J Cerebrovasc Endovasc Neurosurg.
2021 Sep;23(3):233-239. 10.7461/jcen.2021.E2021.03.007.
Association of Parkinson’s disease with ischemic stroke in Korea: A nationwide longitudinal cohort study in Korea
- Affiliations
-
- 1Department of Neurosurgery, CHA University, CHA Bundang Medical Center, Seongnam, Korea
- 2Genome & Health Big Data Branch, Department of Public Health, Graduate School of Public Health, Seoul National University, Seoul, Korea
- 3Department of Neurosurgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2520882
- DOI: http://doi.org/10.7461/jcen.2021.E2021.03.007
Abstract
Objective
The aim of this nationwide age- and sex- matched longitudinal follow up study is to determine the risk of Parkinson’s disease (PD) associated with ischemic stroke in Korea.
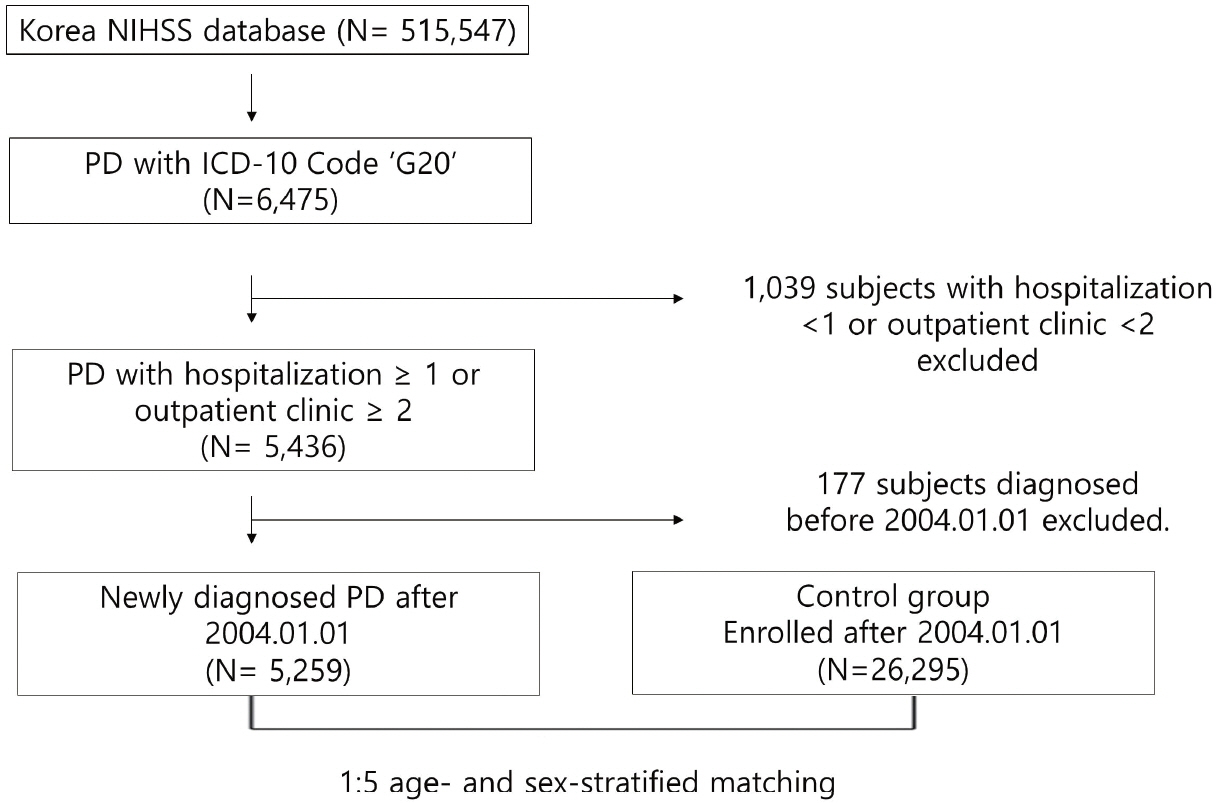
Methods
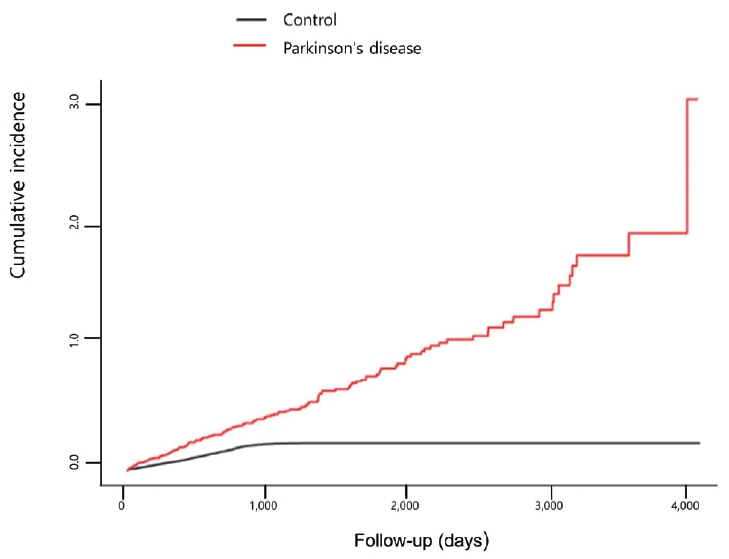
Patient data were collected from the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS). PD was identified using the International Classification of Diseases (ICD) 10-CM code G 20. In total, 6,475 patients were enrolled in the PD group from the NHISS. After subtracting 1,039 patients who underwent hospitalization less than once or those who visited an outpatient clinic less than two times, 5,259 patients who were diagnosed after January 1, 2004 ultimately participated in this study. After case-control match was done through 1:5 age- and sex- stratified matching, 26,295 individuals were chosen as control. Kaplan-Meier method and Cox proportional hazard regression analysis were performed to evaluate the risk of ischemic stroke in PD.
Results
The hazard ratio of ischemic stroke in the PD group was 3.848 (95% confidence interval (confidence interval [CI]): 3.14-4.70) after adjusting for age and sex. The adjusted hazard ratio of ischemic stroke in PD group was 3.885 (95% CI: 3.17-4.75) after adjusting for comorbidities. According to subgroup analysis, in male and female and non-diabetes and diabetes and non-hypertension and hypertension and dyslipidemia and non-dyslipidemia subgroups, ischemic stroke incidence rates were significantly higher in the PD group than those in the control group.
