J Korean Neurosurg Soc.
2023 Jul;66(4):418-425. 10.3340/jkns.2022.0259.
Added Predictive Values of Proton Density Magnetic Resonance Imaging on Posterior Communicating Artery Aneurysms and Surrounding Soft Tissues with Simple Classification
- Affiliations
-
- 1Department of Radiology, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Neurosurgery, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Neurosurgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2543533
- DOI: http://doi.org/10.3340/jkns.2022.0259
Abstract
Objective
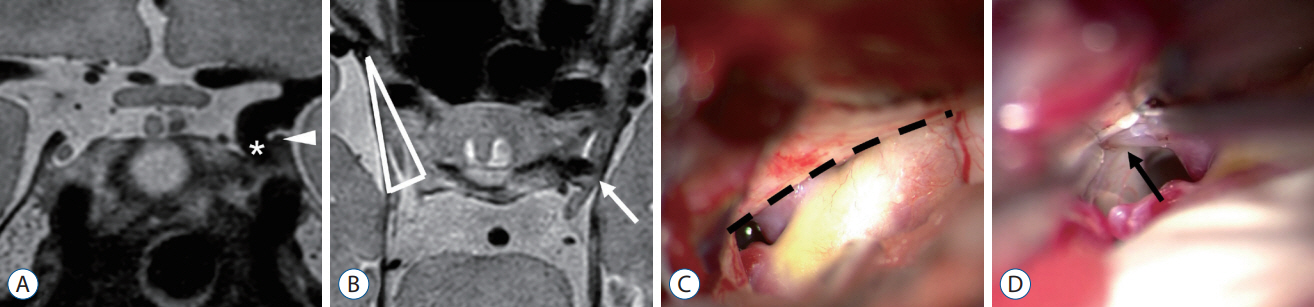
: Deciphering the anatomy of posterior communicating artery (PCoA) aneurysms in relation to surrounding structures is essential to determine adjuvant surgical procedures. However, it is difficult to predict surgical structures through preoperative imaging studies. We aimed to present anatomical structures using preoperative high-resolution three-dimensional proton densityweighted turbo spin-echo magnetic resonance (PDMR) imaging with simple classification.
Methods
: From January 2020 to April 2022, 30 patients underwent PDMR before microsurgical clipping for unruptured PCoA aneurysms in a single tertiary institute. We retrospectively reviewed the radiographic images and operative data of these patients. The structural relationship described by PDMR and intraoperative findings were compared. Subsequently, we classified aneurysms into two groups and analyzed the rate of adjuvant surgical procedures and contact with the surrounding structures.
Results
: Correlations between preoperative PDMR predictions and actual intraoperative findings for PCoA aneurysm contact to the oculomotor nerve, temporal uncus, and anterior petroclinoid fold (APCF) reported a diagnostic accuracy of 0.90, 0.87, and 0.90, respectively. In 12 patients (40.0%), an aneurysm dome was located on the plane of the oculomotor triangle and was classified as the infratentorial type. Compared to the supratentorial type PCoA aneurysm, adjuvant procedures were required more frequently (66.7% vs. 22.2%, p=0.024) for infratentorial type PCoA aneurysm clipping.
Conclusion
: Preoperative PCoA aneurysm categorization using PDMR can be helpful for predicting surgical complexity and planning of microsurgical clipping.
Figure
Reference
-
References
1. Fukuda H, Hayashi K, Yoshino K, Koyama T, Lo B, Kurosaki Y, et al. Impact of aneurysm projection on intraoperative complications during surgical clipping of ruptured posterior communicating artery aneurysms. Neurosurgery. 78:381–390. discussion 390. 2016.
Article2. Golshani K, Ferrell A, Zomorodi A, Smith TP, Britz GW. A review of the management of posterior communicating artery aneurysms in the modern era. Surg Neurol Int. 1:88. 2010.
Article3. González-Darder JM, Quilis-Quesada V, Talamantes-Escribá F, Botella-Maciá L, Verdú-López F. Microsurgical relations between internal carotid artery-posterior communicating artery (ICA-PComA) segment aneurysms and skull base: an anatomoclinical study. J Neurol Surg B Skull Base. 73:337–341. 2012.
Article4. Houkin K, Kuroda S, Takahashi A, Takikawa S, Ishikawa T, Yoshimoto T, et al. Intra-operative premature rupture of the cerebral aneurysms. Analysis of the causes and management. Acta Neurochir (Wien). 141:1255–1263. 1999.
