J Korean Med Sci.
2023 Aug;38(31):e239. 10.3346/jkms.2023.38.e239.
Temporal Trend of the Incidence and Characteristics of Renal Infarction: Korean Nationwide Population Study
- Affiliations
-
- 1Division of Cardiology, Soonchunhyang University Bucheon Hospital, Bucheon, Korea
- 2Department of Data Science, Hanmi Pharm. Co., Ltd., Seoul, Korea
- 3Division of Cardiology, Soonchunhyang University Seoul Hospital, Seoul, Korea
- KMID: 2544958
- DOI: http://doi.org/10.3346/jkms.2023.38.e239
Abstract
- Background
Large-scale studies about epidemiologic characteristics of renal infarction (RI) are few. In this study, we aimed to analyze the incidence and prevalence of RI with comorbidities in the South Korean population.
Methods
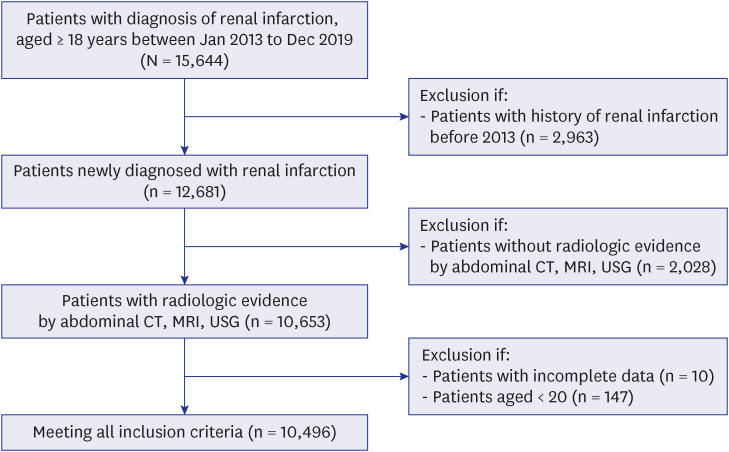
We investigated the medical history of the entire South Korean adult population between 2013 and 2019 using the National Health Insurance Service database (n = 51,849,591 in 2019). Diagnosis of RI comorbidities were confirmed with International Classification of Disease, Tenth Revision, Clinical Modification codes. Epidemiologic characteristics, distribution of comorbidities according to etiologic mechanisms, and trend of antithrombotic agents were estimated.
Results
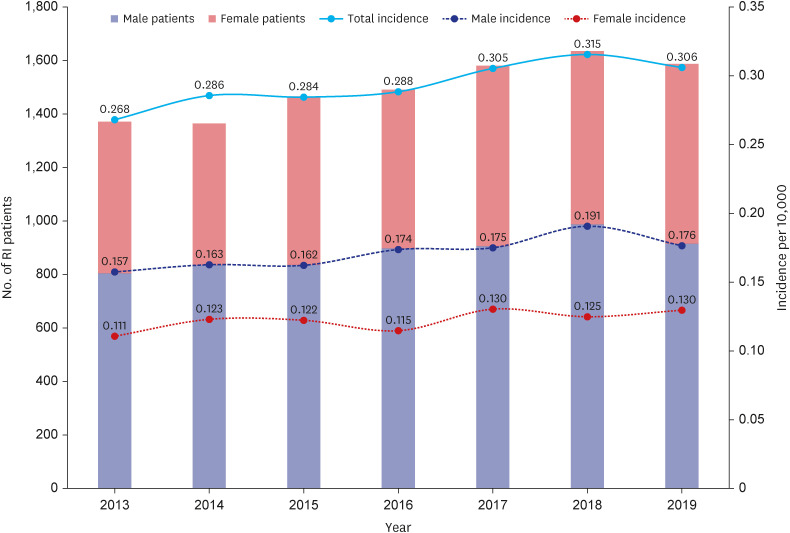
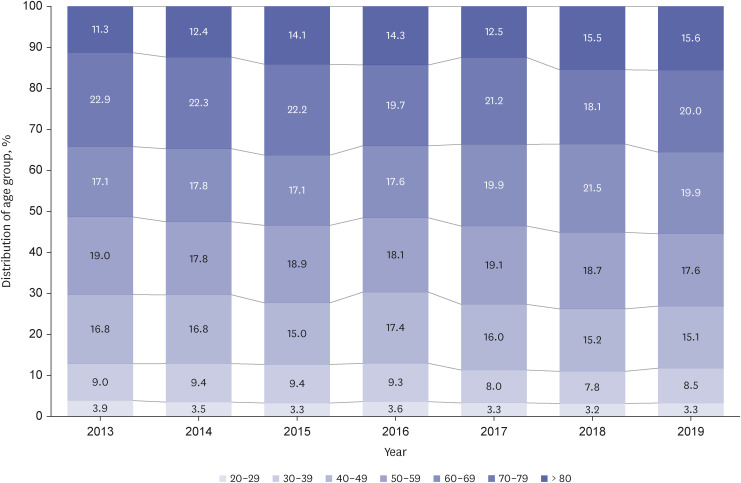
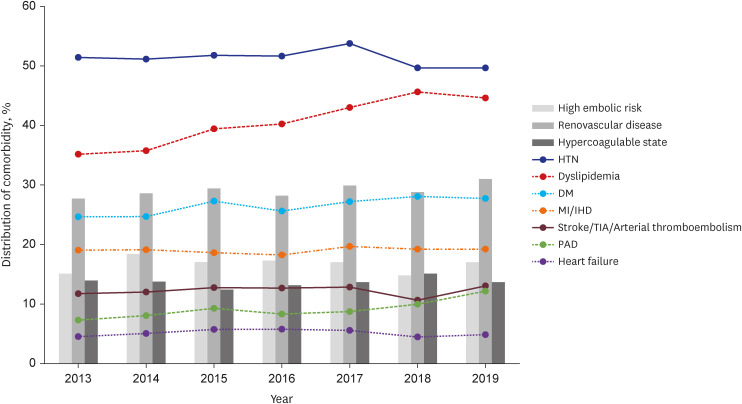
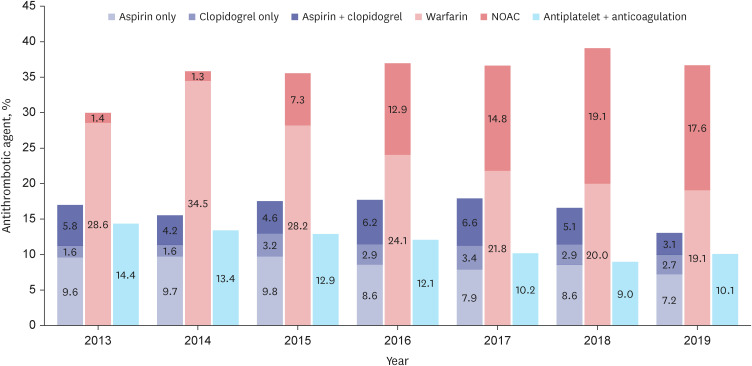
During the 7-years, 10,496 patients were newly diagnosed with RI. The incidence rate increased from 2.68 to 3.06 per 100,000 person-years during the study period. The incidence rate of RI increased with age peaking in the 70s with 1.41 times male predominance. The most common comorbidity was hypertension, followed by dyslipidemia and diabetes mellitus. Regarding etiologic risk factor distribution, high embolic risk group, renovascular disease group, and hypercoagulable state group accounted for 16.6%, 29.1%, and 13.7% on average, respectively. For the antithrombotic treatment of RI, the prescription of antiplatelet agent gradually decreased from 17.0% to 13.0% while that of anticoagulation agent was maintained around 35%. The proportion of non-vitamin K antagonist oral anticoagulants remarkably increased from only 1.4% to 17.6%.
Conclusion
Considering the progressively increasing incidence of RI and high prevalence of coexisting risk factors, constant efforts to raise awareness of the disease are necessary. The current epidemiologic investigation of RI would be the stepping-stone to establishing future studies about clinical outcomes and optimal treatment strategies.
Figure
Reference
-
