J Korean Med Sci.
2023 Jul;38(29):e219. 10.3346/jkms.2023.38.e219.
Contrast-Enhanced Ultrasonography for the Evaluation of Crohn’s Disease in Pediatric Patients
- Affiliations
-
- 1Department of Radiology and Research Institute of Radiological Science, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 2Division of Gastroenterology, Hepatology and Nutrition, Department of Pediatrics, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2544942
- DOI: http://doi.org/10.3346/jkms.2023.38.e219
Abstract
- Background
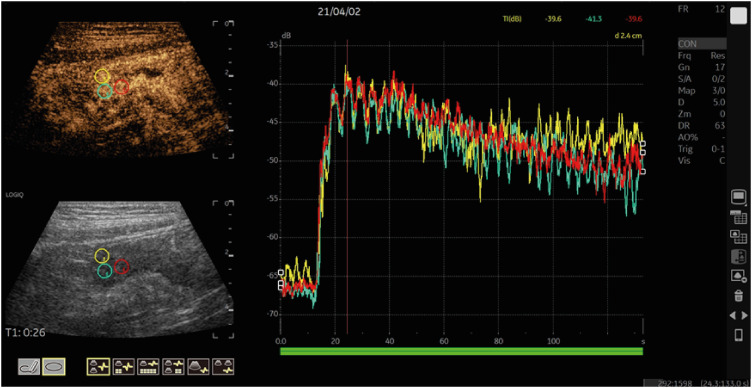
Contrast-enhanced ultrasonography (CEUS) of the bowel wall has been suggested as an alternative imaging modality for the follow-up of children with Crohn’s disease. To demonstrate the feasibility and clinical usefulness of CEUS in the estimation of Crohn’s disease activity in children with endoscopy as the reference standard. Method: In this prospective study, 30 pediatric patients with Crohn’s disease (24 males and 6 females; median age 14 years) underwent CEUS from December 2020 to August 2021. The simple endoscopic score for Crohn’s disease, pediatric Crohn’s disease activity index, serologic inflammatory markers, fecal calprotectin and CEUS perfusion parameters were assessed and compared between the inactive and active group based on endoscopic findings.
Results
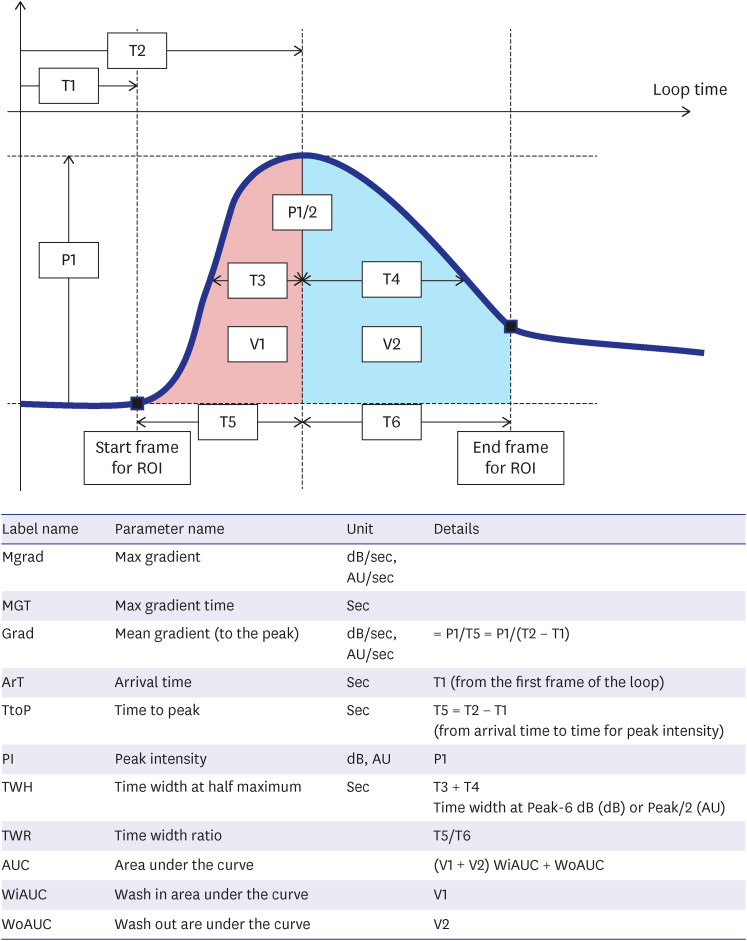
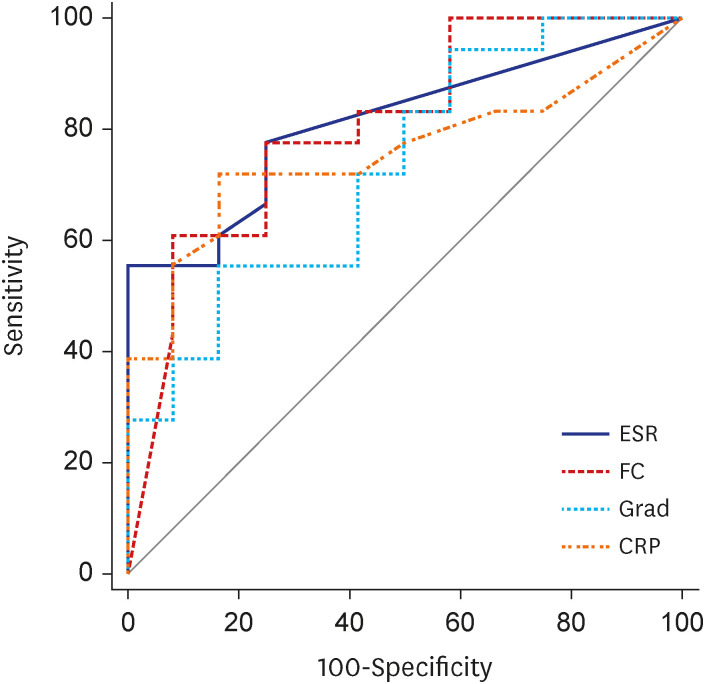
CEUS was performed successfully in all 30 patients. Two patients showed mild adverse side effects such as temporary dysosmia. The active Crohn’s disease group showed higher erythrocyte sedimentation rate (mm/hr) (13.0 vs. 2.0, P = 0.003), C-reactive protein (mg/dL) (4.7 vs. 0.55, P = 0.018) and fecal calprotectin (mcg/g) (1,503 vs. 237.5, P = 0.005). Among the quantitative parameters for CEUS, the mean gradient to the peak value was higher in the active group (1.18 vs. 0.93, P = 0.034). The sensitivity and specificity of the mean gradient to the peak value for predicting active Crohn’s disease was 55.6% and 83.3%, respectively, with a cut-off of 1.09 (P = 0.015).
Conclusion
CEUS can be a safe and specific diagnostic modality for Crohn’s disease activity in children. Among quantitative CEUS parameters, the mean gradient to the peak value could be used to differentiate active and inactive Crohn’s disease.
Figure
Reference
-
