Clin Exp Otorhinolaryngol.
2023 Aug;16(3):201-216. 10.21053/ceo.2022.01361.
Clinical Practice Guideline: Clinical Efficacy of Nasal Surgery in the Treatment of Obstructive Sleep Apnea
- Affiliations
-
- 1Department of Otolaryngology, Ajou University School of Medicine, Suwon, Korea
- 2Department of Otorhinolaryngology-Head and Neck Surgery, Konkuk University School of Medicine, Seoul, Korea
- 3Department of Otorhinolaryngology-Head and Neck Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Otorhinolaryngology-Head and Neck Surgery, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea
- 5Department of Otorhinolaryngology-Head and Neck Surgery, Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea
- 6Department of Otorhinolaryngology, Gyeongsang National University College of Medicine, Jinju, Korea
- 7Department of Otorhinolaryngology-Head and Neck Surgery, Research Institute for Medical Science, Chungnam National University College of Medicine, Daejeon, Korea
- 8Department of Otolaryngology-Head and Neck Surgery, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 99Department of Otolaryngology-Head and Neck Surgery, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea
- 10Department of Otorhinolaryngology-Head and Neck Surgery, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 11Department of Otorhinolaryngology, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2545259
- DOI: http://doi.org/10.21053/ceo.2022.01361
Abstract
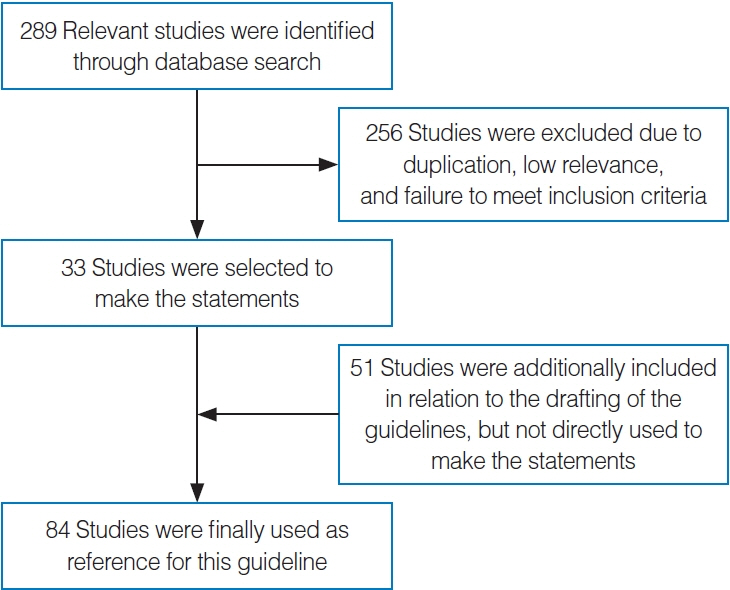
- Obstructive sleep apnea (OSA) is a common disorder characterized by upper airway obstruction during sleep. To reduce the morbidity of OSA, sleep specialists have explored various methods of managing the condition, including manifold positive airway pressure (PAP) techniques and surgical procedures. Nasal obstruction can cause significant discomfort during sleep, and it is likely that improving nasal obstruction would enhance the quality of life and PAP compliance of OSA patients. Many reliable studies have offered evidence to support this assumption. However, few comprehensive guidelines for managing OSA through nasal surgery encompass all this evidence. In order to address this gap, the Korean Society of Otorhinolaryngology-Head and Neck Surgery (KORL-HNS) and the Korean Society of Sleep and Breathing designated a guideline development group (GDG) to develop recommendations for nasal surgery in OSA patients. Several databases, including OVID Medline, Embase, the Cochrane Library, and KoreaMed, were searched to identify all relevant papers using a predefined search strategy. The types of nasal surgery included septoplasty, turbinate surgery, nasal valve surgery, septorhinoplasty, and endoscopic sinus surgery. When insufficient evidence was found, the GDG sought expert opinions and attempted to fill the evidence gap. Evidence-based recommendations for practice were ranked according to the American College of Physicians’ grading system. The GDG developed 10 key action statements with supporting text to support them. Three statements are ranked as strong recommendations, three are only recommendations, and four can be considered options. The GDG hopes that this clinical practice guideline will help physicians make optimal decisions when caring for OSA patients. Conversely, the statements in this guideline are not intended to limit or restrict physicians’ care based on their experience and assessment of individual patients.
