J Cerebrovasc Endovasc Neurosurg.
2023 Jun;25(2):143-149. 10.7461/jcen.2023.E2022.09.001.
Association between ischemic stroke and pyogenic spondylitis in Korea: Nationwide longitudinal cohort study
- Affiliations
-
- 1Department of Neurosurgery, CHA University, CHA Bundang Medical Center, Seongnam, Korea
- 2Genome & Health Big Data Branch, Department of Public Health, Graduate School of Public Health, Seoul National University, Seoul, Korea
- 3Department of Neurosurgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2543510
- DOI: http://doi.org/10.7461/jcen.2023.E2022.09.001
Abstract
Objective
The purpose of this nationwide age- and sex- matched longitudinal study was to determine the pyogenic spondylitis (PS) increases the incidence of ischemic stroke (IS) in Korea.
Methods
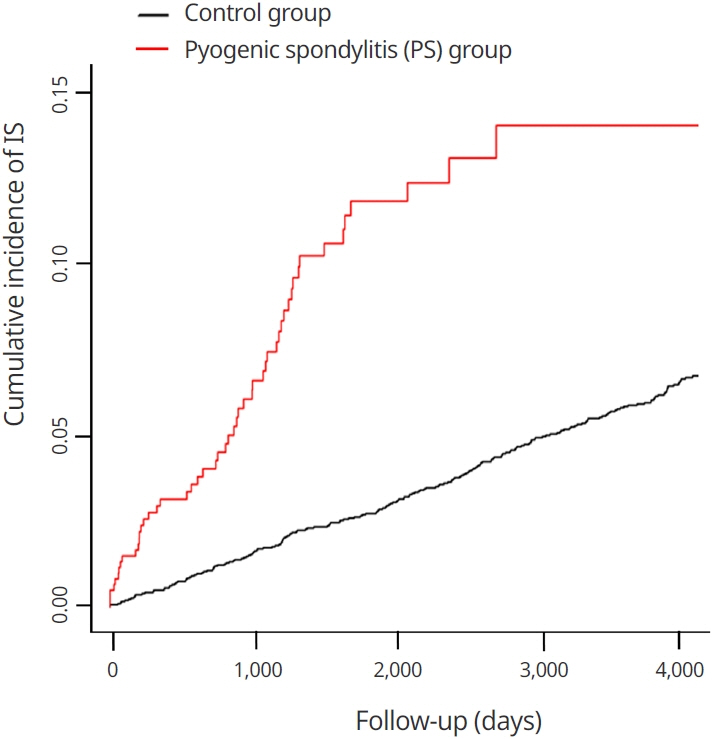
From the National Health Insurance Service (NHIS), we collected the patient data for the period from January 1, 2004 to December 31, 2015. PS was classified according to the International Classification of Disease codes M46.2-M46.8, M49.2, and M49.3. By using a 1:5 age- and sex- stratified matching, a total of 628 patients and 3140 control subjects were included in the study. The IS incidence rates in PS and control group was calculated by using the Kaplan-Meier method. The outcome of hazard ratio of IS was estimated by Cox proportional hazards regression analyses. This study did not exclude PS as a result of postoperative complications.
Results
According to the study, 51 patients (8.12%) in the PS group and 201 patients (6.4%) in the control group experienced IS. The adjusted hazard ratio of IS in the PS group was 3.419 (95% CI: 2.473-4.729) after adjusting individual medical condition and demographics. Following the results of subgroup analysis, the risk ratio of IS was greater in most of the subgroup categories (male, female, age <65, age >65, non-diabetic, hypertensive, non-hypertensive, dyslipidemic and non-dyslipidemic subgroup). However, the risk of IS did not differ significantly in diabetic subgroup (95% CI: 0.953-4.360).
Conclusions
The risk rate of IS increased in patient with pyogenic spondylitis.
Figure
Reference
-
1. Banerjee C, Chimowitz MI. Stroke caused by atherosclerosis of the major intracranial arteries. Circ Res. 2017; Feb. 120(3):502–13.
Article2. Bova IY, Bornstein NM, Korczyn AD. Acute infection as a risk factor for ischemic stroke. Stroke. 1996; Dec. 27(12):2204–6.3. Cheung WY, Luk KDK. Pyogenic spondylitis. Int Orthop. 2012; Feb. 36(2):397–404.
Article4. Cowan LT, Alonso A, Pankow JS, Folsom AR, Rosamond WD, Gottesman RF, et al. Hospitalized infection as a trigger for acute ischemic stroke: the atherosclerosis risk in communities study. Stroke. 2016; Jun. 47(6):1612–7.
Article5. Di Napoli M, Papa F, Bocola V. Prognostic influence of increased C-reactive protein and fibrinogen levels in ischemic stroke. Stroke. 2001; Jan. 32(1):133–8.
Article6. Divecha H, Sattar N, Rumley A, Cherry L, Lowe GD, Sturrock R. Cardiovascular risk parameters in men with ankylosing spondylitis in comparison with non-inflammatory control subjects: relevance of systemic inflammation. Clin Sci (Lond). 2005; Aug. 109(2):171–6.
Article7. Elkind MSV, Boehme AK, Smith CJ, Meisel A, Buckwalter MS. Infection as a stroke risk factor and determinant of outcome after stroke. Stroke. 2020; 51(10):3156–68.
Article8. Emsley HC, Tyrrell PJ. Inflammation and infection in clinical stroke. J Cereb Blood Flow Metab. 2002; Dec. 22(12):1399–419.