1. Park SH, Im JP, Park H, Jeong SK, Lee JH, Rhee KH, et al. Clinical features and long-term outcomes of paediatric-onset inflammatory bowel disease in a population-based cohort in the Songpa-Kangdong district of Seoul, Korea. J Crohns Colitis. 2022; 16(2):207–215. PMID: 34309652.2. Lee JW, Eun CS. Inflammatory bowel disease in Korea: epidemiology and pathophysiology. Korean J Intern Med. 2022; 37(5):885–894. PMID: 35902371.3. Choe JY, Choi S, Song KH, Jang HJ, Choi KH, Yi DY, et al. Incidence and prevalence trends of pediatric inflammatory bowel disease in the Daegu-Kyungpook Province from 2017 to 2020. Front Pediatr. 2022; 9:810173. PMID: 35059365.4. Park S, Kang B, Kim S, Choi S, Suh HR, Kim ES, et al. Comparison between pediatric Crohn’s disease and ulcerative colitis at diagnosis in Korea: results from a multicenter, registry-based, inception cohort study. Gut Liver. 2022; 16(6):921–929. PMID: 36059091.5. Choi SY, Choi S, Kang B, Choe BH, Lee YJ, Park JH, et al. Epidemiological trends of pediatric inflammatory bowel disease in Korea: a multicenter study of the last 3 years including the COVID-19 era. J Korean Med Sci. 2022; 37(37):e279. PMID: 36163477.6. Rosen MJ, Dhawan A, Saeed SA. Inflammatory bowel disease in children and adolescents. JAMA Pediatr. 2015; 169(11):1053–1060. PMID: 26414706.7. Levine A, Koletzko S, Turner D, Escher JC, Cucchiara S, de Ridder L, et al. ESPGHAN revised porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr. 2014; 58(6):795–806. PMID: 24231644.8. Medellin A, Merrill C, Wilson SR. Role of contrast-enhanced ultrasound in evaluation of the bowel. Abdom Radiol (NY). 2018; 43(4):918–933. PMID: 29260278.9. Zezos P, Zittan E, Islam S, Hudson J, Ben-Bassat O, Nazarian A, et al. Associations between quantitative evaluation of bowel wall microvascular flow by contrast-enhanced ultrasound and indices of disease activity in Crohn’s disease patients using both bolus and infusion techniques. J Clin Ultrasound. 2019; 47(8):453–460. PMID: 31343081.10. Kljucevsek D, Vidmar D, Urlep D, Dezman R. Dynamic contrast-enhanced ultrasound of the bowel wall with quantitative assessment of Crohn’s disease activity in childhood. Radiol Oncol. 2016; 50(4):347–354. PMID: 27904441.11. Martínez MJ, Ripollés T, Paredes JM, Moreno-Osset E, Pazos JM, Blanc E. Intravenous contrast-enhanced ultrasound for assessing and grading postoperative recurrence of Crohn’s disease. Dig Dis Sci. 2019; 64(6):1640–1650. PMID: 30604372.12. Quaia E, Cabibbo B, De Paoli L, Toscano W, Poillucci G, Cova MA. The value of time-intensity curves obtained after microbubble contrast agent injection to discriminate responders from non-responders to anti-inflammatory medication among patients with Crohn’s disease. Eur Radiol. 2013; 23(6):1650–1659. PMID: 23306710.13. Mudambi K, Sandberg J, Bass D, Rubesova E. Contrast enhanced ultrasound: comparing a novel modality to MRI to assess for bowel disease in pediatric Crohn’s patients. Transl Gastroenterol Hepatol. 