J Rhinol.
2023 Jul;30(2):98-104. 10.18787/jr.2023.00016.
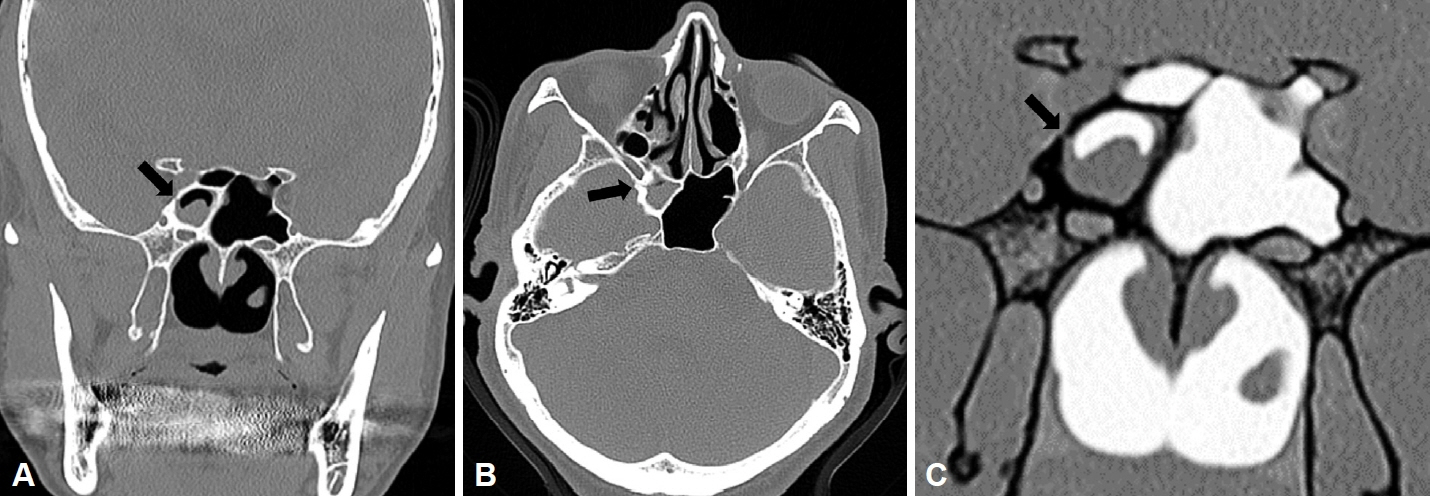
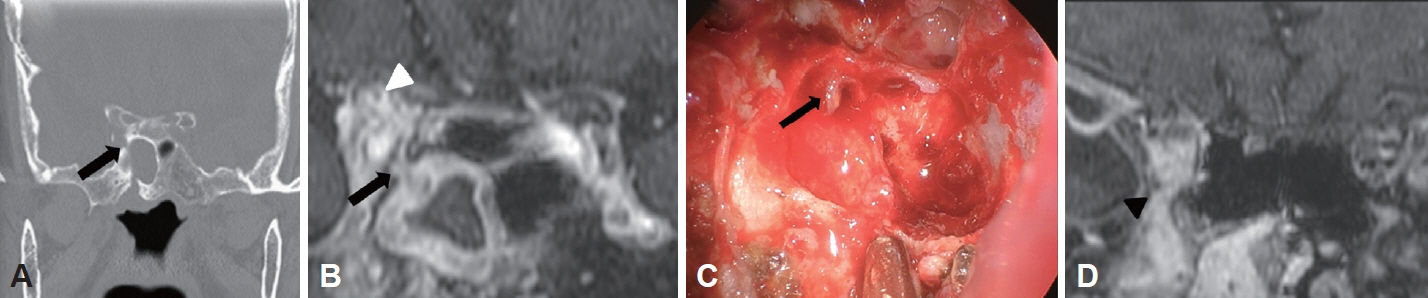
Prevalence and Clinical Implications of Lateral Wall Dehiscence in the Sphenoid Sinus: Sternberg’s Canal
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Republic of Korea
- 2Department of Radiology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Republic of Korea
- KMID: 2544619
- DOI: http://doi.org/10.18787/jr.2023.00016
Abstract
- Background and Objectives
Sternberg’s canal is known to result from incomplete fusion of bony compartments constituting the sphenoid bone during the developmental process. This study aimed to evaluate the prevalence and clinical implications of Sternberg’s canal.
