Korean J Orthod.
2023 Jul;53(4):241-253. 10.4041/kjod23.036.
Skeletal and dentoalveolar effects of different types of microimplant-assisted rapid palatal expansion
- Affiliations
-
- 1Department of Orthodontics, College of Dentistry, Dankook University, Cheonan, Korea
- KMID: 2545040
- DOI: http://doi.org/10.4041/kjod23.036
Abstract
Objective
To evaluate the following null hypothesis: the skeletal and dentoalveolar expansion patterns in the coronal and axial planes are not different with two different types of microimplant-assisted rapid palatal expansion (MARPE) systems.
Methods
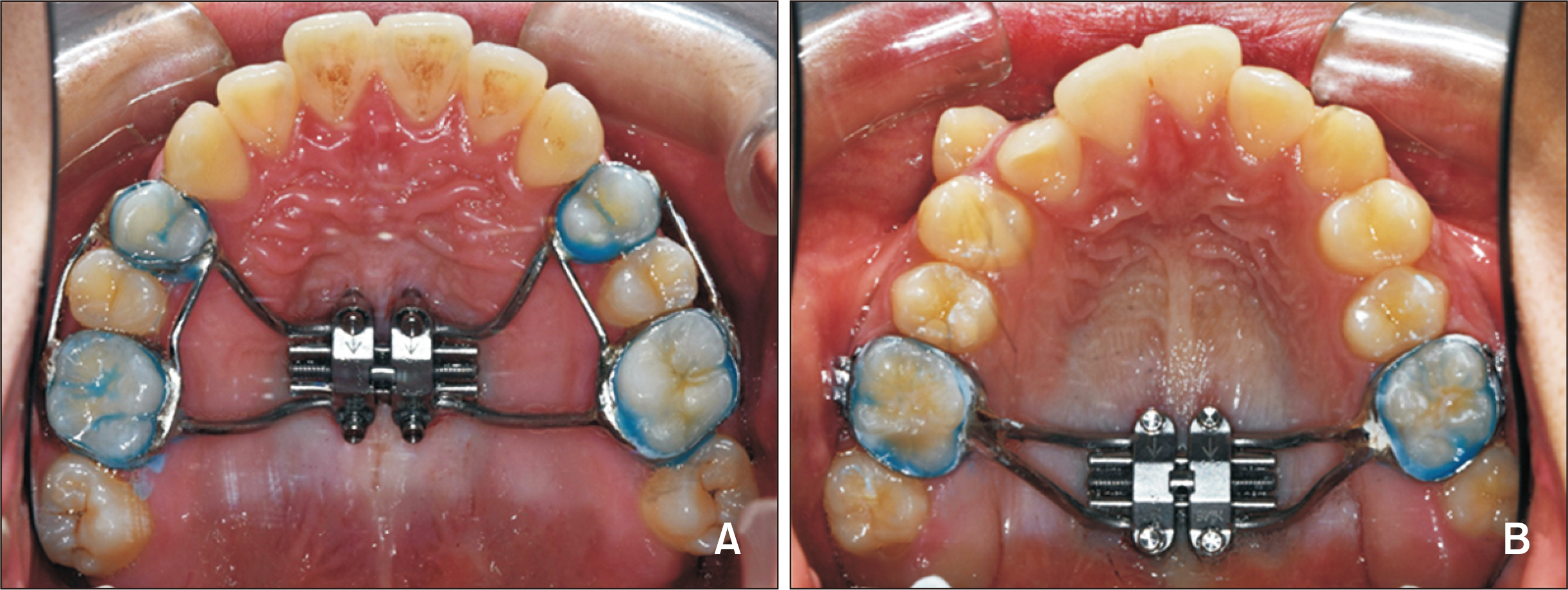
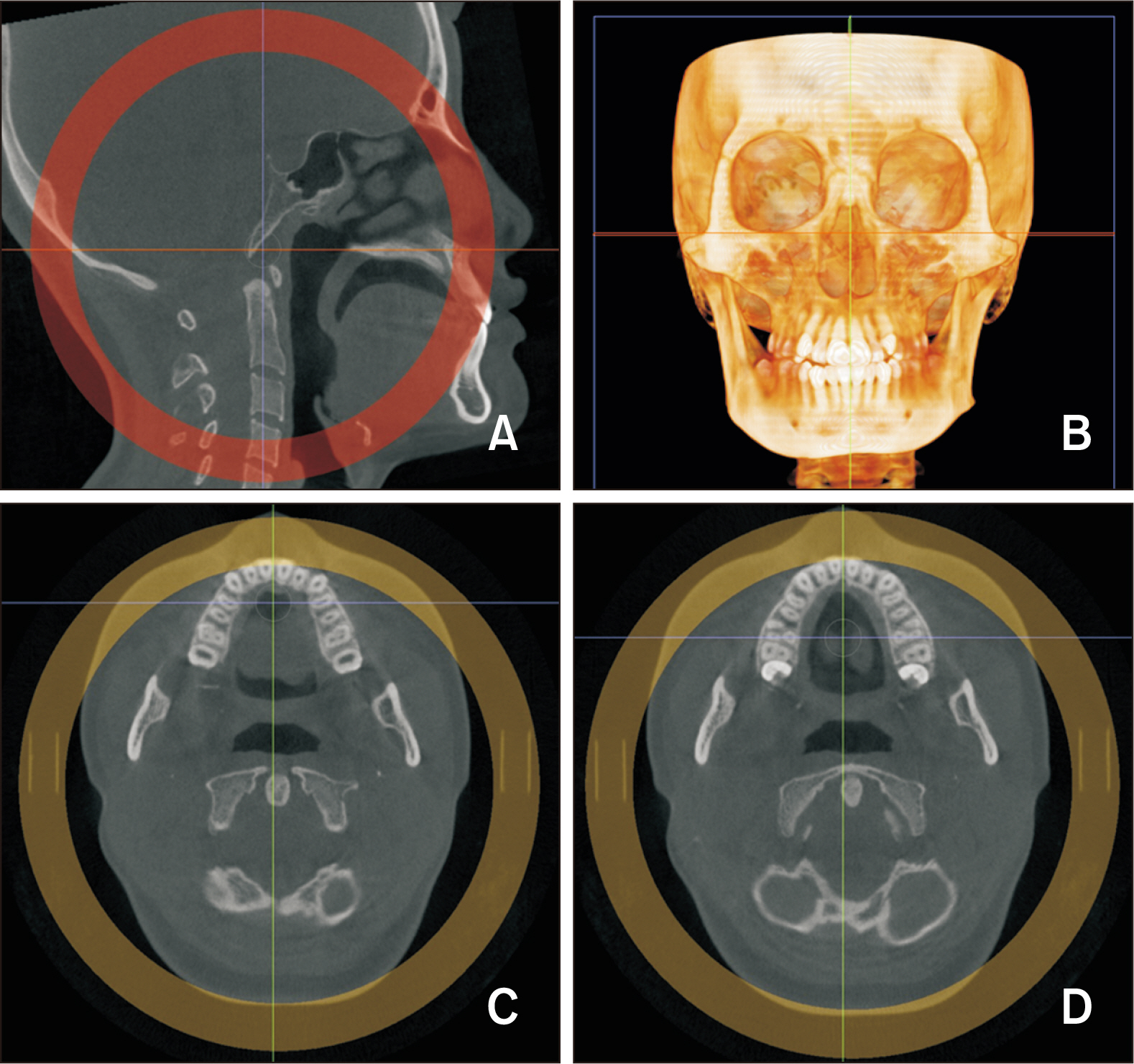
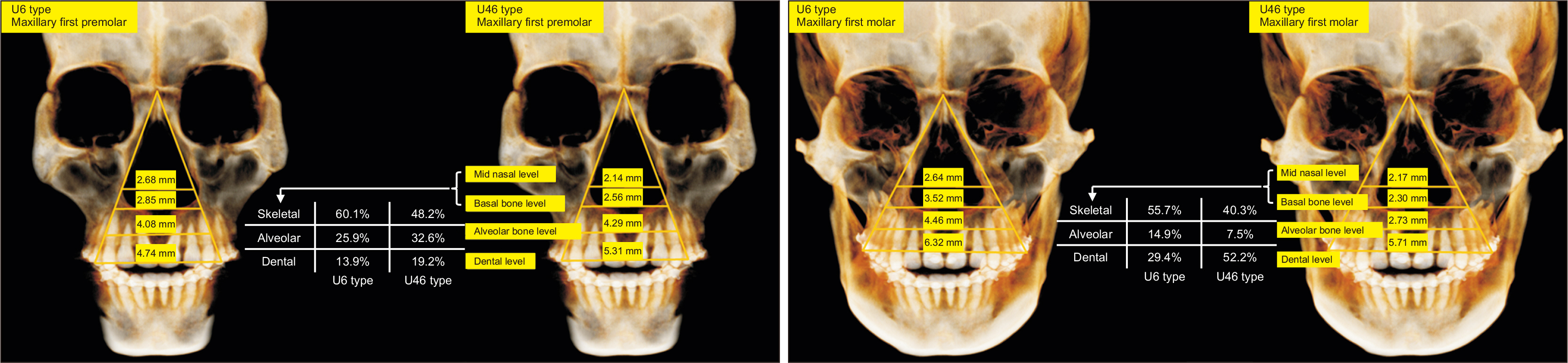
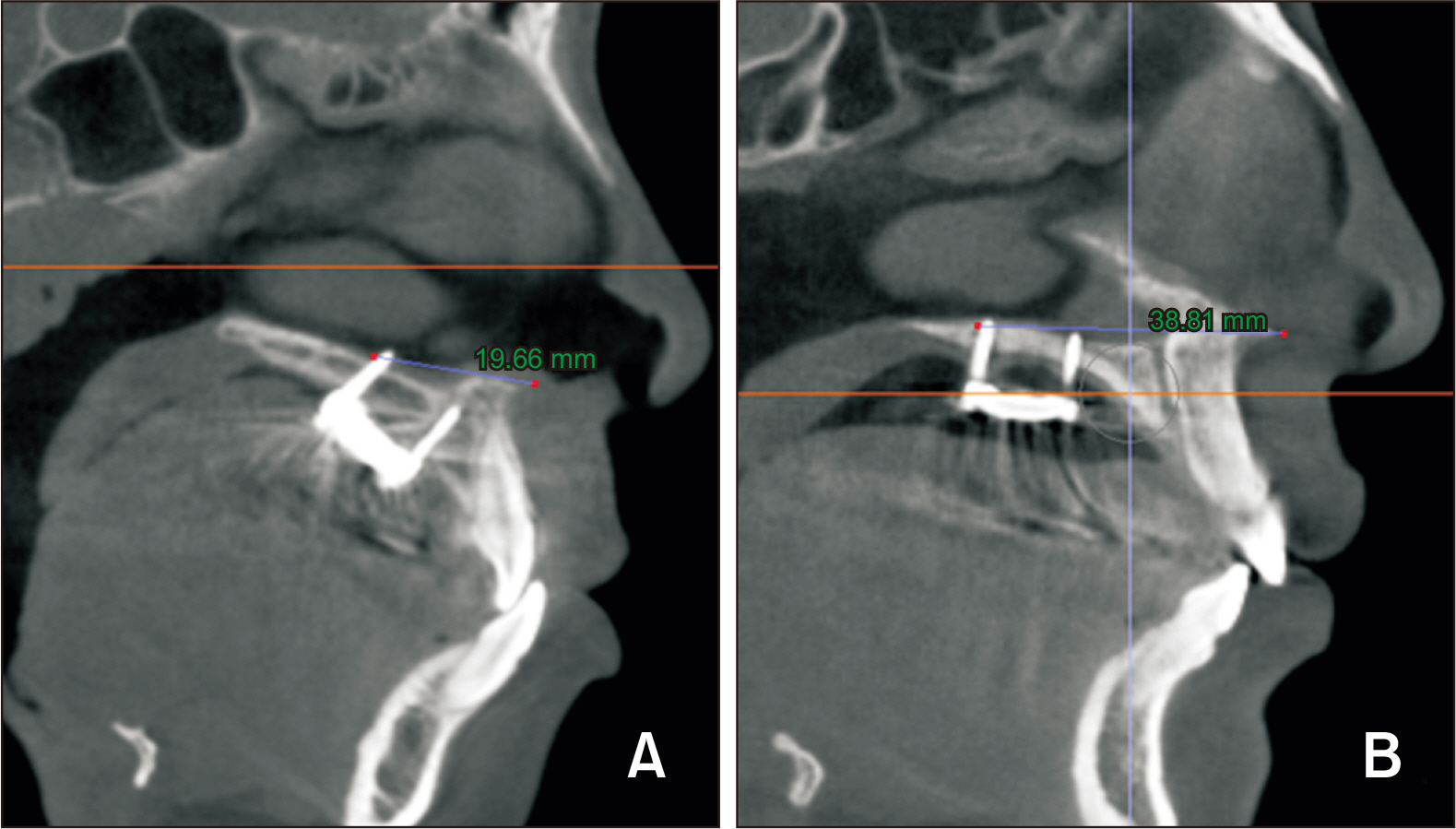
Pretreatment (T0) and post-MARPE (T1) cone-beam computed tomography (CBCT) images of 32 patients (14 males and 18 females; mean age, 19.37) were analyzed. We compared two different MARPE systems. One MARPE system included the maxillary first premolars, maxillary first molars, and four microimplants as anchors (U46 type, n = 16), while the other included only the maxillary first molars and microimplants as anchors (U6 type, n = 16).
