Ann Rehabil Med.
2023 Jun;47(3):192-204. 10.5535/arm.23018.
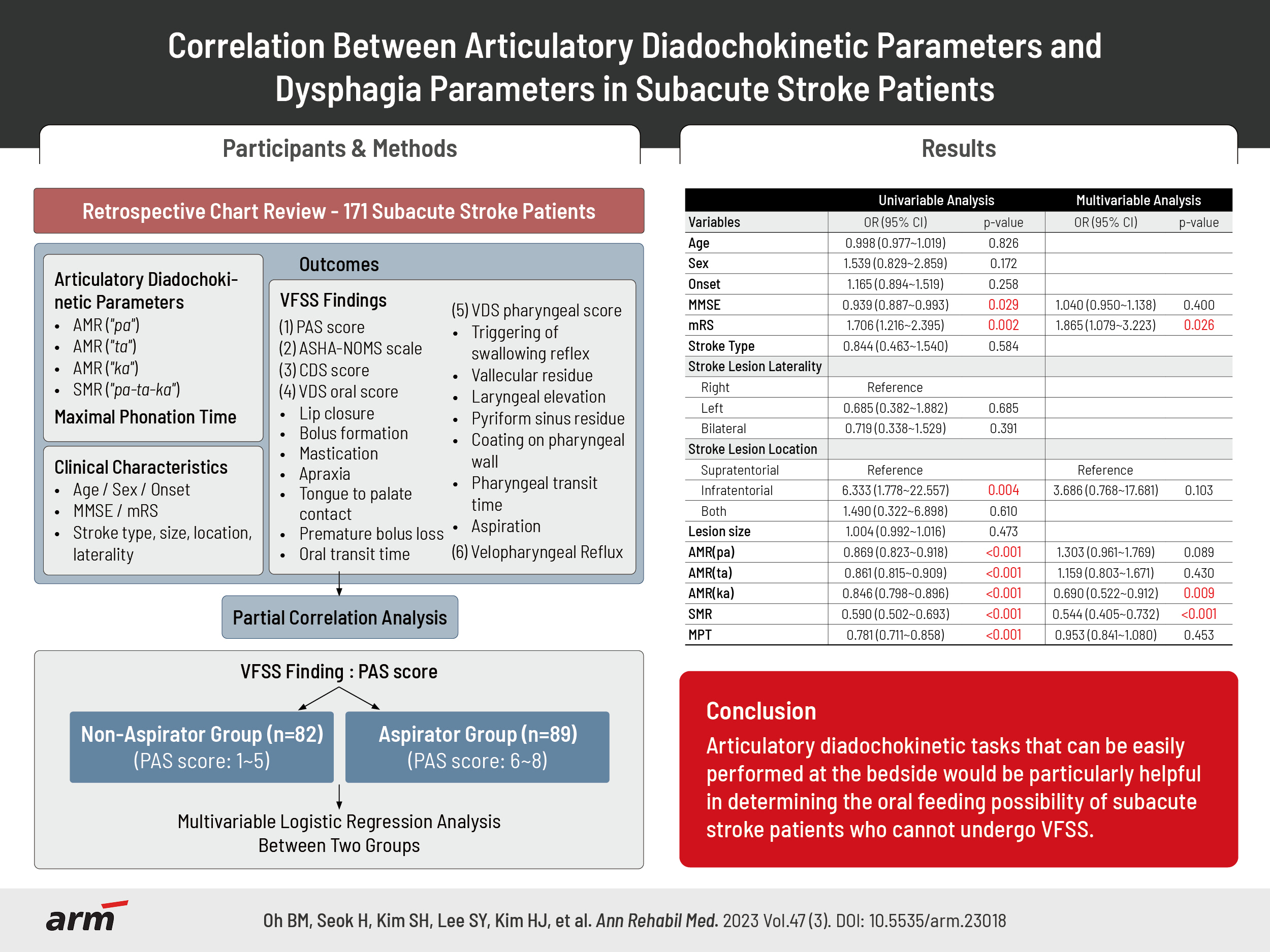
Correlation Between Articulatory Diadochokinetic Parameters and Dysphagia Parameters in Subacute Stroke Patients
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea
- KMID: 2543416
- DOI: http://doi.org/10.5535/arm.23018
Abstract
Objective
To determine correlations of alternation motor rate (AMR), sequential motor rate (SMR), and maximum phonation time (MPT) with the severity of dysphagia in subacute stroke patients.