Keyword
Figure
Reference
-
1. Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002; May. 165(9):1217–39.2. Donovan LM, Kapur VK. Prevalence and characteristics of central compared to obstructive sleep apnea: analyses from the Sleep Heart Health Study Cohort. Sleep. 2016; Jul. 39(7):1353–9.3. Aronson D, Nakhleh M, Zeidan-Shwiri T, Mutlak M, Lavie P, Lavie L. Clinical implications of sleep disordered breathing in acute myocardial infarction. PLoS One. 2014; Feb. 9(2):e88878.4. Azarbarzin A, Sands SA, Stone KL, Taranto-Montemurro L, Messineo L, Terrill PI, et al. The hypoxic burden of sleep apnoea predicts cardiovascular disease-related mortality: the Osteoporotic Fractures in Men Study and the Sleep Heart Health Study. Eur Heart J. 2019; Apr. 40(14):1149–57.5. Nieto FJ, Peppard PE, Young T, Finn L, Hla KM, Farre R. Sleep-disordered breathing and cancer mortality: results from the Wisconsin Sleep Cohort Study. Am J Respir Crit Care Med. 2012; Jul. 186(2):190–4.6. Veasey SC, Rosen IM. Obstructive sleep apnea in adults. N Engl J Med. 2019; Apr. 380(15):1442–9.7. Yaffe K, Laffan AM, Harrison SL, Redline S, Spira AP, Ensrud KE, et al. Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA. 2011; Aug. 306(6):613–9.8. Benjafield AV, Ayas NT, Eastwood PR, Heinzer R, Ip MS, Morrell MJ, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019; Aug. 7(8):687–98.9. Marshall NS, Wong KK, Cullen SR, Knuiman MW, Grunstein RR. Sleep apnea and 20-year follow-up for all-cause mortality, stroke, and cancer incidence and mortality in the Busselton Health Study cohort. J Clin Sleep Med. 2014; Apr. 10(4):355–62.10. Gurubhagavatula I, Patil S, Meoli A, Olson R, Sullivan S, Berneking M, et al. Sleep apnea evaluation of commercial motor vehicle operators. J Clin Sleep Med. 2015; Mar. 12(3):285–6.11. Kales SN, Czeisler CA. Obstructive sleep apnea and work accidents: time for action. Sleep. 2016; Jun. 39(6):1171–3.12. Epstein LJ, Kristo D, Strollo PJ Jr, Friedman N, Malhotra A, Patil SP, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009; Jun. 5(3):263–76.13. Kushida CA, Littner MR, Hirshkowitz M, Morgenthaler TI, Alessi CA, Bailey D, et al. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep. 2006; Mar. 29(3):375–80.14. Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc. 2008; Feb. 5(2):173–8.15. Weaver TE, Maislin G, Dinges DF, Bloxham T, George CF, Greenberg H, et al. Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep. 2007; Jun. 30(6):711–9.16. Sunwoo BY, Light M, Malhotra A. Strategies to augment adherence in the management of sleep-disordered breathing. Respirology. 2020; Apr. 25(4):363–71.17. Camacho M, Riaz M, Capasso R, Ruoff CM, Guilleminault C, Kushida CA, et al. The effect of nasal surgery on continuous positive airway pressure device use and therapeutic treatment pressures: a systematic review and meta-analysis. Sleep. 2015; Feb. 38(2):279–86.18. Wilhelm CP, deShazo RD, Tamanna S, Ullah MI, Skipworth LB. The nose, upper airway, and obstructive sleep apnea. Ann Allergy Asthma Immunol. 