Ann Surg Treat Res.
2023 Jul;105(1):1-9. 10.4174/astr.2023.105.1.1.
Survival analysis of breast cancer patients after diagnosis of second primary malignancies, focusing on the second primary hematologic malignancy
- Affiliations
-
- 1Department of Surgery, Korea Cancer Center Hospital, Korea Institute of Radiological and Medical Sciences, Seoul, Korea
- 2Division of Fusion Radiology Research, Korea Institute of Radiological & Medical Sciences, Seoul, Korea
- 3Department of Surgery, Konkuk University Medical Center, Seoul, Korea
- 4Department of Internal Medicine, Korea Cancer Center Hospital, Korea Institute of Radiological and Medical Sciences, Seoul, Korea
- KMID: 2544597
- DOI: http://doi.org/10.4174/astr.2023.105.1.1
Abstract
- Purpose
Although the overall survival (OS) of breast cancer patients is increasing with improved detection and therapies, so is the risk of breast cancer patients developing subsequent malignancies. We investigated the OS of breast cancer survivors according to sites of second primary malignancies (SPM). The OS of the second primary hematologic malignancy (SPHM) was then compared with that of metastatic breast cancer (MBC).
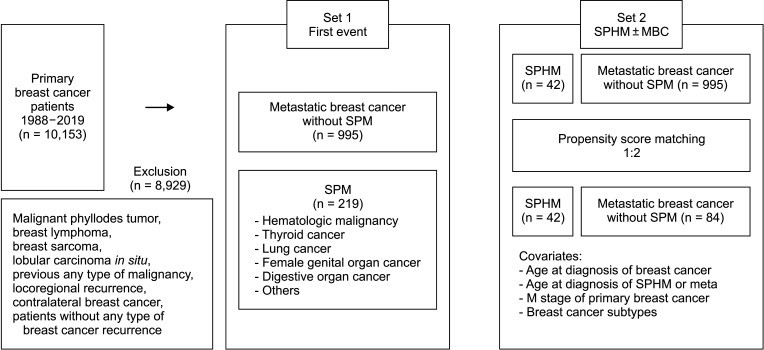
Methods
We retrospectively analyzed patients diagnosed with primary breast cancer between 1998 and 2019. Only those with SPM were eligible for analysis. First, the OS of patients with SPM diagnosed as the first event after the diagnosis of breast cancer was analyzed. Next, the OS of patients with SPHM, with or without breast cancer relapse, was compared with that of patients with MBC, matched using the propensity score.
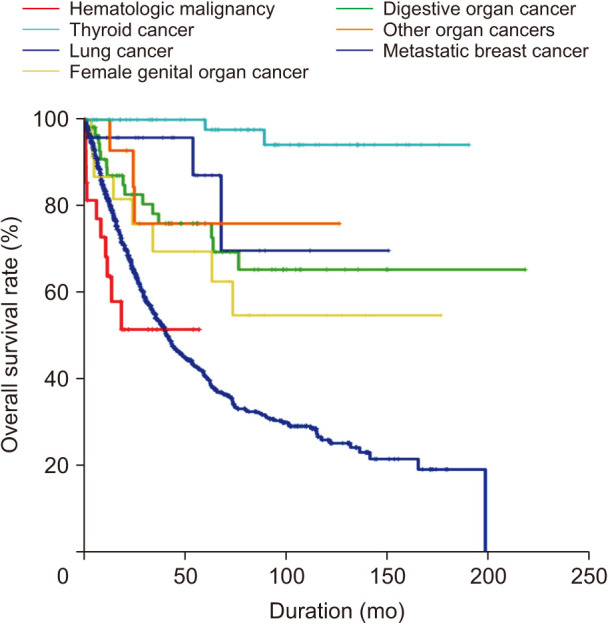
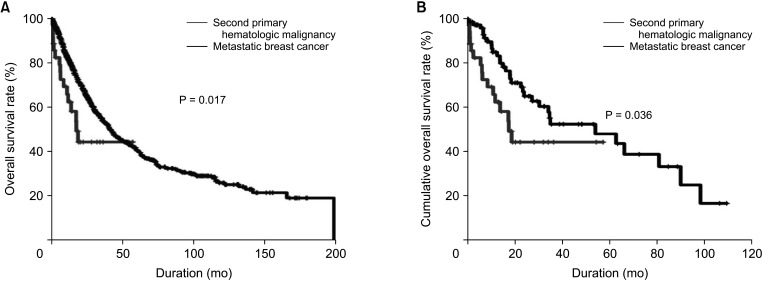
Results
Patients diagnosed with SPM without breast cancer relapse as the first event had a significantly better OS than did patients with MBC, but the OS of those with SPHM as the first event did not differ significantly from that of patients with MBC (hazard ratio [HR], 1.558; 95% confidence interval [CI], 0.856–2.839; P = 0.147). The OS of patients with SPHM with or without breast cancer relapse was worse than that of the MBC group after propensity score matching (HR, 1.954; 95% CI, 1.045–3.654; P = 0.036).
