation of appendicular skeletal muscle mass and establishing a cutoff for sarcopenia. Int J Environ Res Public Health. 2017; 14:809.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship Between Respiratory Muscle Strength and Conventional Sarcopenic Indices in Young Adults: A Preliminary Study
- Sarcopenia of the Old Age
- Assessment of Muscle Quantity, Quality and Function
- Differences among skeletal muscle mass indices derived from height-, weight-, and body mass index-adjusted models in assessing sarcopenia
- Evaluating Postoperative Muscle Strength Using Surface Electromyography in Hip Fracture Patient