2015; Aug. 115(2):96–102.19. Friedman M, Maley A, Kelley K, Leesman C, Patel A, Pulver T, et al. Impact of nasal obstruction on obstructive sleep apnea. Otolaryngol Head Neck Surg. 2011; Jun. 144(6):1000–4.20. Young T, Finn L, Kim H; The University of Wisconsin Sleep and Respiratory Research Group. Nasal obstruction as a risk factor for sleep-disordered breathing. J Allergy Clin Immunol. 1997; Feb. 99(2):S757–62.21. Lofaso F, Coste A, d’Ortho MP, Zerah-Lancner F, Delclaux C, Goldenberg F, et al. Nasal obstruction as a risk factor for sleep apnoea syndrome. Eur Respir J. 2000; Oct. 16(4):639–43.22. Ryan CM, Bradley TD. Pathogenesis of obstructive sleep apnea. J Appl Physiol (1985). 2005; Dec. 99(6):2440–50.23. Ryan CF. Sleep • 9: an approach to treatment of obstructive sleep apnoea/hypopnoea syndrome including upper airway surgery. Thorax. 2005; Jul. 60(7):595–604.24. Fitzpatrick MF, McLean H, Urton AM, Tan A, O’Donnell D, Driver HS. Effect of nasal or oral breathing route on upper airway resistance during sleep. Eur Respir J. 2003; Nov. 22(5):827–32.25. Campos-Rodriguez F, Martinez-Garcia MA, de la Cruz-Moron I, Almeida-Gonzalez C, Catalan-Serra P, Montserrat JM. Cardiovascular mortality in women with obstructive sleep apnea with or without continuous positive airway pressure treatment: a cohort study. Ann Intern Med. 2012; Jan. 156(2):115–22.26. Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993; Apr. 328(17):1230–5.27. Kim J, In K, Kim J, You S, Kang K, Shim J, et al. Prevalence of sleep-disordered breathing in middle-aged Korean men and women. Am J Respir Crit Care Med. 2004; Nov. 170(10):1108–13.28. Knauert M, Naik S, Gillespie MB, Kryger M. Clinical consequences and economic costs of untreated obstructive sleep apnea syndrome. World J Otorhinolaryngol Head Neck Surg. 2015; Sep. 1(1):17–27.29. Albarrak M, Banno K, Sabbagh AA, Delaive K, Walld R, Manfreda J, et al. Utilization of healthcare resources in obstructive sleep apnea syndrome: a 5-year follow-up study in men using CPAP. Sleep. 2005; Oct. 28(10):1306–11.30. Berger MB, Sullivan W, Owen R, Wu C. A corporate driven sleep apnea detection and treatment program: results and challenges [Internet]. Precision Pulmonary Diagnostics; 2005 [cited 2023 Mar 16]. Available from: https://www.precisionpulmonary.com/articles/corporate_program/.31. Hoffman B, Wingenbach DD, Kagey AN, Schaneman JL, Kasper D. The long-term health plan and disability cost benefit of obstructive sleep apnea treatment in a commercial motor vehicle driver population. J Occup Environ Med. 2010; May. 52(5):473–7.32. Kapur V, Blough DK, Sandblom RE, Hert R, de Maine JB, Sullivan SD, et al. The medical cost of undiagnosed sleep apnea. Sleep. 1999; Sep. 22(6):749–55.33. Tarasiuk A, Greenberg-Dotan S, Brin YS, Simon T, Tal A, Reuveni H. Determinants affecting health-care utilization in obstructive sleep apnea syndrome patients. Chest. 2005; Sep. 128(3):1310–4.34. American Academy of Sleep Medicine. Hidden health crisis costing America billions: underdiagnosing and undertreating obstructive sleep apnea draining healthcare system. Frost & Sullivan;2016.35. Rosenfeld RM, Shiffman RN, Robertson P; Department of Otolaryngology State University of New York Downstate. Clinical practice guideline development manual, third edition: a quality-driven approach for translating evidence into action. Otolaryngol Head Neck Surg. 2013; Jan. 148(1 Suppl):S1–55.36. Morris LG, Burschtin O, Lebowitz RA, Jacobs JB, Lee KC. Nasal obstruction and sleep-disordered breathing: a study using acoustic rhinometry. Am J Rhinol. 