Conclusion
Prognosis of SPM diagnosed as the first event was statistically better than that of MBC, except in case of SPHM. Patients with SPHM, with or without MBC, showed poor OS before and after propensity score matching.
Figure
Reference
-
1. Kang SY, Lee SB, Kim YS, Kim Z, Kim HY, Kim HJ, et al. Breast cancer statistics in Korea, 2018. J Breast Cancer. 2021; 24:123–137. PMID: 33913273.2. Long Q, Wang Y, Che G. Primary lung cancer after treatment for breast cancer. Int J Womens Health. 2021; 13:1217–1225. PMID: 34908880.3. Kaplan HG, Malmgren JA, Atwood MK. Increased incidence of myelodysplastic syndrome and acute myeloid leukemia following breast cancer treatment with radiation alone or combined with chemotherapy: a registry cohort analysis 1990-2005. BMC Cancer. 2011; 11:260. PMID: 21693006.4. Jung HK, Park S, Kim NW, Lee JE, Kim Z, Han SW, et al. Development of second primary cancer in Korean breast cancer survivors. Ann Surg Treat Res. 2017; 93:287–292. PMID: 29250506.5. Emons G, Mustea A, Tempfer C. Tamoxifen and endometrial cancer: a Janus-headed drug. Cancers (Basel). 2020; 12:2535. PMID: 32906618.6. Ministry of Health and Welfare. Cancer Registration Statistics: number of cancer cases and incidence rates by 24 cancer types/sex/age (in 5-year intervals) [Internet]. Ministry of Health and Welfare;2023. cited 2023 Jun 26. Available from: https://kosis.kr/statHtml/statHtml.do?orgId=117&tblId=DT_117N_A00023&conn_path=I2.7. Paik S, Tang G, Shak S, Kim C, Baker J, Kim W, et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006; 24:3726–3734. PMID: 16720680.8. Kalinsky K, Barlow WE, Gralow JR, Meric-Bernstam F, Albain KS, Hayes DF, et al. 21-gene assay to inform chemotherapy benefit in node-positive breast cancer. N Engl J Med. 2021; 385:2336–2347. PMID: 34914339.9. Jabagi MJ, Vey N, Goncalves A, Le Tri T, Zureik M, Dray-Spira R. Evaluation of the incidence of hematologic malignant neoplasms among breast cancer survivors in France. JAMA Netw Open. 2019; 2:e187147. PMID: 30657534.10. Morton LM, Dores GM, Schonfeld SJ, Linet MS, Sigel BS, Lam CJ, et al. Association of chemotherapy for solid tumors with development of therapy-related myelodysplastic syndrome or acute myeloid leukemia in the modern era. JAMA Oncol. 2019; 5:318–325. PMID: 30570657.11. Colozza M, de Azambuja E, Personeni N, Lebrun F, Piccart MJ, Cardoso F. Achievements in systemic therapies in the pregenomic era in metastatic breast cancer. Oncologist. 2007; 12:253–270. PMID: 17405890.12. Kaplan HG, Calip GS, Malmgren JA. Maximizing breast cancer therapy with awareness of potential treatment-related blood disorders. Oncologist. 2020; 25:391–397. PMID: 32073195.13. Piccart M, van't Veer LJ, Poncet C, Lopes Cardozo JM, Delaloge S, Pierga JY, et al. 70-gene signature as an aid for treatment decisions in early breast cancer: updated results of the phase 3 randomised MINDACT trial with an exploratory analysis by age. Lancet Oncol. 2021; 22:476–488. PMID: 33721561.14. Villarreal-Garza C, Ferrigno AS, De la Garza-Ramos C, Barragan-Carrillo R, Lambertini M, Azim HA Jr. Clinical utility of genomic signatures in young breast cancer patients: a systematic review. NPJ Breast Cancer. 2020; 6:46. PMID: 33062888.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unexpected Second Primary Malignancies Detected by F-18 FDG PET/CT During Follow-up for Primary Malignancy: Two Case Reports
- The Incidence of Occult Malignancy in Contralateral Risk Reducing Mastectomy Among Affected Breast Cancer Gene Mutation Carriers in South Korea
- Second Primary Malignancies in Patients with Head and Neck Cancer
- Metachronous Four Primary Malignancies in Gastro-intestinal Tract
- A case of metachronous multiple primary malignant neoplasm of the gastric cancer and ovarian cancer and breast cancer