2020; 5:13. PMID: 32258517.14. Benjamin JL, Dennis R, White S Jr, Munson D, Anupindi SA, Piskunowicz M, et al. Improved diagnostic sensitivity of bowel disease of prematurity on contrast-enhanced ultrasound. J Ultrasound Med. 2020; 39(5):1031–1036. PMID: 31705672.15. Thimm MA, Cuffari C, Garcia A, Sidhu S, Hwang M. Contrast-enhanced ultrasound and shear wave elastography evaluation of Crohn’s disease activity in three adolescent patients. Pediatr Gastroenterol Hepatol Nutr. 2019; 22(3):282–290. PMID: 31110961.16. Ponorac S, Gošnak RD, Urlep D, Ključevšek D. Contrast-enhanced ultrasonography in the evaluation of Crohn disease activity in children: comparison with histopathology. Pediatr Radiol. 2021; 51(3):410–418. PMID: 33411024.17. Moskovitz DN, Daperno M, Assche GA. Defining and validating cut-offs for the Simple Endocopic Score for Crohn’s disease. Gastroenterology. 2007; 132:S1097.18. Sidhu PS, Cantisani V, Deganello A, Dietrich CF, Duran C, Franke D, et al. Role of contrast-enhanced ultrasound (CEUS) in paediatric practice: an EFSUMB position statement. Ultraschall Med. 2017; 38(1):33–43. PMID: 27414980.19. Piskunowicz M, Kosiak W, Batko T, Piankowski A, Połczyńska K, Adamkiewicz-Drożyńska E. Safety of intravenous application of second-generation ultrasound contrast agent in children: prospective analysis. Ultrasound Med Biol. 2015; 41(4):1095–1099. PMID: 25701526.20. Migaleddu V, Scanu AM, Quaia E, Rocca PC, Dore MP, Scanu D, et al. Contrast-enhanced ultrasonographic evaluation of inflammatory activity in Crohn’s disease. Gastroenterology. 2009; 137(1):43–52. PMID: 19422826.21. Girlich C, Jung EM, Huber E, Ott C, Iesalnieks I, Schreyer A, et al. Comparison between preoperative quantitative assessment of bowel wall vascularization by contrast-enhanced ultrasound and operative macroscopic findings and results of histopathological scoring in Crohn’s disease. Ultraschall Med. 2011; 32(2):154–159. PMID: 20449794.22. Quaia E, De Paoli L, Stocca T, Cabibbo B, Casagrande F, Cova MA. The value of small bowel wall contrast enhancement after sulfur hexafluoride-filled microbubble injection to differentiate inflammatory from fibrotic strictures in patients with Crohn’s disease. Ultrasound Med Biol. 2012; 38(8):1324–1332. PMID: 22698508.23. Paredes JM, Ripollés T, Cortés X, Moreno N, Martínez MJ, Bustamante-Balén M, et al. Contrast-enhanced ultrasonography: usefulness in the assessment of postoperative recurrence of Crohn’s disease. J Crohn’s Colitis. 2013; 7(3):192–201. PMID: 22542055.24. Schreyer AG, Finkenzeller T, Gössmann H, Daneschnejad M, Müller-Wille R, Schacherer D, et al. Microcirculation and perfusion with contrast enhanced ultrasound (CEUS) in Crohn’s disease: first results with linear contrast harmonic imaging (CHI). Clin Hemorheol Microcirc. 