Methods
A retrospective review of patients over the age of 18 years who had undergone endoscopic sinus surgery from 2014 to 2019 at a single institution was performed. Patients (n=98) were categorized into those with sphenoid fungal ball (SFB) (n=39), those with primary chronic rhinosinusitis (CRS) (n=39), and controls (n=20) and were evaluated radiologically. A small pit in the lateral wall, located medial to the maxillary division of the trigeminal nerve (V2), in front of the opticocarotid recess was regarded as Sternberg’s canal. Children under the age of 12 years (n=39) without any sinus disease were also evaluated to determine the prevalence of Sternberg’s canal in the pediatric population.
Results
Patients with SFB showed the highest prevalence of Sternberg’s canal (56.4%), followed by those with CRS (20.5%) and controls (10.0%) (p<0.001). Logistic regression revealed that Sternberg’s canal was associated with osteitis of the sphenoid wall, and not with age, sex, or sphenoid sinus pathology. Children under the age of 12 years showed a significantly higher prevalence of the defect than adult controls (46.2%, p<0.001).
Conclusion
Sternberg’s canal was frequently identified in children under the age of 12 years. Sphenoid sinus pathology was often accompanied by osteitis. However, the presence of the canal alone did not predict skull base involvement in patients with SFB. A comprehensive evaluation should hence be performed if skull base involvement is suspected in such patients. Additionally, other clinical implications of Sternberg’s canal should be further evaluated.
Figure
Reference
-
References
1. Simmonds JC, Scott AR. Spontaneous CSF rhinorrhea from the trigeminal canal in an adolescent. Int J Pediatr Otorhinolaryngol. 2017; 98:162–5.2. Illing E, Schlosser RJ, Palmer JN, Curé J, Fox N, Woodworth BA. Spontaneous sphenoid lateral recess cerebrospinal fluid leaks arise from intracranial hypertension, not Sternberg’s canal. Int Forum Allergy Rhinol. 2014; 4(3):246–50.3. Settecase F, Harnsberger HR, Michel MA, Chapman P, Glastonbury CM. Spontaneous lateral sphenoid cephaloceles: anatomic factors contributing to pathogenesis and proposed classification. AJNR Am J Neuroradiol. 2014; 35(4):784–9.4. Thakur JD, Manzi B, Savardekar AR, Singh MP, Menger R, Nanda A. Commentary: Maximilian Sternberg (1863-1934): the man behind Sternberg’s canal and his contribution to the modern-day skull base anatomy and neuroscience—historical vignette. Neurosurgery. 2018; 83(3):E120–4.5. Barañano CF, Curé J, Palmer JN, Woodworth BA. Sternberg’s canal: fact or fiction? Am J Rhinol Allergy. 2009; 23(2):167–71.6. Jung JH, Cho GS, Chung YS, Lee BJ. Clinical characteristics and outcome in patients with isolated sphenoid sinus aspergilloma. Auris Nasus Larynx. 2013; 40(2):189–93.7. Meier JC, Scangas GA, Remenschneider AK, Sadow P, Chambers K, Dedmon M, et al. Skull base erosion and associated complications in sphenoid sinus fungal balls. Allergy Rhinol (Providence). 2016; 7(4):227–32.8. Fokkens W, Desrosiers M, Harvey R, Hopkins C, Mullol J, Philpott C, et al. EPOS2020: development strategy and goals for the latest European position paper on rhinosinusitis. Rhinology. 