1. Paris B, Bobrie G, Rossignol P, Le Coz S, Chedid A, Plouin PF. Blood pressure and renal outcomes in patients with kidney infarction and hypertension. J Hypertens. 2006; 24(8):1649–1654. PMID: 16877969.2. Bae EJ, Hwang K, Jang HN, Kim MJ, Jeon DH, Kim HJ, et al. A retrospective study of short- and long-term effects on renal function after acute renal infarction. Ren Fail. 2014; 36(9):1385–1389. PMID: 25112371.3. Eren N, Gungor O, Kocyigit I, Guzel FB, Erken E, Altunoren O, et al. Acute renal infarction in Turkey: a review of 121 cases. Int Urol Nephrol. 2018; 50(11):2067–2072. PMID: 30251011.4. Lessman RK, Johnson SF, Coburn JW, Kaufman JJ. Renal artery embolism: clinical features and long-term follow-up of 17 cases. Ann Intern Med. 1978; 89(4):477–482. PMID: 697226.5. Lee HH, Cho SM, Lee H, Baek J, Bae JH, Chung WJ, et al. Korea heart disease fact sheet 2020: analysis of nationwide data. Korean Circ J. 2021; 51(6):495–503. PMID: 34085422.6. Arafa A, Lee HH, Eshak ES, Shirai K, Liu K, Li J, et al. Modifiable risk factors for cardiovascular disease in Korea and Japan. Korean Circ J. 2021; 51(8):643–655. PMID: 34227266.7. Antopolsky M, Simanovsky N, Stalnikowicz R, Salameh S, Hiller N. Renal infarction in the ED: 10-year experience and review of the literature. Am J Emerg Med. 2012; 30(7):1055–1060. PMID: 21871764.8. Kagaya S, Yoshie O, Fukami H, Sato H, Saito A, Takeuchi Y, et al. Renal infarct volume and renal function decline in acute and chronic phases. Clin Exp Nephrol. 2017; 21(6):1030–1034. PMID: 28283850.9. Kim JS, Lee SY, Kim JH, Kwon EH, Song SH, Lee DW, et al. Acute renal infarction: clinical features in 23 cases. Korean J Med. 2006; 70(5):543–550.10. Ongun S, Bozkurt O, Demir O, Cimen S, Aslan G. Midterm renal functions following acute renal infarction. Kaohsiung J Med Sci. 2015; 31(10):529–533. PMID: 26520692.11. Moon I, Lee SY, Kim HK, Han KD, Kwak S, Kim M, et al. Trends of the prevalence and incidence of hypertrophic cardiomyopathy in Korea: a nationwide population-based cohort study. PLoS One. 2020; 15(1):e0227012. PMID: 31929538.12. Bourgault M, Grimbert P, Verret C, Pourrat J, Herody M, Halimi JM, et al. Acute renal infarction: a case series. Clin J Am Soc Nephrol. 2013; 8(3):392–398. PMID: 23204242.13. Faucon AL, Bobrie G, Jannot AS, Azarine A, Plouin PF, Azizi M, et al. Cause of renal infarction: a retrospective analysis of 186 consecutive cases. J Hypertens. 2018; 36(3):634–640. PMID: 29045340.14. Oh YK, Yang CW, Kim YL, Kang SW, Park CW, Kim YS, et al. Clinical characteristics and outcomes of renal infarction. Am J Kidney Dis. 2016; 67(2):243–250. PMID: 26545635.15. Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021; 52(7):e364–e467. PMID: 34024117.16. Mulder FI, Horváth-Puhó E, van Es N, Pedersen L, Büller HR, Bøtker HE, et al. Arterial thromboembolism in cancer patients: a Danish population-based cohort study. JACC CardioOncol. 2021; 3(2):205–218. PMID: 34396325.17. Navi BB, Singer S, Merkler AE, Cheng NT, Stone JB, Kamel H, et al. Recurrent thromboembolic events after ischemic stroke in patients with cancer. Neurology. 2014; 83(1):26–33. PMID: 24850486.18. Mejza F, Lamprecht B, Niżankowska-Mogilnicka E, Undas A. Arterial and venous thromboembolism in chronic obstructive pulmonary disease: from pathogenic mechanisms to prevention and treatment. Pneumonol Alergol Pol. 2015; 83(6):485–494. PMID: 26559802.19. Fimognari FL, Scarlata S, Conte ME, Incalzi RA. Mechanisms of atherothrombosis in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2008; 3(1):89–96. PMID: 18488431.20. Domanovits H, Paulis M, Nikfardjam M, Meron G, Kürkciyan I, Bankier AA, et al. Acute renal infarction. Clinical characteristics of 17 patients. Medicine (Baltimore). 1999; 78(6):386–394. PMID: 10575421.21. Huang CC, Lo HC, Huang HH, Kao WF, Yen DH, Wang LM, et al. ED presentations of acute renal infarction. Am J Emerg Med. 2007; 25(2):164–169. PMID: 17276805.22. Weber E, Grangeon F, Reynaud Q, Hot A, Sève P, Jardel S, et al. Acute renal and splenic infarctions: a review. QJM. 2020; 113(3):186–193. PMID: 31593227.23. Kanjwal K, Figueredo VM. Controversies in the management of the renal artery stenosis. Cardiol J. 2013; 20(1):11–16. PMID: 23558805.24. Khayat MI, Nee R, Little DJ, Olson SW. Idiopathic renal infarction and anticoagulation. TH Open. 2019; 3(4):e331–e334. PMID: 31602422.25. Silverberg D, Menes T, Rimon U, Salomon O, Halak M. Acute renal artery occlusion: presentation, treatment, and outcome. J Vasc Surg. 2016; 64(4):1026–1032. PMID: 27345378.26. Fu ZF, Zhang ZG, Liu XM. A rare case of acute renal infarction. Chin Med J (Engl). 2008; 121(2):185–187. PMID: 18272051.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The effect of age, gender, economic state, and urbanization on the temporal trend in sudden cardiac arrest: a nationwide population‑based cohort study
- Continuous Blood Pressure Monitorings during Cardiovascular Opertions in Takayasu`s Syndrome
- Absence of a Seasonal Variation of Hemorrhagic Fever with Renal Syndrome in Yeoncheon Compared to Nationwide Korea
- A study on the recent trend and risk factors of cerebrovascular disease
- Epidemiology and Management Trend of Renal Trauma: Results of a Nationwide Population-Based Study