Article9. Erren M, Reinecke H, Junker R, Fobker M, Schulte H, Schurek JO, et al. Systemic inflammatory parameters in patients with atherosclerosis of the coronary and peripheral arteries. Arterioscler Thromb Vasc Biol. 1999; Oct. 19(10):2355–63.
Article10. Grau AJ, Buggle F, Heindl S, Steichen-Wiehn C, Banerjee T, Maiwald M, et al. Recent infection as a risk factor for cerebrovascular ischemia. Stroke. 1995; Mar. 26(3):373–9.
Article11. Handa K, Kono S, Saku K, Sasaki J, Kawano T, Sasaki Y, et al. Plasma fibrinogen levels as an independent indicator of severity of coronary atherosclerosis. Atherosclerosis. 1989; Jun. 77(2-3):209–13.
Article12. Ionita CC, Siddiqui AH, Levy EI, Hopkins LN, Snyder KV, Gibbons KJ. Acute ischemic stroke and infections. J Stroke Cerebrovasc Dis. 2011; Jan-Feb. 20(1):1–9.
Article13. Jeong DK, Lee HW, Kwon YM. Clinical value of procalcitonin in patients with spinal infection. J Korean Neurosurg Soc. 2015; Sep. 58(3):271–5.
Article14. Jeong SJ, Choi SW, Youm JY, Kim HW, Ha HG, Yi JS. Microbiology and epidemiology of infectious spinal disease. J Korean Neurosurg Soc. 2014; Jul. 56(1):21–7.
Article15. Kim YJ, Hong JB, Kim YS, Yi J, Choi JM, Sohn S. Change of pyogenic and tuberculous spondylitis between 2007 and 2016 year: a nationwide study. J Korean Neurosurg Soc. 2020; Nov. 63(6):784–93.16. Kim YS, Kim JG, Yi J, Choi JM, Chung CK, Choi UY, et al. Changes in the medical burden of pyogenic and tuberculous spondylitis between 2007 and 2016: a nationwide cohort study. J Clin Neurosci. 2020; Mar. 73:89–93.
Article17. Lee DH, Choi YJ, Han IB, Hong JB, Han KD, Choi JM, et al. Association of ischemic stroke with ankylosing spondylitis: a nationwide longitudinal cohort study. Acta Neurochir (Wien). 2018; May. 160(5):949–55.
Article18. Lee DH, Sheen SH, Lee DG, Jang JW, Lee DC, Shin SH, et al. Association between ischemic stroke and seropositive rheumatoid arthritis in Korea: a nationwide longitudinal cohort study. PloS One. 2021; May. 16(5):e0251851.19. Lee JK, Kim H, Hong JB, Sheen SH, Han IB, Sohn S. Association of acute myocardial infarction with seropositive rheumatoid arthritis in Korea: a nationwide longitudinal cohort study. J Clin Neurosci. 2020; Aug. 78:97–101.
Article20. Levenson J, Giral P, Razavian M, Gariepy J, Simon A. Fibrinogen and silent atherosclerosis in subjects with cardiovascular risk factors. Arterioscler Thromb Vasc Biol. 1995; Sep. 15(9):1263–8.
Article21. McColl B, Allan SM, Rothwell NJ. Systemic infection, inflammation and acute ischemic stroke. Neuroscience. 2009; Feb. 158(3):1049–61.
Article22. Palm F, Pussinen PJ, Aigner A, Becher H, Buggle F, Bauer MF, et al. Association between infectious burden, socioeconomic status, and ischemic stroke. Atherosclerosis. 2016; Nov. 254:117–23.
Article23. Park CJ, Choi YJ, Kim JG, Han IB, Han KD, Choi JM, et al. Association of acute myocardial infarction with ankylosing spondylitis: a nationwide longitudinal cohort study. J Clin Neurosci. 2018; Oct. 56:34–7.
Article24. Rodríguez-Yáñez M, Castillo J. Role of inflammatory markers in brain ischemia. Curr Opin Neurol. 2008; Jun. 21(3):353–7.
Article25. Ross R. Atherosclerosis—an inflammatory disease. N Engl J Med. 1999; Jan. 340(2):115–26.26. Sato K, Yamada K, Yokosuka K, Yoshida T, Goto M, Matsubara T, et al. Pyogenic spondylitis: clinical features, diagnosis and treatment. Kurume Med J. 2019; Sep. 25. 65(3):83–9.
Article27. Sebastian S, Stein LK, Dhamoon MS. Infection as a stroke trigger: associations between different organ system infection admissions and stroke subtypes. Stroke. 2019; Aug. 50(8):2216–8.28. Shao IY, Elkind MS, Boehme AK. Risk factors for stroke in patients with sepsis and bloodstream infections. Stroke. 2019; May. 50(5):1046–51.
Article29. Stoll G, Bendszus M. Inflammation and atherosclerosis: novel insights into plaque formation and destabilization. Stroke. 2006; Jul. 37(7):1923–32.30. Stone M, Thorp J. Plasma fibrinogen—a major coronary risk factor. J R Coll Gen Pract. 1985; Dec. 35(281):565–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- 3 Cases of Pyogenic spondylitis
- Comparison of Pyogenic Spondylitis and Tuberculous Spondylitis
- Latent Multiple Noncontiguous Pyogenic Spondylitis: a case report
- Association of Parkinson’s disease with ischemic stroke in Korea: A nationwide longitudinal cohort study in Korea
- Streptococcus Spondylitis Concomitant Infectious Endocarditis: A Case Report