Methods
This was a retrospective chart review study. Data of 171 subacute stroke patients were analyzed. Patient’s AMR, SMR, and MPT data were collected from their language evaluations. Video fluoroscopic swallowing study (VFSS) was done. Data of dysphagia scales including penetration-aspiration scale (PAS), American Speech-Language-Hearing Association National Outcomes Measurement System (ASHA-NOMS) scale, clinical dysphagia scale (CDS), and videofluoroscopic dysphagia scale (VDS) were obtained. AMR, SMR, and MPT were compared between a non-aspirator group and an aspirator group. Correlations of AMR, SMR, and MPT with dysphagia scales were analyzed.
Results
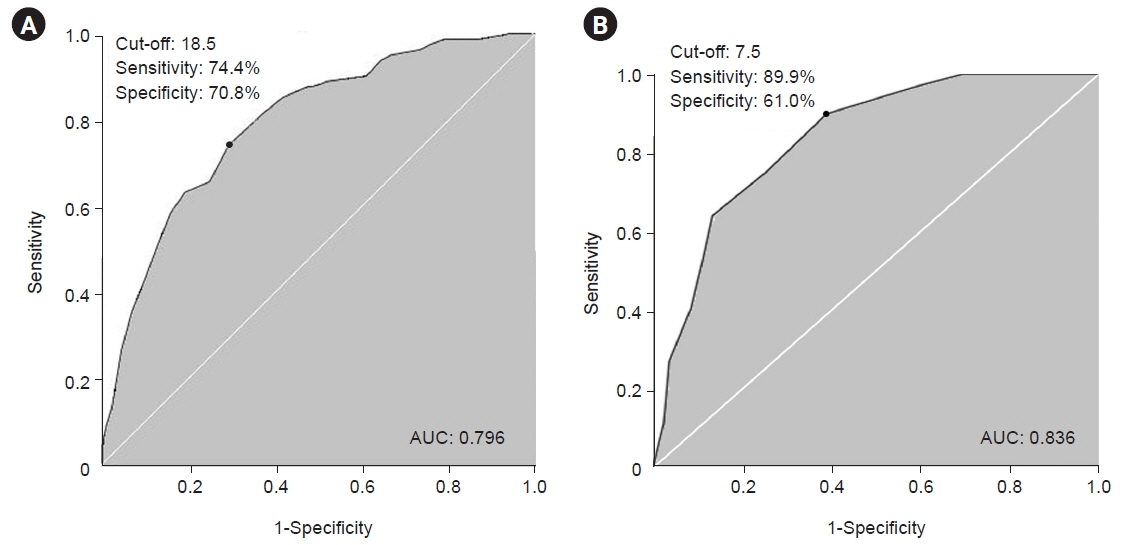
AMR ("ka"), SMR, and modified Rankin Scale were significant associated factors between non-aspirator group and aspirator group, while AMR ("pa"), AMR ("ta"), and MPT were not. AMR, SMR, and MPT showed significant correlations with PAS score, ASHA-NOMS scale, CDS, VDS oral, and VDS pharyngeal scores. The cut-off value for distinguishing non-aspirator group and aspiration group was 18.5 for AMR ("ka") (sensitivity of 74.4%, specificity of 70.8%) and 7.5 for SMR (sensitivity of 89.9%, specificity of 61.0%). AMR and SMR were significantly lower in before-swallow aspiration group.
Conclusion
Articulatory diadochokinetic tasks that can be easily performed at the bedside would be particularly helpful in determining the oral feeding possibility of subacute stroke patients who cannot undergo VFSS, which is the gold standard for dysphagia assessment.
Keyword
Figure
Reference
-
1. Knuijt S, Kalf JG, de Swart BJ, Drost G, Hendricks HT, Geurts AC, et al. Dysarthria and dysphagia are highly prevalent among various types of neuromuscular diseases. Disabil Rehabil. 2014; 36:1285–9.
