J Korean Med Sci.
2023 Jul;38(26):e199. 10.3346/jkms.2023.38.e199.
Assessment of the Suitability of the Fleischner Society Imaging Guidelines in Evaluating Chest Radiographs of COVID-19 Patients
- Affiliations
-
- 1Department of Radiology, Dongsan Hospital, Keimyung University College of Medicine, Daegu, Korea
- 2Department of Internal Medicine, Dongsan Hospital, Keimyung University College of Medicine, Daegu, Korea
- KMID: 2544014
- DOI: http://doi.org/10.3346/jkms.2023.38.e199
Abstract
- Background
The Fleischner Society established consensus guidelines for imaging in patients with coronavirus disease 2019 (COVID-19). We investigated the prevalence of pneumonia and the adverse outcomes by dividing groups according to the symptoms and risk factors of patients and assessed the suitability of the Fleischner society imaging guidelines in evaluating chest radiographs of COVID-19 patients.
Methods
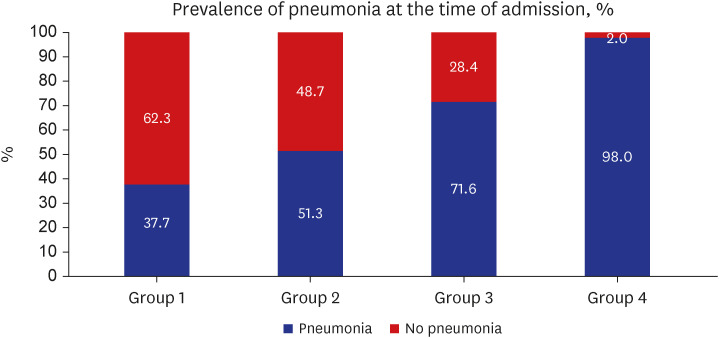
From February 2020 to May 2020, 685 patients (204 males, mean 58 ± 17.9 years) who were diagnosed with COVID-19 and hospitalized were included. We divided patients into four groups according to the severity of symptoms and presence of risk factors (age > 65 years and presence of comorbidities). The patient groups were defined as follows: group 1 (asymptomatic patients), group 2 (patients with mild symptoms without risk factors), group 3 (patients with mild symptoms and risk factors), and group 4 (patients with moderate to severe symptoms). According to the Fleischner society, chest imaging is not indicated for groups 1–2 but is indicated for groups 3–4. We compared the prevalence and score of pneumonia on chest radiographs and compare the adverse outcomes (progress to severe pneumonia, intensive care unit admission, and death) between groups.
Results
Among the 685 COVID-19 patients, 138 (20.1%), 396 (57.8%), 102 (14.9%), and 49 (7.1%) patients corresponded to groups 1 to 4, respectively. Patients in groups 3–4 were significantly older and showed significantly higher prevalence rates of pneumonia (group 1–4: 37.7%, 51.3%, 71.6%, and 98%, respectively, P < 0.001) than those in groups 1-2. Adverse outcomes were also higher in groups 3–4 than in groups 1–2 (group 1–4: 8.0%, 3.5%, 6.9%, and 51%, respectively, P < 0.001). Patients with adverse outcomes in group 1 were initially asymptomatic but symptoms developed during follow-up. They were older (mean age, 80 years) and most of them had comorbidities (81.8%). Consistently asymptomatic patients had no adverse events.
Conclusion
The prevalence of pneumonia and adverse outcomes were different according to the symptoms and risk factors in COVID-19 patients. Therefore, as the Fleischner Society recommended, evaluation and monitoring of COVID-19 pneumonia using chest radiographs is necessary for old symptomatic patients with comorbidities.