2008; 40(2):143–155. PMID: 19029639.25. Liu C, Xu XR, Xu HX, Liu ZJ, Zhang YF, Sun LP, et al. Conventional ultrasound and contrast-enhanced ultrasound in evaluating the severity of Crohn’s disease. Int J Clin Exp Med. 2015; 8(1):123–134. PMID: 25784981.26. Romanini L, Passamonti M, Navarria M, Lanzarotto F, Villanacci V, Grazioli L, et al. Quantitative analysis of contrast-enhanced ultrasonography of the bowel wall can predict disease activity in inflammatory bowel disease. Eur J Radiol. 2014; 83(8):1317–1323. PMID: 24908589.27. De Franco A, Di Veronica A, Armuzzi A, Roberto I, Marzo M, De Pascalis B, et al. Ileal Crohn disease: mural microvascularity quantified with contrast-enhanced US correlates with disease activity. Radiology. 2012; 262(2):680–688. PMID: 22157203.28. Wong DD, Forbes GM, Zelesco M, Mason R, Pawlik J, Mendelson RM. Crohn’s disease activity: quantitative contrast-enhanced ultrasound assessment. Abdom Imaging. 2012; 37(3):369–376. PMID: 21830051.29. Serafin Z, Białecki M, Białecka A, Sconfienza LM, Kłopocka M. Contrast-enhanced ultrasound for detection of Crohn’s disease activity: systematic review and meta-analysis. J Crohn’s Colitis. 2016; 10(3):354–362. PMID: 26507861.30. Ripollés T, Rausell N, Paredes JM, Grau E, Martínez MJ, Vizuete J. Effectiveness of contrast-enhanced ultrasound for characterisation of intestinal inflammation in Crohn’s disease: a comparison with surgical histopathology analysis. J Crohn’s Colitis. 2013; 7(2):120–128. PMID: 22483566.31. Turner D, Ricciuto A, Lewis A, D’Amico F, Dhaliwal J, Griffiths AM, et al. STRIDE-II: an update on the selecting therapeutic targets in inflammatory bowel disease (STRIDE) initiative of the international organization for the study of IBD (IOIBD): determining therapeutic goals for treat-to-target strategies in IBD. Gastroenterology. 2021; 160(5):1570–1583. PMID: 33359090.32. Lee S, Choi YH, Cho YJ, Cheon JE, Moon JS, Kang GH, et al. Quantitative evaluation of Crohn’s disease using dynamic contrast-enhanced MRI in children and young adults. Eur Radiol. 2020; 30(6):3168–3177. PMID: 32078012.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Contrast-Enhanced Ultrasound and Shear Wave Elastography Evaluation of Crohn's Disease Activity in Three Adolescent Patients
- Contrast-enhanced ultrasonography for the evaluation of malignant focal liver lesions
- Contrast-enhanced ultrasound of hepatocellular carcinoma: where do we stand?
- Ultrasonography of pediatric urogenital emergencies: review of classic and new techniques
- General principles and overview of vascular contrast-enhanced ultrasonography