Ann Rehabil Med.
2023 Jun;47(3):173-181. 10.5535/arm.22153.
Impact of Extra-Corporeal Membrane Oxygenation and Blood Purification Therapy on Early Mobilization in the Intensive Care Unit: Retrospective Cohort Study
- Affiliations
-
- 1Department of Rehabilitation Medicine, National Hospital Organization, Nagoya Medical Center, Nagoya, Japan
- 2Department of Physical Therapy, Faculty of Rehabilitation, Gifu University of Health Science, Gifu, Japan
- 3Department of Physical Therapy, School of Health Sciences, Toyohashi Sozo University, Toyohashi, Japan
- 4Department of Rehabilitation Medicine, Tosei General Hospital, Seto, Japan
- 5Department of Rehabilitation Medicine, National Hospital Organization, Shizuoka Medical Center, Shizuoka, Japan
- 6Department of Rehabilitation Medicine, Ichinomiyanishi Hospital, Ichinomiya, Japan
- 7Department of Rehabilitation, Toyohashi Municipal Hospital, Toyohashi, Japan
- 8Department of Rehabilitation Medicine, Kainan Hospital, Yatomi, Japan
- 9Department of Emergency Medicine, National Hospital Organization, Nagoya Medical Center, Nagoya, Japan
- KMID: 2543414
- DOI: http://doi.org/10.5535/arm.22153
Abstract
Objective
To investigate the effect on early mobilization in patients undergoing extra-corporeal membrane oxygenation (ECMO) and acute blood purification therapy in the intensive care unit (ICU).
Methods
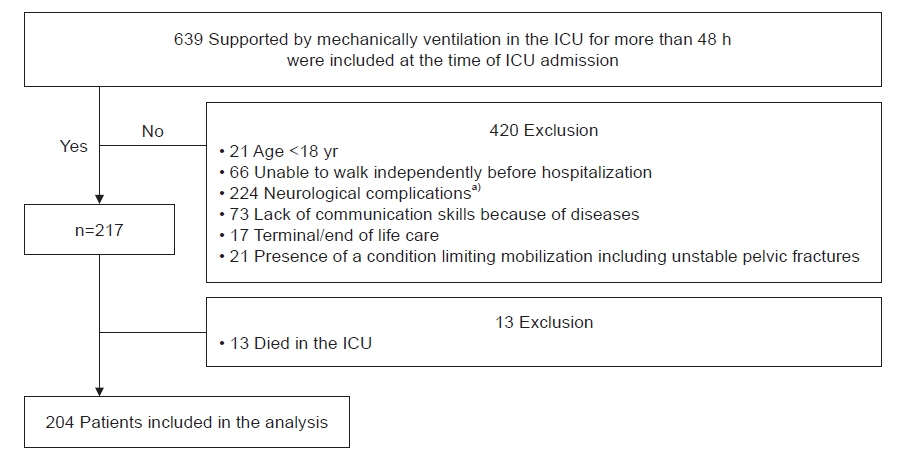
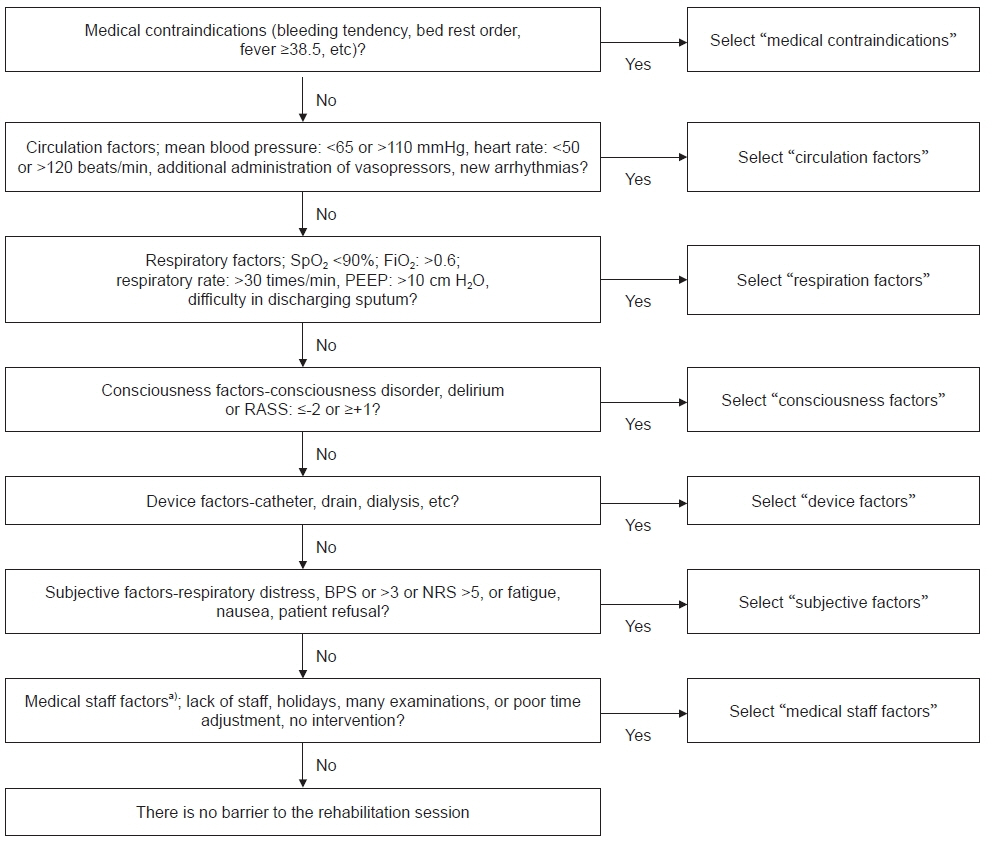
We conducted this multicenter retrospective cohort study by collecting data from six ICUs in Japan. Consecutive patients who were admitted to the ICU, aged ≥18 years, and received mechanical ventilation for >48 hours were eligible. The analyzed were divided into two groups: ECMO/blood purification or control group. Clinical outcomes; time to first mobilization, number of total ICU rehabilitations, mean and highest ICU mobility scale (IMS); and daily barrier changes were also investigated.
Results
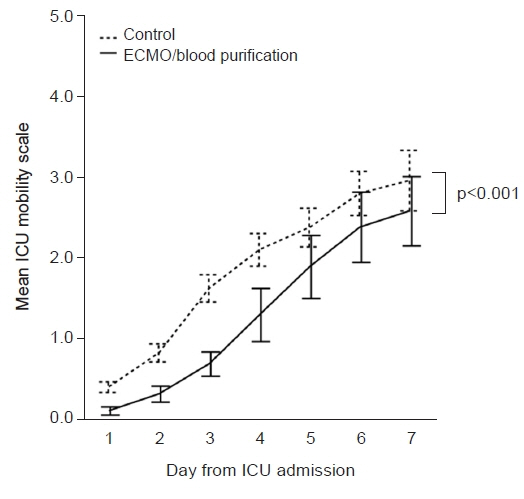