Results
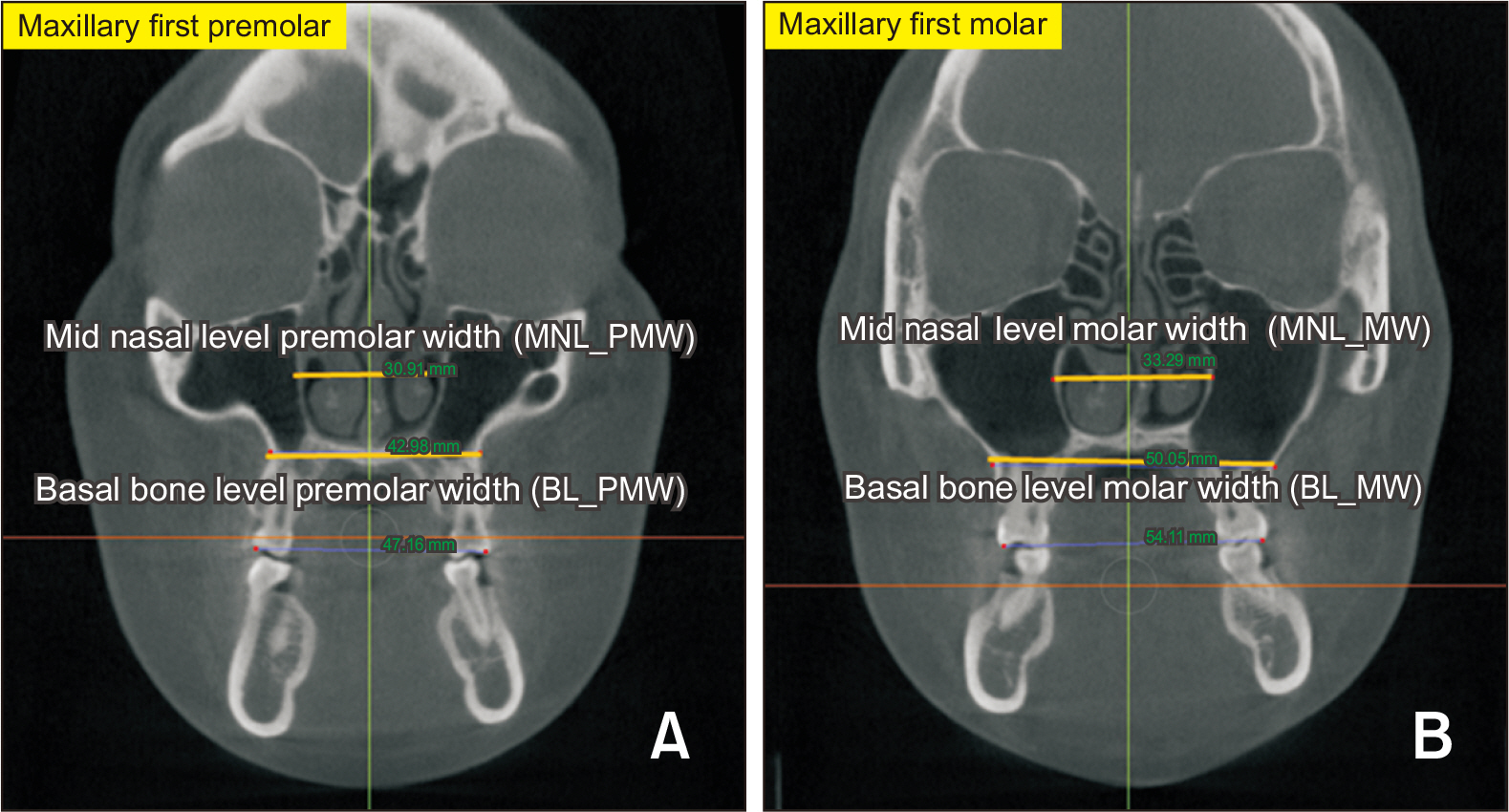
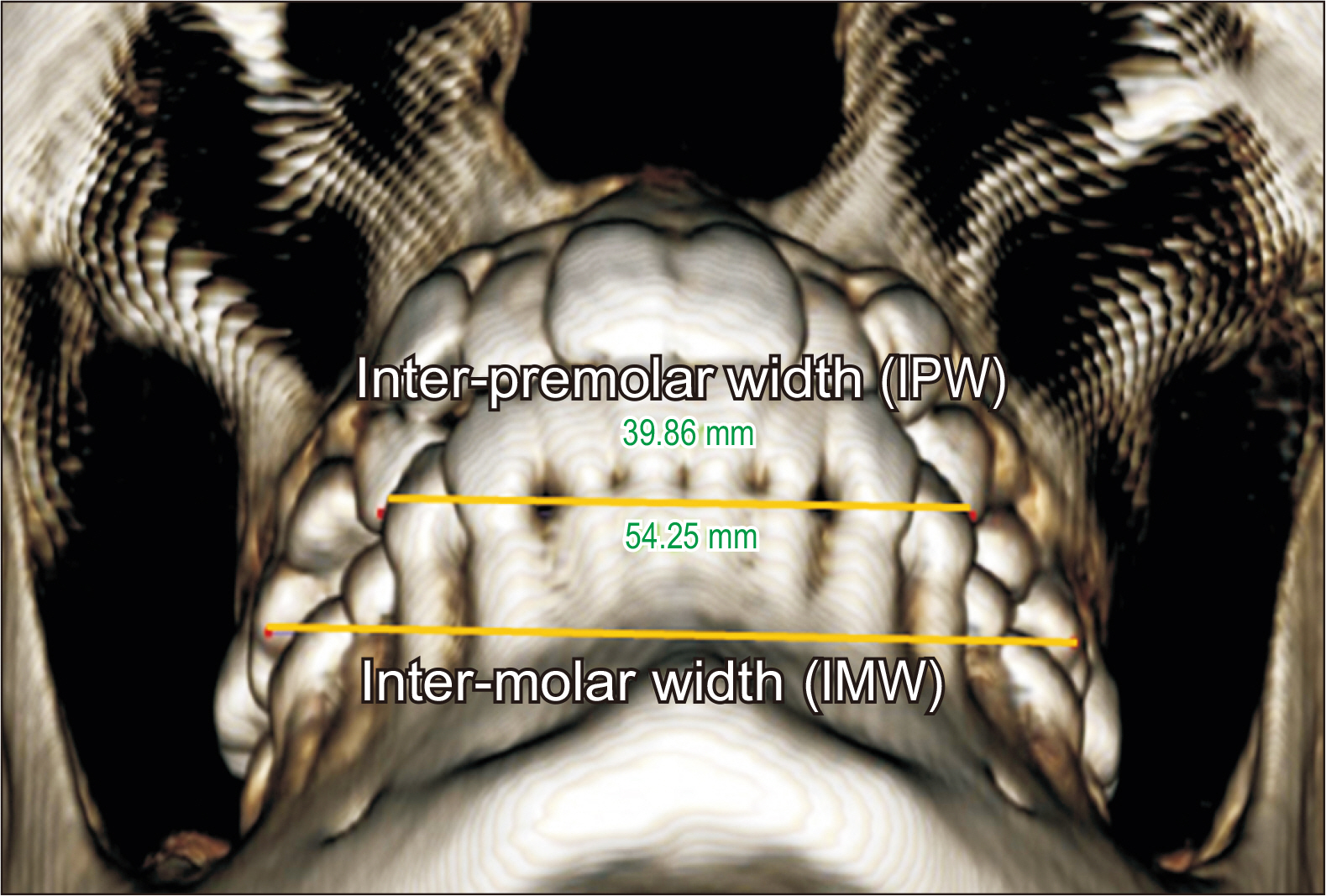
In the molar region of the U6 and U46 groups, the transverse expansion at the midnasal, basal, alveolar, and dental levels was 2.64, 3.52, 4.46, and 6.32 mm and 2.17, 2.56, 2.73, and 5.71 mm, respectively. A significant difference was observed in the posterior alveolar-level expansion (p = 0.036) and posterior basal-bone-level expansion (p = 0.043) between the groups, with greater posterior skeletal and alveolar expansion in the U6 group.
Conclusions
Compared with the U46 group, the U6 group showed greater posterior expansion at the alveolar and basal-bone levels, with an almost parallel split. Both groups showed a pyramidal expansion pattern in the coronal view.
Keyword
Figure
Reference
-
1. Lee SR, Lee JW, Chung DH, Lee SM. 2020; Short-term impact of microimplant-assisted rapid palatal expansion on the nasal soft tissues in adults: a three-dimensional stereophotogrammetry study. Korean J Orthod. 50:75–85. https://doi.org/10.4041/kjod.2020.50.2.75. DOI: 10.4041/kjod.2020.50.2.75. PMID: 32257933. PMCID: PMC7093666.