2019; 57(3):162–8.9. Cha H, Song Y, Bae YJ, Won TB, Kim JW, Cho SW, et al. Clinical characteristics other than intralesional hyperdensity may increase the preoperative diagnostic accuracy of maxillary sinus fungal ball. Clin Exp Otorhinolaryngol. 2020; 13(2):157–63.10. Kim YS, Kim HJ, Kim CH, Kim J. CT and MR imaging findings of sinonasal schwannoma: a review of 12 cases. AJNR Am J Neuroradiol. 2013; 34(3):628–33.11. Bhandarkar ND, Mace JC, Smith TL. The impact of osteitis on disease severity measures and quality of life outcomes in chronic rhinosinusitis. Int Forum Allergy Rhinol. 2011; 1(5):372–8.12. Park JB, Cho YS, Choi HJ. Diagnostic accuracy of the inverted grayscale rib series for detection of rib fracture in minor chest trauma. Am J Emerg Med. 2015; 33(4):548–52.13. Hopkins C, Browne JP, Slack R, Lund V, Brown P. The Lund-Mackay staging system for chronic rhinosinusitis: how is it used and what does it predict? Otolaryngol Head Neck Surg. 2007; 137(4):555–61.14. Sethi N. The significance of osteitis in rhinosinusitis. Eur Arch Otorhinolaryngol. 2015; 272(4):821–6.15. Seo MY, Seok H, Lee SH, Choi JE, Hong SD, Chung SK, et al. Microinvasive fungal rhinosinusitis: proposal of a new subtype in the classification. J Clin Med. 2020; 9(2):600.16. Aribandi M, McCoy VA, Bazan C 3rd. Imaging features of invasive and noninvasive fungal sinusitis: a review. Radiographics. 2007; 27(5):1283–96.17. Coop CA, England RW. Allergic fungal sinusitis presenting with proptosis and diplopia: a review of ophthalmologic complications and treatment. Allergy Asthma Proc. 2006; 27(1):72–6.18. Deutsch PG, Whittaker J, Prasad S. Invasive and non-invasive fungal rhinosinusitis—a review and update of the evidence. Medicina (Kaunas). 2019; 55(7):319.19. Schick B, Brors D, Prescher A. Sternberg’s canal--cause of congenital sphenoidal meningocele. Eur Arch Otorhinolaryngol. 2000; 257(8):430–2.20. Giacchi RJ, Lebowitz RA, Yee HT, Light JP, Jacobs JB. Histopathologic evaluation of the ethmoid bone in chronic sinusitis. Am J Rhinol. 2001; 15(3):193–7.21. Szolar D, Preidler K, Ranner G, Braun H, Kugler C, Wolf G, et al. The sphenoid sinus during childhood: establishment of normal developmental standards by MRI. Surg Radiol Anat. 1994; 16(2):193–8.22. Shetty PG, Shroff MM, Fatterpekar GM, Sahani DV, Kirtane MV. A retrospective analysis of spontaneous sphenoid sinus fistula: MR and CT findings. AJNR Am J Neuroradiol. 2000; 21(2):337–42.23. Choi YR, Kim JH, Min HS, Won JK, Kim HJ, Yoo RE, et al. Acute invasive fungal rhinosinusitis: MR imaging features and their impact on prognosis. Neuroradiology. 2018; 60(7):715–23.24. Jun YJ, Shin JM, Lee JY, Baek BJ. Bony changes in a unilateral maxillary sinus fungal ball. J Craniofac Surg. 2018; 29(1):e44. –7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pneumatization of the sphenoid sinus and its surrounding neurovascular structures
- Lateral Sinus Thrombophlebitis Caused by Isolated Sphenoid Sinusitis
- Endoscope-Assisted Trans-Sphenoidal Approach for Treatment of Sternberg's Canal
- Anatomical Relationship between the Optic Nerve and Posterior Paranasal Sinuses on Ostiomeatal Unit CT
- Isolated Inverted Papilloma of the Sphenoid Sinus Presenting as Ptosis