Article5. Kamide T, Burkhardt JK, Tabani H, Safaee MM, Lawton MT. Preoperative prediction of the necessity for anterior clinoidectomy during microsurgical clipping of ruptured posterior communicating artery aneurysms. World Neurosurg. 109:e493–e501. 2018.
Article6. Kim E. Clip compression injury of the oculomotor nerve: its prevention and recovery. Korean J Neurotrauma. 16:85–89. 2020.
Article7. Kim JH, Kim JM, Cheong JH, Bak KH, Kim CH. Simple anterior petroclinoid fold resection in the treatment of low-lying internal carotid-posterior communicating artery aneurysms. Surg Neurol. 72:142–145. 2009.
Article8. Kim JW, Shin NY, Kim YD, Lee SK, Lim SM, Oh SW. Added value of 3D proton-density weighted images in diagnosis of intracranial arterial dissection. PLoS One. 11:e0166929. 2016.
Article9. Kim S, Chung J, Cha J, Kim BM, Kim DJ, Kim YB, et al. Usefulness of high-resolution three-dimensional proton density-weighted turbo spinecho MRI in distinguishing a junctional dilatation from an intracranial aneurysm of the posterior communicating artery: a pilot study. J Neurointerv Surg. 12:315–319. 2020.
Article10. Kuzmik GA, Bulsara KR. Microsurgical clipping of true posterior communicating artery aneurysms. Acta Neurochir (Wien). 154:1707–1710. 2012.
Article11. Lawton MT. Seven Aneurysms: Tenets and Techniques for Clipping. New York: Thieme;2011.12. Lee SH, Jung SC, Kang DW, Kwon SU, Kim JS. Visualization of culprit perforators in anterolateral pontine infarction: high-resolution magnetic resonance imaging study. Eur Neurol. 78:229–233. 2017.
Article13. Matano F, Murai Y, Mizunari T, Yamaguchi M, Yamada T, Baba E, et al. Incision of the anterior petroclinoidal fold during clipping for securing the proximal space of an internal carotid artery-posterior communicating artery aneurysm: a technical note. Neurosurg Rev. 42:777–781. 2019.
Article14. Niibo T, Takizawa K, Sakurai J, Takebayashi S, Koizumi H, Kobayashi T, et al. Prediction of the difficulty of proximal vascular control using 3D-CTA for the surgical clipping of internal carotid artery-posterior communicating artery aneurysms. J Neurosurg. 134:1165–1172. 2020.
Article15. Nossek E, Setton A, Dehdashti AR, Chalif DJ. Anterior petroclinoid fold fenestration: an adjunct to clipping of postero-laterally projecting posterior communicating aneurysms. Neurosurg Rev. 37:637–641. 2014.
Article16. Park SK, Shin YS, Lim YC, Chung J. Preoperative predictive value of the necessity for anterior clinoidectomy in posterior communicating artery aneurysm clipping. Neurosurgery. 65:281–285. discussion 285-286. 2009.
Article17. Sanai N, Caldwell N, Englot DJ, Lawton MT. Advanced technical skills are required for microsurgical clipping of posterior communicating artery aneurysms in the endovascular era. Neurosurgery. 71:285–294. discussion 294-295. 2012.
Article18. Yim Y, Jung SC, Kim JY, Kim SO, Kim BJ, Lee DH, et al. Added diagnostic values of three-dimensional high-resolution proton density-weighted magnetic resonance imaging for unruptured intracranial aneurysms in the circle-of-Willis: comparison with time-of-flight magnetic resonance angiography. PLoS One. 15:e0243235. 2020.
Article19. Yoon SJ, Shin NY, Lee JW, Huh SK, Park KY. Localization and treatment of unruptured paraclinoid aneurysms: a proton density MRI-based study. J Cerebrovasc Endovasc Neurosurg. 17:180–184. 2015.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Localization and Treatment of Unruptured Paraclinoid Aneurysms: A Proton Density MRI-based Study
- True Posterior Communicating Artery Aneurysm
- True Posterior Communicating Artery Aneurysm
- Clinical Analysis of the Pattern of Anterior-Posterior Circulation in Patients with Posterior Communicating Artery Aneurysm
- Physiologic Flow Diversion Coiling Technique for Wide-Necked Aneurysms with an Asymmetric Bidirectional Flow at the Aneurysm Neck