Article2. Proffit WR, White RP Jr. 1990; Who needs surgical-orthodontic treatment? Int J Adult Orthodon Orthognath Surg. 5:81–9. https://pubmed.ncbi.nlm.nih.gov/2074379/. PMID: 2074379.3. Mohan CN, Araujo EA, Oliver DR, Kim KB. 2016; Long-term stability of rapid palatal expansion in the mixed dentition vs the permanent dentition. Am J Orthod Dentofacial Orthop. 149:856–62. https://doi.org/10.1016/j.ajodo.2015.11.027. DOI: 10.1016/j.ajodo.2015.11.027. PMID: 27241996.
Article4. de Oliveira CB, Ayub P, Ledra IM, Murata WH, Suzuki SS, Ravelli DB, et al. 2021; Microimplant assisted rapid palatal expansion vs surgically assisted rapid palatal expansion for maxillary transverse discrepancy treatment. Am J Orthod Dentofacial Orthop. 159:733–42. https://doi.org/10.1016/j.ajodo.2020.03.024. DOI: 10.1016/j.ajodo.2020.03.024. PMID: 33931257.
Article5. Park JJ, Park YC, Lee KJ, Cha JY, Tahk JH, Choi YJ. 2017; Skeletal and dentoalveolar changes after miniscrew-assisted rapid palatal expansion in young adults: a cone-beam computed tomography study. Korean J Orthod. 47:77–86. https://doi.org/10.4041/kjod.2017.47.2.77. DOI: 10.4041/kjod.2017.47.2.77. PMID: 28337417. PMCID: PMC5359634.