2005; Jan-Feb. 19(1):33–9.37. Rimmer J, Hellings P, Lund VJ, Alobid I, Beale T, Dassi C, et al. European position paper on diagnostic tools in rhinology. Rhinology. 2019; Jul. 57(Suppl 28):1–41.38. Li HY, Lin Y, Chen NH, Lee LA, Fang TJ, Wang PC. Improvement in quality of life after nasal surgery alone for patients with obstructive sleep apnea and nasal obstruction. Arch Otolaryngol Head Neck Surg. 2008; Apr. 134(4):429–33.39. Park CY, Hong JH, Lee JH, Lee KE, Cho HS, Lim SJ, et al. Clinical effect of surgical correction for nasal pathology on the treatment of obstructive sleep apnea syndrome. PLoS One. 2014; Jun. 9(6):e98765.40. Wu J, Zhao G, Li Y, Zang H, Wang T, Wang D, et al. Apnea-hypopnea index decreased significantly after nasal surgery for obstructive sleep apnea: a meta-analysis. Medicine (Baltimore). 2017; Feb. 96(5):e6008.41. Mickelson SA. Nasal surgery for obstructive sleep apnea syndrome. Otolaryngol Clin North Am. 2016; Dec. 49(6):1373–81.42. Xiao Y, Han D, Zang H, Wang D. The effectiveness of nasal surgery on psychological symptoms in patients with obstructive sleep apnea and nasal obstruction. Acta Otolaryngol. 2016; Jun. 136(6):626–32.43. Kim SD, Jung DW, Lee JW, Park JH, Mun SJ, Cho KS. Relationship between allergic rhinitis and nasal surgery success in patients with obstructive sleep apnea. Am J Otolaryngol. 2021; Nov-Dec. 42(6):103079.44. Nakata S, Noda A, Yagi H, Yanagi E, Mimura T, Okada T, et al. Nasal resistance for determinant factor of nasal surgery in CPAP failure patients with obstructive sleep apnea syndrome. Rhinology. 2005; Dec. 43(4):296–9.45. Nakata S, Noda A, Yasuma F, Morinaga M, Sugiura M, Katayama N, et al. Effects of nasal surgery on sleep quality in obstructive sleep apnea syndrome with nasal obstruction. Am J Rhinol. 2008; Jan-Feb. 22(1):59–63.46. Uz U, Gunhan K, Yilmaz H, Unlu H. The evaluation of pattern and quality of sleep in patients with chronic rhinosinusitis with nasal polyps. Auris Nasus Larynx. 2017; Dec. 44(6):708–12.47. Tagaya M, Otake H, Suzuki K, Yasuma F, Yamamoto H, Noda A, et al. The comparison of nasal surgery and CPAP on daytime sleepiness in patients with OSAS. Rhinology. 2017; Sep. 55(3):269–73.48. Koutsourelakis I, Georgoulopoulos G, Perraki E, Vagiakis E, Roussos C, Zakynthinos SG. Randomised trial of nasal surgery for fixed nasal obstruction in obstructive sleep apnoea. Eur Respir J. 2008; Jan. 31(1):110–7.49. Bican A, Kahraman A, Bora I, Kahveci R, Hakyemez B. What is the efficacy of nasal surgery in patients with obstructive sleep apnea syndrome? J Craniofac Surg. 2010; Nov. 21(6):1801–6.50. Na Y, Kim YJ, Kim HY, Jung YG. Improvements in airflow characteristics and effect on the NOSE score after septoturbinoplasty: a computational fluid dynamics analysis. PLoS One. 2022; Nov. 17(11):e0277712.51. Cai Y, Goldberg AN, Chang JL. The nose and nasal breathing in sleep apnea. Otolaryngol Clin North Am. 2020; Jun. 53(3):385–95.52. Tosun F, Kemikli K, Yetkin S, Ozgen F, Durmaz A, Gerek M. Impact of endoscopic sinus surgery on sleep quality in patients with chronic nasal obstruction due to nasal polyposis. J Craniofac Surg. 2009; Mar. 20(2):446–9.53. Tajudeen BA, Brooks SG, Yan CH, Kuan EC, Schwartz JS, Suh JD, et al. Quality-of-life improvement after endoscopic sinus surgery in patients with obstructive sleep apnea. Allergy Rhinol (Providence). 