A total of 204 patients were included in the analysis, 43 in the ECMO/blood purification group and 161 in the control group. In comparison of clinical outcome, the ECMO/blood purification group had a significantly longer time to first mobilization: ECMO/blood purification group 6 vs. control group 4 (p=0.003), higher number of total ICU rehabilitations: 6 vs. 5 (p=0.042), lower mean: 0 vs. 1 (p=0.043) and highest IMS: 2 vs. 3 (p=0.039) during ICU stay. Circulatory factor were most frequently described as barriers to early mobilization on days 1 (51%), 2 (47%), and 3 (26%). On days 4 to 7, the most frequently described barrier was consciousness factors (21%, 16%, 19%, and 21%, respectively)
Conclusion
The results of this study comparing the ECMO/blood purification group and the untreated group in the ICU showed that the ECMO/blood purification group had significantly longer days to mobilization and significantly lower mean and highest IMS.
Keyword
Figure
Reference
-
1. Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders' conference. Crit Care Med. 2012; 40:502–9.2. Ministry of Health, Labor and Welfare (Japan). Reiwa 4-year Revision of Medical Fees I-3-9. Revision of the upper limit of calculation days for emergency hospitalization charges [Internet]. Tokyo: Ministry of Health, Labor and Welfare;2022. [cited 2022 Oct 10]. Available from: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000188411_00037.html.3. Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009; 373:1874–82.
Article4. Morris PE, Berry MJ, Files DC, Thompson JC, Hauser J, Flores L, et al. Standardized rehabilitation and hospital length of stay among patients with acute respiratory failure: a randomized clinical trial. JAMA. 2016; 315:2694–702.
Article5. Watanabe S, Liu K, Nakamura K, Kozu R, Horibe T, Ishii K, et al. Association between early mobilization in the ICU and psychiatric symptoms after surviving a critical illness: a multi-center prospective cohort study. J Clin Med. 2022; 11:2587.