Article6. Gurel HG, Memili B, Erkan M, Sukurica Y. 2010; Long-term effects of rapid maxillary expansion followed by fixed appliances. Angle Orthod. 80:5–9. https://doi.org/10.2319/011209-22.1. DOI: 10.2319/011209-22.1. PMID: 19852633. PMCID: PMC8978752.7. Cantarella D, Dominguez-Mompell R, Mallya SM, Moschik C, Pan HC, Miller J, et al. 2017; Changes in the midpalatal and pterygopalatine sutures induced by micro-implant-supported skeletal expander, analyzed with a novel 3D method based on CBCT imaging. Prog Orthod. 18:34. https://doi.org/10.1186/s40510-017-0188-7. DOI: 10.1186/s40510-017-0188-7. PMID: 29090368. PMCID: PMC5663987. PMID: c0a5028c7c5749d28981e5b6114032c6.8. Abate A, Cavagnetto D, Fama A, Matarese M, Lucarelli D, Assandri F. 2021; Short term effects of rapid maxillary expansion on breathing function assessed with spirometry: a case-control study. Saudi Dent J. 33:538–45. https://doi.org/10.1016/j.sdentj.2020.09.001. DOI: 10.1016/j.sdentj.2020.09.001. PMID: 34803298. PMCID: PMC8589571.9. Annarumma F, Posadino M, De Mari A, Drago S, Aghazada H, Gravina GM, et al. 2021; Skeletal and dental changes after maxillary expansion with a bone-borne appliance in young and late adolescent patients. Am J Orthod Dentofacial Orthop. 159:e363–75. https://doi.org/10.1016/j.ajodo.2020.11.031. DOI: 10.1016/j.ajodo.2020.11.031. PMID: 33573898.10. Harzer W, Reusser L, Hansen L, Richter R, Nagel T, Tausche E. 2010; Minimally invasive rapid palatal expansion with an implant-supported hyrax screw. Biomed Tech (Berl). 55:39–45. https://doi.org/10.1515/bmt.2010.002. DOI: 10.1515/bmt.2010.002. PMID: 20128744.11. Deeb W, Hansen L, Hotan T, Hietschold V, Harzer W, Tausche E. 2010; Changes in nasal volume after surgically assisted bone-borne rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 137:782–9. https://doi.org/10.1016/j.ajodo.2009.03.042. DOI: 10.1016/j.ajodo.2009.03.042. PMID: 20685533.12. Garib DG, Navarro R, Francischone CE, Oltramari PV. 2008; Rapid maxillary expansion using palatal implants. J Clin Orthod. 42:665–71. https://pubmed.ncbi.nlm.nih.gov/19075382/. PMID: 19075382.13. MacGinnis M, Chu H, Youssef G, Wu KW, Machado AW, Moon W. 2014; The effects of micro-implant assisted rapid palatal expansion (MARPE) on the nasomaxillary complex--a finite element method (FEM) analysis. Prog Orthod. 15:52. https://doi.org/10.1186/s40510-014-0052-y. DOI: 10.1186/s40510-014-0052-y. PMID: 25242527. PMCID: PMC4148550.14. De Cock J, Mermuys K, Goubau J, Van Petegem S, Houthoofd B, Casselman JW. 2012; Cone-beam computed tomography: a new low dose, high resolution imaging technique of the wrist, presentation of three cases with technique. Skeletal Radiol. 41:93–6. https://doi.org/10.1007/s00256-011-1198-z. DOI: 10.1007/s00256-011-1198-z. PMID: 21603872.15. Mah JK, Danforth RA, Bumann A, Hatcher D. 2003; Radiation absorbed in maxillofacial imaging with a new dental computed tomography device. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 96:508–13. https://doi.org/10.1016/s1079-2104(03)00350-0. DOI: 10.1016/S1079-2104(03)00350-0. PMID: 14561979.16. Abate A, Gaffuri F, Lanteri V, Fama A, Ugolini A, Mannina L, et al. 2022; A CBCT based analysis of the correlation between volumetric morphology of the frontal sinuses and the facial growth pattern in caucasian subjects. A cross-sectional study. Head Face Med. 18:4. https://doi.org/10.1186/s13005-022-00308-3. DOI: 10.1186/s13005-022-00308-3. PMID: 35109901. PMCID: PMC8809041. PMID: 5646d82bd58547428037b43553fdb251.17. Farronato M, Maspero C, Abate A, Grippaudo C, Connelly ST, Tartaglia GM. 2020; 3D cephalometry on reduced FOV CBCT: skeletal class assessment through AF-BF on Frankfurt plane-validity and reliability through comparison with 2D measurements. Eur Radiol. 