2017; Mar. 8(1):25–31.54. Moxness MH, Nordgard S. An observational cohort study of the effects of septoplasty with or without inferior turbinate reduction in patients with obstructive sleep apnea. BMC Ear Nose Throat Disord. 2014; Oct. 14:11.55. Hisamatsu K, Kudo I, Makiyama K. The effect of compound nasal surgery on obstructive sleep apnea syndrome. Am J Rhinol Allergy. 2015; Nov-Dec. 29(6):e192–6.56. Choi JH, Kim EJ, Kim YS, Kim TH, Choi J, Kwon SY, et al. Effectiveness of nasal surgery alone on sleep quality, architecture, position, and sleep-disordered breathing in obstructive sleep apnea syndrome with nasal obstruction. Am J Rhinol Allergy. 2011; Sep-Oct. 25(5):338–41.57. Nourizadeh N, Rasoulian B, Majidi MR, Ardani AR, Rezaeitalab F, Asadpour H. Sleep quality after endoscopic sinus surgery in patients with sinonasal polyposis. Auris Nasus Larynx. 2019; Dec. 46(6):866–70.58. Li HY, Wang PC, Chen YP, Lee LA, Fang TJ, Lin HC. Critical appraisal and meta-analysis of nasal surgery for obstructive sleep apnea. Am J Rhinol Allergy. 2011; Jan-Feb. 25(1):45–9.59. Ishii L, Roxbury C, Godoy A, Ishman S, Ishii M. Does nasal surgery improve OSA in patients with nasal obstruction and OSA?: a meta-analysis. Otolaryngol Head Neck Surg. 2015; Sep. 153(3):326–33.60. Johnson DM, Soose RJ. Updated nasal surgery for obstructive sleep apnea. Adv Otorhinolaryngol. 2017; 80:66–73.61. Guttemberg MD, Mata FA, Nakanishi M, de Andrade KR, Pereira MG. Sleep quality assessment in chronic rhinosinusitis patients submitted to endoscopic sinus surgery: a meta-analysis. Braz J Otorhinolaryngol. 2019; Nov-Dec. 85(6):780–7.62. Wang M, Liu SY, Zhou B, Li Y, Cui S, Huang Q. Effect of nasal and sinus surgery in patients with and without obstructive sleep apnea. Acta Otolaryngol. 2019; May. 139(5):467–72.63. Victores AJ, Takashima M. Effects of nasal surgery on the upper airway: a drug-induced sleep endoscopy study. Laryngoscope. 2012; Nov. 122(11):2606–10.64. Virkkula P, Hytonen M, Bachour A, Malmberg H, Hurmerinta K, Salmi T, et al. Smoking and improvement after nasal surgery in snoring men. Am J Rhinol. 2007; Mar-Apr. 21(2):169–73.65. Deary V, Ellis JG, Wilson JA, Coulter C, Barclay NL. Simple snoring: not quite so simple after all? Sleep Med Rev. 2014; Dec. 18(6):453–62.66. Friedman M, Tanyeri H, Lim JW, Landsberg R, Vaidyanathan K, Caldarelli D. Effect of improved nasal breathing on obstructive sleep apnea. Otolaryngol Head Neck Surg. 2000; Jan. 122(1):71–4.67. Kakkar RK, Berry RB. Positive airway pressure treatment for obstructive sleep apnea. Chest. 2007; Sep. 132(3):1057–72.68. Kim ST, Choi JH, Jeon HG, Cha HE, Kim DY, Chung YS. Polysomnographic effects of nasal surgery for snoring and obstructive sleep apnea. Acta Otolaryngol. 