Article6. Watanabe S, Kotani T, Taito S, Ota K, Ishii K, Ono M, et al. Determinants of gait independence after mechanical ventilation in the intensive care unit: a Japanese multicenter retrospective exploratory cohort study. J Intensive Care. 2019; 7:53.
Article7. Ad Hoc Committee for Early Rehabilitation; The Japanese Society of Intensive Care Medicine. [Evidence based expert consensus for early rehabilitation in the intensive care unit]. J Jpn Soc Intensive Care Med. 2017; 24:255–303. Japanese.8. Watanabe S, Liu K, Morita Y, Kanaya T, Naito Y, Arakawa R, et al. Changes in barriers to implementing early mobilization in the intensive care unit: a single center retrospective cohort study. Nagoya J Med Sci. 2021; 83:443–64.9. Yasuda H, Kato A, Fujigaki Y, Hishida A; Shizuoka Kidney Disease Study Group. Incidence and clinical outcomes of acute kidney injury requiring renal replacement therapy in Japan. Ther Apher Dial. 2010; 14:541–6.
Article10. Hodgson C, Needham D, Haines K, Bailey M, Ward A, Harrold M, et al. Feasibility and inter-rater reliability of the ICU Mobility Scale. Heart Lung 2014;43:19-24. Erratum in: Heart Lung. 2014; 43:388.11. Hermans G, Casaer MP, Clerckx B, Güiza F, Vanhullebusch T, Derde S, et al. Effect of tolerating macronutrient deficit on the development of intensive-care unit acquired weakness: a subanalysis of the EPaNIC trial. Lancet Respir Med. 2013; 1:621–9.
Article12. Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, et al. Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med. 2001; 29:1370–9.
Article13. Watanabe S, Morita Y, Suzuki S, Kochi K, Ohno M, Liu K, et al. Effects of the intensity and activity time of early rehabilitation on activities of daily living dependence in mechanically ventilated patients. Prog Rehabil Med. 2021; 6:20210054.
Article14. Watanabe S, Iida Y, Ito T, Mizutani M, Morita Y, Suzuki S, et al. Effect of early rehabilitation activity time on critically Ill patients with intensive care unit-acquired weakness: a Japanese retrospective multicenter study. Prog Rehabil Med. 2018; 3:20180003.
Article15. Suzuki M, Oya H, Ishihara Y. [Practice of ICU nurses caring for patients undergoing blood purification therapy: the approach at our ICU]. J Jpn Soc Blood Purif Crit Care. 2020; 11:128–32. Japanese.16. Scheffenbichler FT, Teja B, Wongtangman K, Mazwi N, Waak K, Schaller SJ, et al. Effects of the level and duration of mobilization therapy in the surgical ICU on the loss of the ability to live independently: an international prospective cohort study. Crit Care Med. 2021; 49:e247–57.
Article17. TEAM Study Investigators and the ANZICS Clinical Trials Group. Early active mobilization during mechanical ventilation in the ICU. N Engl J Med. 2022; 387:1747–58.18. Ministry of Health, Labor and Welfare (Japan). Central social insurance medical council general assembly (493rd) proceedings. Source: 2019 DPC data [Internet. Tokyo: Ministry of Health, Labor and Welfare;2022. [cited 2022 Oct 10]. Available from: https://www.mhlw.go.jp/stf/shingi2/0000212500_00115.html.19. Watanabe S, Hirasawa J, Naito Y, Mizutani M, Uemura A, Nishimura S, et al. Association between the early mobilization of mechanically ventilated patients and independence in activities of daily living at hospital discharge. Sci Rep. 2023; 13:4265.
Article20. TEAM Study Investigators. Early mobilization and recovery in mechanically ventilated patients in the ICU: a bi-national, multi-centre, prospective cohort study. Crit Care. 2015; 19:81.21. Devlin JW, Skrobik Y, Gélinas C, Needham DM, Slooter AJC, Pandharipande PP, et al. Clinical practice guidelines for the prevention and management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep disruption in adult patients in the ICU. Crit Care Med. 2018; 46:e825–73.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Improving mobility in the intensive care unit with a protocolized, early mobilization program: observations of a single center before-and-after the implementation of a multidisciplinary program
- Extracorporeal Membrane Oxygenation Therapy for Aspiration Pneumonia in a Patient following Left Pneumonectomy for Lung Cancer
- Transjugular central venous catheter guidewire embolism to venoarterial extracorporeal membrane oxygenation cannula
- Blood Transfusion Strategies in Patients Supported by Extracorporeal Membrane Oxygenation
- Rehabilitation in Intensive Care Unit