Conclusions
This nationwide longitudinal study suggests an increased risk of ischemic stroke in PD patients.
Keyword
Figure
Reference
-
1. Bae KH, Hong JB, Choi YJ, Jung JH, Han IB, Choi JM, et al. Association of congestive heart failure and death with ankylosing spondylitis: a nationwide longitudinal cohort study in Korea. J Korean Neurosurg Soc. 2019; Mar. 62(2):217–24.2. Becker C, Jick SS, Meier CR. Risk of stroke in patients with idiopathic Parkinson disease. Parkinsonism Relat Disord. 2010; Jan. 16(1):31–5.
Article3. Ben-Shlomo Y, Marmot MG. Survival and cause of death in a cohort of patients with parkinsonism: possible clues to aetiology? J Neurol Neurosurg Psychiatry. 1995; Mar. 58(3):293–9.
Article4. de Lau LM, Breteler MM. Epidemiology of Parkinson’s disease. Lancet Neurol. 2006; Jun. 5(6):525–35.
Article5. Elkind MS, Ramakrishnan P, Moon YP, Boden-Albala B, Liu KM, Spitalnik SL, et al. Infectious burden and risk of stroke: the northern Manhattan study. Arch Neurol. 2010; Jan. 67(1):33–8.6. Gorell JM, Johnson CC, Rybicki BA. Parkinson’s disease and its comorbid disorders: an analysis of Michigan mortality data, 1970 to 1990. Neurology. 1994; Oct. 44(10):1865–8.
Article7. Harrison D, Griendling KK, Landmesser U, Hornig B, Drexler H. Role of oxidative stress in atherosclerosis. Am J Cardiol. 2003; Feb. 91(3A):7A–11A.
Article8. Ho D, Imai K, King G, Stuart EA. MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Soft. 2011; May. 42(8):1–28.
Article9. Ho DE, Imai K, King G, Stuart EA. Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Political Analysis. 2007; 15(3):199–236.
Article10. Hoshi T, Kitagawa K, Yamagami H, Furukado S, Hougaku H, Hori M. Relations of serum high-sensitivity C-reactive protein and interleukin-6 levels with silent brain infarction. Stroke. 2005; Apr. 36(4):768–72.
Article11. Huang YP, Chen LS, Yen MF, Fann CY, Chiu YH, Chen HH, et al. Parkinson’s disease is related to an increased risk of ischemic stroke-a population-based propensity score-matched follow-up study. PLoS One. 2013; Sep. 8(9):e68314.