2004; Apr. 124(3):297–300.69. Li HY, Lee LA, Wang PC, Chen NH, Lin Y, Fang TJ. Nasal surgery for snoring in patients with obstructive sleep apnea. Laryngoscope. 2008; Feb. 118(2):354–9.70. Li HY, Lee LA, Wang PC, Fang TJ, Chen NH. Can nasal surgery improve obstructive sleep apnea: subjective or objective? Am J Rhinol Allergy. 2009; Nov-Dec. 23(6):e51–5.71. Sufioglu M, Ozmen OA, Kasapoglu F, Demir UL, Ursavas A, Erisen L, et al. The efficacy of nasal surgery in obstructive sleep apnea syndrome: a prospective clinical study. Eur Arch Otorhinolaryngol. 2012; Feb. 269(2):487–94.72. Park DY, Kim JS, Park B, Kim HJ. Risk factors and clinical prediction formula for the evaluation of obstructive sleep apnea in Asian adults. PLoS One. 2021; Feb. 16(2):e0246399.73. Iwata N, Nakata S, Inada H, Kimura A, Hirata M, Yasuma F. Clinical indication of nasal surgery for the CPAP intolerance in obstructive sleep apnea with nasal obstruction. Auris Nasus Larynx. 2020; Dec. 47(6):1018–22.74. Yalamanchali S, Cipta S, Waxman J, Pott T, Joseph N, Friedman M. Effects of endoscopic sinus surgery and nasal surgery in patients with obstructive sleep apnea. Otolaryngol Head Neck Surg. 2014; Jul. 151(1):171–5.75. Series F, St Pierre S, Carrier G. Effects of surgical correction of nasal obstruction in the treatment of obstructive sleep apnea. Am Rev Respir Dis. 1992; Nov. 146(5 Pt 1):1261–5.76. Verse T, Maurer JT, Pirsig W. Effect of nasal surgery on sleep-related breathing disorders. Laryngoscope. 2002; Jan. 112(1):64–8.77. Virkkula P, Bachour A, Hytonen M, Salmi T, Malmberg H, Hurmerinta K, et al. Snoring is not relieved by nasal surgery despite improvement in nasal resistance. Chest. 2006; Jan. 129(1):81–7.78. Shuaib SW, Undavia S, Lin J, Johnson CM Jr, Stupak HD. Can functional septorhinoplasty independently treat obstructive sleep apnea? Plast Reconstr Surg. 2015; Jun. 135(6):1554–65.79. Mandour YM, Abo Youssef SM, Moussa HH. Polysomnographic and pulmonary function changes in patients with sleep problems after septoplasty with turbinectomy. Am J Otolaryngol. 2019; Mar-Apr. 40(2):187–90.80. In SM, Park DY, Lee KI, Gu G, Kim HJ. The effects of intermittent hypoxia on human nasal mucosa. Sleep Breath. 2021; Sep. 25(3):1453–60.81. Poirier J, George C, Rotenberg B. The effect of nasal surgery on nasal continuous positive airway pressure compliance. Laryngoscope. 2014; Jan. 124(1):317–9.82. Reilly EK, Boon MS, Vimawala S, Chitguppi C, Patel J, Murphy K, et al. Tolerance of continuous positive airway pressure after sinonasal surgery. Laryngoscope. 2021; Mar. 131(3):E1013–8.83. Zonato AI, Bittencourt LR, Martinho FL, Gregorio LC, Tufik S. Upper airway surgery: the effect on nasal continuous positive airway pressure titration on obstructive sleep apnea patients. Eur Arch Otorhinolaryngol. 2006; May. 263(5):481–6.84. Powell NB, Zonato AI, Weaver EM, Li K, Troell R, Riley RW, et al. Radiofrequency treatment of turbinate hypertrophy in subjects using continuous positive airway pressure: a randomized, double-blind, placebo-controlled clinical pilot trial. Laryngoscope. 2001; Oct. 111(10):1783–90.