30:6295–302. https://doi.org/10.1007/s00330-020-06905-7. DOI: 10.1007/s00330-020-06905-7. PMID: 32382843.18. Timock AM, Cook V, McDonald T, Leo MC, Crowe J, Benninger BL, et al. 2011; Accuracy and reliability of buccal bone height and thickness measurements from cone-beam computed tomography imaging. Am J Orthod Dentofacial Orthop. 140:734–44. https://doi.org/10.1016/j.ajodo.2011.06.021. DOI: 10.1016/j.ajodo.2011.06.021. PMID: 22051495.19. Lim HM, Park YC, Lee KJ, Kim KH, Choi YJ. 2017; Stability of dental, alveolar, and skeletal changes after miniscrew-assisted rapid palatal expansion. Korean J Orthod. 47:313–22. https://doi.org/10.4041/kjod.2017.47.5.313. DOI: 10.4041/kjod.2017.47.5.313. PMID: 28861393. PMCID: PMC5548712.20. Lione R, Ballanti F, Franchi L, Baccetti T, Cozza P. 2008; Treatment and posttreatment skeletal effects of rapid maxillary expansion studied with low-dose computed tomography in growing subjects. Am J Orthod Dentofacial Orthop. 134:389–92. https://doi.org/10.1016/j.ajodo.2008.05.011. DOI: 10.1016/j.ajodo.2008.05.011. PMID: 18774085.21. Lee DW, Park JH, Moon W, Seo HY, Chae JM. 2021; Effects of bicortical anchorage on pterygopalatine suture opening with microimplant-assisted maxillary skeletal expansion. Am J Orthod Dentofacial Orthop. 159:502–11. https://doi.org/10.1016/j.ajodo.2020.02.013. DOI: 10.1016/j.ajodo.2020.02.013. PMID: 33495061.22. Baltatu MS, Tugui CA, Perju MC, Benchea M, Spataru MC, Sandu AV, et al. 2019; Biocompatible titanium alloys used in medical applications. Rev Chim. 70:1302–6. https://doi.org/10.37358/RC.19.4.7114. DOI: 10.37358/RC.19.4.7114.23. Koo YJ, Choi SH, Keum BT, Yu HS, Hwang CJ, Melsen B, et al. 2017; Maxillomandibular arch width differences at estimated centers of resistance: comparison between normal occlusion and skeletal class III malocclusion. Korean J Orthod. 47:167–75. https://doi.org/10.4041/kjod.2017.47.3.167. DOI: 10.4041/kjod.2017.47.3.167. PMID: 28523243. PMCID: PMC5432438.24. Magnusson A, Bjerklin K, Kim H, Nilsson P, Marcusson A. 2012; Three-dimensional assessment of transverse skeletal changes after surgically assisted rapid maxillary expansion and orthodontic treatment: a prospective computerized tomography study. Am J Orthod Dentofacial Orthop. 142:825–33. https://doi.org/10.1016/j.ajodo.2012.08.015. DOI: 10.1016/j.ajodo.2012.08.015. PMID: 23195368.25. Lin L, Ahn HW, Kim SJ, Moon SC, Kim SH, Nelson G. 2015; Tooth-borne vs bone-borne rapid maxillary expanders in late adolescence. Angle Orthod. 85:253–62. https://doi.org/10.2319/030514-156.1. DOI: 10.2319/030514-156.1. PMID: 25490552. PMCID: PMC8631879.26. Gunyuz Toklu M, Germec-Cakan D, Tozlu M. 2015; Periodontal, dentoalveolar, and skeletal effects of tooth-borne and tooth-bone-borne expansion appliances. Am J Orthod Dentofacial Orthop. 148:97–109. https://doi.org/10.1016/j.ajodo.2015.02.022. DOI: 10.1016/j.ajodo.2015.02.022. PMID: 26124033.27. Lagravère MO, Carey J, Heo G, Toogood RW, Major PW. 2010; Transverse, vertical, and anteroposterior changes from bone-anchored maxillary expansion vs traditional rapid maxillary expansion: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 137:304.e1–12. discussion 304–5. https://doi.org/10.1016/j.ajodo.2009.09.016. DOI: 10.1016/j.ajodo.2009.09.016. PMID: 20197161.28. Altieri F, Cassetta M. 2022; Comparison of changes in skeletal, dentoalveolar, periodontal, and nasal structures after tooth-borne or bone-borne rapid maxillary expansion: a parallel cohort study. Am J Orthod Dentofacial Orthop. 161:e336–44. https://doi.org/10.1016/j.ajodo.2021.11.007. DOI: 10.1016/j.ajodo.2021.11.007. PMID: 34996663.29. Carlson C, Sung J, McComb RW, Machado AW, Moon W. 2016; Microimplant-assisted rapid palatal expansion appliance to orthopedically correct transverse maxillary deficiency in an adult. Am J Orthod Dentofacial Orthop. 