Article12. Jenner P. Oxidative stress in Parkinson’s disease. Ann Neurol. 2003; Mar. 53 Suppl 3:S26–38.
Article13. Kang SH, Choi EK, Han KD, Lee SR, Lim WH, Cha MJ, et al. Underweight is a risk factor for atrial fibrillation: A nationwide population-based study. Int J Cardiol. 2016; Jul. 215:449–56.
Article14. Kim YS, Kim JG, Yi J, Choi JM, Chung CK, Choi UY, et al. Changes in the medical burden of pyogenic and tuberculous spondylitis between 2007 and 2016: A nationwide cohort study. J Clin Neurosci. 2020; Mar. 73:89–93.
Article15. Korten A, Lodder J, Vreeling F, Boreas A, van Raak L, Kessels F. Stroke and idiopathic Parkinson’s disease: does a shortage of dopamine offer protection against stroke? Mov Disord. 2001; Jan. 16(1):119–23.
Article16. Lee DH, Choi YJ, Han IB, Hong JB, Do Han K, Choi JM, et al. Association of ischemic stroke with ankylosing spondylitis: a nationwide longitudinal cohort study. Acta Neurochir (Wien). 2018; May. 160(5):949–55.
Article17. Lim SY, Lang AE. The nonmotor symptoms of Parkinson’s disease--an overview. Mov Disord. 2010; 25 Suppl 1:S123–30.
Article18. McDonald C, Newton JL, Burn DJ. Orthostatic hypotension and cognitive impairment in Parkinson’s disease: Causation or association? Mov Disord. 2016; Jul. 31(7):937–46.
Article19. Park CJ, Choi YJ, Kim JG, Han IB, Do Han K, Choi JM, et al. Association of acute myocardial infarction with ankylosing spondylitis: a nationwide longitudinal cohort study. J Clin Neurosci. 2018; Oct. 56:34–7.
Article20. Park CS, Choi EK, Han KD, Lee HJ, Rhee TM, Lee SR, et al. Association between adult height, myocardial infarction, heart failure, stroke and death: a Korean nationwide population-based study. Int J Epidemiol. 2018; Feb. 47(1):289–98.
Article21. Rektor I, Goldemund D, Sheardová K, Rektorová I, Michálková Z, Dufek M. Vascular pathology in patients with idiopathic Parkinson’s disease. Parkinsonism Relat Disord. 2009; Jan. 15(1):24–9.
Article22. Roos RA, Jongen JC, van der Velde EA. Clinical course of patients with idiopathic Parkinson’s disease. Mov Disord. 1996; May. 11(3):236–42.
Article23. Scigliano G, Musicco M, Soliveri P, Piccolo I, Ronchetti G, Girotti F. Reduced risk factors for vascular disorders in Parkinson disease patients: a case-control study. Stroke. 2006; May. 37(5):1184–8.24. Seong SC, Kim YY, Park SK, Khang YH, Kim HC, Park JH, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open. 2017; Sep. 7(9):e016640.
Article25. Simanek AM, Dowd JB, Pawelec G, Melzer D, Dutta A, Aiello AE. Seropositivity to cytomegalovirus, inflammation, all-cause and cardiovascular disease-related mortality in the United States. PLoS One. 2011; Feb. 6(2):e16103.
Article26. Song IU, Lee JE, Kwon DY, Park JH, Ma HI. Parkinson’s disease might increase the risk of cerebral ischemic lesions. Int J Med Sci. 2017; Mar. 14(4):319–22.
Article27. Struck LK, Rodnitzky RL, Dobson JK. Stroke and its modification in Parkinson’s disease. Stroke. 1990; Oct. 21(10):1395–9.
Article28. Velseboer DC, de Haan RJ, Wieling W, Goldstein DS, de Bie RM. Prevalence of orthostatic hypotension in Parkinson’s disease: a systematic review and meta-analysis. Parkinsonism Relat Disord. 2011; Dec. 17(10):724–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Association between the Triglyceride-Glucose Index and the Incidence Risk of Parkinson’s Disease: A Nationwide Cohort Study
- Ischemic Stroke Associated with Orthostasis in an Advanced Parkinson's Disease Patient with Orthostatic Hypotension
- Diagnosis of Cerebrovascular Disease
- Current Opinion on the Role of Neurogenesis in the Therapeutic Strategies for Alzheimer Disease, Parkinson Disease, and Ischemic Stroke; Considering Neuronal Voiding Function
- Neurologic Diseases in the Elderly