Article2. Bahia MM, Mourão LF, Chun RY. Dysarthria as a predictor of dysphagia following stroke. NeuroRehabilitation. 2016; 38:155–62.
Article3. Flowers HL, Silver FL, Fang J, Rochon E, Martino R. The incidence, co-occurrence, and predictors of dysphagia, dysarthria, and aphasia after first-ever acute ischemic stroke. J Commun Disord. 2013; 46:238–48.
Article4. Falsetti P, Acciai C, Palilla R, Bosi M, Carpinteri F, Zingarelli A, et al. Oropharyngeal dysphagia after stroke: incidence, diagnosis, and clinical predictors in patients admitted to a neurorehabilitation unit. J Stroke Cerebrovasc Dis. 2009; 18:329–35.
Article5. Ludlow CL. Central nervous system control of voice and swallowing. J Clin Neurophysiol. 2015; 32:294–303.
Article6. Kwon YG, Do KH, Park SJ, Chang MC, Chun MH. Effect of repetitive transcranial magnetic stimulation on patients with dysarthria after subacute stroke. Ann Rehabil Med. 2015; 39:793–9.
Article7. Kim HJ, Lee KM. Development of the Korea Dysarthria Test following stroke. Ann Rehabil Med. 2022; 46:71–86.
Article8. Shin MJ, Kim JO, Lee SB, Lee SY. Speech mechanism screening test (SMST). Seoul: Hakjisa;2010.9. Kim SJ, Shin JY. Articulatory and phonological disorders. Seoul: Sigmapress;2007.10. Fletcher SG. Time-by-count measurement of diadochokinetic syllable rate. J Speech Hear Res. 1972; 15:763–70.
Article11. Matsuo K, Palmer JB. Anatomy and physiology of feeding and swallowing: normal and abnormal. Phys Med Rehabil Clin N Am. 2008; 19:691–707. vii.12. Goyal R, Mashimo H. Physiology of oral, pharyngeal, and esophageal motility [Internet]. GI Motility Online; 2006 [cited 2022 Dec 1]. Available from: https://www.nature.com/gimo/contents/pt1/full/gimo1.html.13. Kodama N, Kumai Y, Miyamoto T, Matsubara K, Samejima Y, Orita Y. Factors affecting the swallowing dysfunction following oral cancer surgery. Ann Rehabil Med. 2021; 45:368–78.
Article14. Yamaguchi S, Ishida M, Hidaka K, Gomi S, Takayama S, Sato K, et al. Relationship between swallowing function and breathing/phonation. Auris Nasus Larynx. 2018; 45:533–9.
Article15. Maslan J, Leng X, Rees C, Blalock D, Butler SG. Maximum phonation time in healthy older adults. J Voice. 2011; 25:709–13.
Article16. Solomon NP, Garlitz SJ, Milbrath RL. Respiratory and laryngeal contributions to maximum phonation duration. J Voice. 2000; 14:331–40.
Article17. Eibling DE, Gross RD. Subglottic air pressure: a key component of swallowing efficiency. Ann Otol Rhinol Laryngol. 1996; 105:253–8.
Article18. Nakayama H, Jørgensen HS, Raaschou HO, Olsen TS. The influence of age on stroke outcome. The Copenhagen Stroke Study. Stroke. 1994; 25:808–13.
Article19. Tanaka T, Kagaya H, Ozeki Y, Fujii W, Iida T, Shibata S, et al. Revised classification of aspiration before, during, and after the swallow and its reliability. Jpn J Compr Rehabilit Sci. 2016; 7:51–4.
Article20. Jung SH, Lee KJ, Hong JB, Han TR. Validation of clinical dysphagia scale: based on videofluoroscopic swallowing study. J Korean Acad Rehabilit Med. 2005; 29:343–50.21. Chang MC, Kwak S. Videofluoroscopic swallowing study findings associated with subsequent pneumonia in patients with dysphagia due to frailty. Front Med (Lausanne). 2021; 8:690968.
Article22. Han TR, Paik NJ, Park JW, Kwon BS. The prediction of persistent dysphagia beyond six months after stroke. Dysphagia. 2008; 23:59–64.