149:716–28. https://doi.org/10.1016/j.ajodo.2015.04.043. DOI: 10.1016/j.ajodo.2015.04.043. PMID: 27131254.30. Lee RJ, Moon W, Hong C. 2017; Effects of monocortical and bicortical mini-implant anchorage on bone-borne palatal expansion using finite element analysis. Am J Orthod Dentofacial Orthop. 151:887–97. https://doi.org/10.1016/j.ajodo.2016.10.025. DOI: 10.1016/j.ajodo.2016.10.025. PMID: 28457266. PMCID: PMC5472094.31. Tausche E, Hansen L, Hietschold V, Lagravère MO, Harzer W. 2007; Three-dimensional evaluation of surgically assisted implant bone-borne rapid maxillary expansion: a pilot study. Am J Orthod Dentofacial Orthop. 131(4 Suppl):S92–9. https://doi.org/10.1016/j.ajodo.2006.07.021. DOI: 10.1016/j.ajodo.2006.07.021. PMID: 17448393.32. Pickard MB, Dechow P, Rossouw PE, Buschang PH. 2010; Effects of miniscrew orientation on implant stability and resistance to failure. Am J Orthod Dentofacial Orthop. 137:91–9. https://doi.org/10.1016/j.ajodo.2007.12.034. DOI: 10.1016/j.ajodo.2007.12.034. PMID: 20122436.33. Ghoneima A, Abdel-Fattah E, Hartsfield J, El-Bedwehi A, Kamel A, Kula K. 2011; Effects of rapid maxillary expansion on the cranial and circummaxillary sutures. Am J Orthod Dentofacial Orthop. 140:510–9. https://doi.org/10.1016/j.ajodo.2010.10.024. DOI: 10.1016/j.ajodo.2010.10.024. PMID: 21967938. PMCID: PMC5161454.34. Ramieri GA, Spada MC, Austa M, Bianchi SD, Berrone S. 2005; Transverse maxillary distraction with a bone-anchored appliance: dento-periodontal effects and clinical and radiological results. Int J Oral Maxillofac Surg. 34:357–63. https://doi.org/10.1016/j.ijom.2004.10.011. DOI: 10.1016/j.ijom.2004.10.011. PMID: 16053842.35. Asscherickx K, Govaerts E, Aerts J, Vande Vannet B. 2016; Maxillary changes with bone-borne surgically assisted rapid palatal expansion: a prospective study. Am J Orthod Dentofacial Orthop. 149:374–83. https://doi.org/10.1016/j.ajodo.2015.08.018. DOI: 10.1016/j.ajodo.2015.08.018. PMID: 26926025.36. Pinto PX, Mommaerts MY, Wreakes G, Jacobs WV. 2001; Immediate postexpansion changes following the use of the transpalatal distractor. J Oral Maxillofac Surg. 59:994–1000. discussion 1001https://doi.org/10.1053/joms.2001.25823. DOI: 10.1053/joms.2001.25823. PMID: 11526562.37. Kim HJ, Yun HS, Park HD, Kim DH, Park YC. 2006; Soft-tissue and cortical-bone thickness at orthodontic implant sites. Am J Orthod Dentofacial Orthop. 130:177–82. https://doi.org/10.1016/j.ajodo.2004.12.024. DOI: 10.1016/j.ajodo.2004.12.024. PMID: 16905061.38. Braun S, Bottrel JA, Lee KG, Lunazzi JJ, Legan HL. 2000; The biomechanics of rapid maxillary sutural expansion. Am J Orthod Dentofacial Orthop. 118:257–61. https://doi.org/10.1067/mod.2000.108254. DOI: 10.1067/mod.2000.108254. PMID: 10982925.39. Lione R, Franchi L, Cozza P. 2013; Does rapid maxillary expansion induce adverse effects in growing subjects? Angle Orthod. 83:172–82. https://doi.org/10.2319/041012-300.1. DOI: 10.2319/041012-300.1. PMID: 22827478. PMCID: PMC8805530.40. Garrett BJ, Caruso JM, Rungcharassaeng K, Farrage JR, Kim JS, Taylor GD. 2008; Skeletal effects to the maxilla after rapid maxillary expansion assessed with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 134:8–9. https://doi.org/10.1016/j.ajodo.2008.06.004. DOI: 10.1016/j.ajodo.2008.06.004. PMID: 18617096.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effectiveness of miniscrew assisted rapid palatal expansion using cone beam computed tomography: A systematic review and meta-analysis
- A posteroanterior cephalometric study on the change of maxilla by rapid palatal expansion
- Skeletal and dentoalveolar changes after miniscrew-assisted rapid palatal expansion in young adults: A cone-beam computed tomography study
- A study on the effect of rapid maxillary expansion and its relapse
- Pattern of microimplant displacement during maxillary skeletal expander treatment: A cone-beam computed tomography study