Keyword
Figure
Reference
-
1. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020; 382(8):727–733. PMID: 31978945.2. Sung HK, Kim JY, Heo J, Seo H, Jang YS, Kim H, et al. Clinical course and outcomes of 3,060 patients with coronavirus disease 2019 in Korea, January-May 2020. J Korean Med Sci. 2020; 35(30):e280. PMID: 32743995.3. Yoon SH, Ham SY, Nam BD, Chae KJ, Lee D, Yoo JY, et al. Establishment of a nationwide Korean imaging cohort of coronavirus disease 2019. J Korean Med Sci. 2020; 35(46):e413. PMID: 33258333.4. Korean Society of Infectious Diseases and Korea Centers for Disease Control and Prevention. Analysis on 54 mortality cases of coronavirus disease 2019 in the Republic of Korea from January 19 to March 10, 2020. J Korean Med Sci. 2020; 35(12):e132. PMID: 32233161.5. Dyer O. Covid-19: Variants are spreading in countries with low vaccination rates. BMJ. 2021; 373(1359):n1359. PMID: 34039569.6. Lopez Bernal J, Andrews N, Gower C, Gallagher E, Simmons R, Thelwall S, et al. Effectiveness of Covid-19 vaccines against the B.1.617.2 (delta) variant. N Engl J Med. 2021; 385(7):585–594. PMID: 34289274.7. Jin KN, Yoon SH, Park CH, Beck KS, Do KH, Yong HS. KSR/KSTR guidelines for the use of diagnostic imaging for COVID-19. J Korean Soc Radiol. 2020; 81(3):577–582.8. Jung HK, Kim JY, Lee MS, Lee JY, Park JS, Hyun M, et al. Characteristics of COVID-19 patients who progress to pneumonia on follow-up chest radiograph: 236 patients from a single isolated cohort in Daegu, South Korea. Korean J Radiol. 2020; 21(11):1265–1272. PMID: 32729278.9. Rubin GD, Ryerson CJ, Haramati LB, Sverzellati N, Kanne JP, Raoof S, et al. The role of chest imaging in patient management during the COVID-19 pandemic: a multinational consensus statement from the Fleischner Society. Chest. 2020; 158(1):106–116. PMID: 32275978.10. Kuo BJ, Lai YK, Tan ML, Goh XC. Utility of screening chest radiographs in patients with asymptomatic or minimally symptomatic COVID-19 in Singapore. Radiology. 2021; 298(3):E131–E140. PMID: 33289614.11. World Health Organization. Clinical Management of COVID-19 Interim Guidance 2020. Geneva, Switzerland: World Health Organization;2020.12. Borghesi A, Zigliani A, Masciullo R, Golemi S, Maculotti P, Farina D, et al. Radiographic severity index in COVID-19 pneumonia: relationship to age and sex in 783 Italian patients. Radiol Med (Torino). 2020; 125(5):461–464. PMID: 32358691.13. Akl EA, Blažić I, Yaacoub S, Frija G, Chou R, Appiah JA, et al. Use of chest imaging in the diagnosis and management of COVID-19: a WHO rapid advice guide. Radiology. 2021; 298(2):E63–E69. PMID: 32729811.14. Li Y, Shi J, Xia J, Duan J, Chen L, Yu X, et al. Asymptomatic and symptomatic patients with non-severe coronavirus disease (COVID-19) have similar clinical features and virological courses: a retrospective single center study. Front Microbiol. 2020; 11:1570. PMID: 32754137.15. Huang H, Cai S, Li Y, Li Y, Fan Y, Li L, et al. Prognostic factors for COVID-19 pneumonia progression to severe symptoms based on earlier clinical features: a retrospective analysis. Front Med (Lausanne). 2020; 7:557453. PMID: 33123541.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Korean Clinical Imaging Guidelines for Justification of Diagnostic Imaging Study for COVID-19
- Assessment and Management of Dysphagia during the COVID-19 Pandemic
- Role of chest imaging in the diagnosis and treatment of COVID-19
- Response Guidelines for Coronavirus Disease 2019 in Newborn Infants: A 2021 Update
- Cardiovascular Imaging in the Era of the COVID-19 Outbreak