Article23. American Speech-Language-Hearing Association. National Outcomes Measurement System (NOMS): adult speech-language pathology user’s guide. Rockville: American Speech-Language-Hearing Association;2002.24. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New York: Lawrence Erlbaum Associates;1988.25. Ko EJ, Chae M, Cho SR. Relationship between swallowing function and maximum phonation time in patients with Parkinsonism. Ann Rehabil Med. 2018; 42:425–32.
Article26. Ko JY, Shin DY, Kim TU, Kim SY, Hyun JK, Lee SJ. Predictors of aspiration pneumonia in the elderly with swallowing dysfunction: videofluoroscopic swallowing study. Ann Rehabil Med. 2021; 45:99–107.
Article27. Nishino T. The swallowing reflex and its significance as an airway defensive reflex. Front Physiol. 2013; 3:489.
Article28. Park A, Jang SJ, Kim NE, Kim TH, Sohn YH, Kim H, et al. Swallowing outcomes following voice therapy in multiple system atrophy with dysphagia: comparison of treatment efficacy with Parkinson's disease. Dysphagia. 2022; 37:198–206.
Article29. Ruda JM, Krakovitz P, Rose AS. A review of the evaluation and management of velopharyngeal insufficiency in children. Otolaryngol Clin North Am. 2012; 45:653–69. viii.
Article30. Clavé P, de Kraa M, Arreola V, Girvent M, Farré R, Palomera E, et al. The effect of bolus viscosity on swallowing function in neurogenic dysphagia. Aliment Pharmacol Ther. 2006; 24:1385–94.
Article31. Lee JH, Kim HS, Yun DH, Chon J, Han YJ, Yoo SD, et al. The relationship between tongue pressure and oral dysphagia in stroke patients. Ann Rehabil Med. 2016; 40:620–8.
Article32. Knack AF. Evaluating the relationship between diadochokinesis and severity of dysphagia as it relates to forced vital capacity in individuals with amyotrophic lateral sclerosis [dissertation]. Detroit, MI: Wayne State University;2015.33. Wang YT, Kent RD, Duffy JR, Thomas JE. Dysarthria associated with traumatic brain injury: speaking rate and emphatic stress. J Commun Disord. 2005; 38:231–60.
Article34. Nishio M, Niimi S. Comparison of speaking rate, articulation rate and alternating motion rate in dysarthric speakers. Folia Phoniatr Logop. 2006; 58:114–31.
Article35. Cho H, Noh JS, Park J, Park C, Park ND, Ahn JY, et al. Decreased maximal tongue protrusion length may predict the presence of dysphagia in stroke patients. Ann Rehabil Med. 2021; 45:440–9.
Article36. Lee SM, Lee BH, Kim JW, Jang JY, Jang EG, Ryu JS. Effects of chin-down maneuver on pharyngeal pressure generation according to dysphagia and viscosity. Ann Rehabil Med. 2020; 44:493–501.
Article37. Kim HD, Choi JB, Yoo SJ, Chang MY, Lee SW, Park JS. Tongue-to-palate resistance training improves tongue strength and oropharyngeal swallowing function in subacute stroke survivors with dysphagia. J Oral Rehabil. 2017; 44:59–64.
Article38. Park HS, Oh DH, Yoon T, Park JS. Effect of effortful swallowing training on tongue strength and oropharyngeal swallowing function in stroke patients with dysphagia: a double-blind, randomized controlled trial. Int J Lang Commun Disord. 2019; 54:479–84.
Article39. Moon JH, Hong DG, Kim KH, Park YA, Hahm SC, Kim SJ, et al. Effects of lingual strength training on lingual strength and articulator function in stroke patients with dysarthria. J Phys Ther Sci. 2017; 29:1201–4.
Article40. Choi J, Baek S, Kim G, Park HW. Peak voluntary cough flow and oropharyngeal dysphagia as risk factors for pneumonia. Ann Rehabil Med. 2021; 45:431–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidemiology, Natural Recovery, Long-term Outcome of Post Stroke Dysphagia
- Changes of the Platelet Parameters in Cerebral Infarction
- Association between Location of Brain Lesion and Clinical Factors and Findings of Videofluoroscopic Swallowing Study in Subacute Stroke Patients
- A Correlation Study of Parameters from MRI and PET in Acute Stroke
- Relationship Between Cognitive Function and Dysphagia After Stroke