Korean J Crit Care Med.
2016 May;31(2):156-161. 10.4266/kjccm.2016.31.2.156.
Extracorporeal Membrane Oxygenation Therapy for Aspiration Pneumonia in a Patient following Left Pneumonectomy for Lung Cancer
- Affiliations
-
- 1Department of Trauma Surgery, Korea University Guro Hospital, Seoul, Korea.
- 2Department of Thracic and Cardiovascular Surgery, Korea University Guro Hospital, Seoul, Korea. kumgaek@medigate.net
- KMID: 2350925
- DOI: http://doi.org/10.4266/kjccm.2016.31.2.156
Abstract
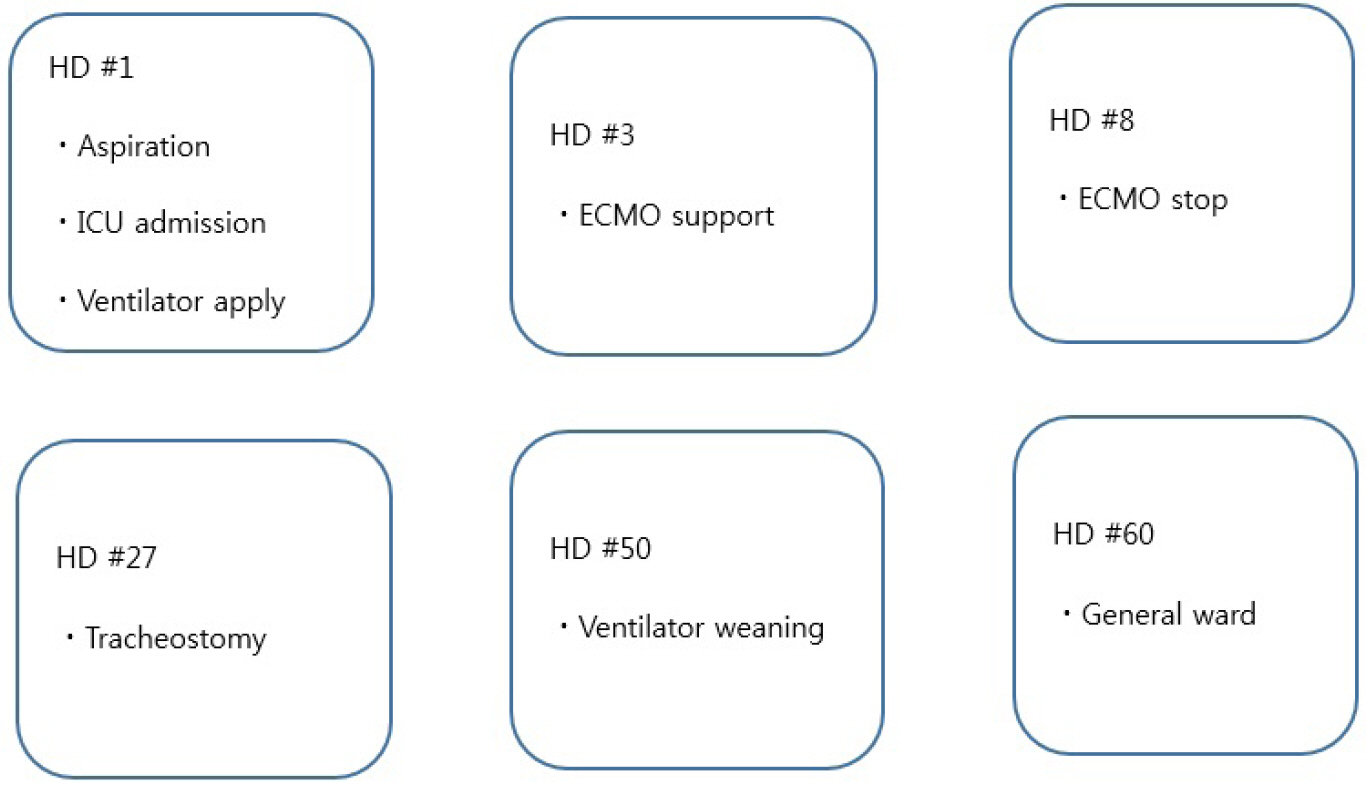
- A patient had undergone left pneumonectomy for lung cancer and had an increased risk of fatal complications such as pneumonia, including acute respiratory distress syndrome (ARDS). The treatment effects of veno-venous extracorporeal membrane oxygenation (VV-ECMO) for ARDS of postpneumonectomy patient are uncertain. A 74-year-old man with one lung experienced aspiration pneumonia while swallowing pills after the operation, and his condition progressed to ARDS within a day. He was successfully treated with VV-ECMO support and intensive care unit care.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
The Future of Research on Extracorporeal Membrane Oxygenation (ECMO)
Ji Young Lee
Korean J Crit Care Med. 2016;31(2):73-75. doi: 10.4266/kjccm.2016.31.2.73.
Reference
-
References
1. Engelhardt T, Webster NR. Pulmonary aspiration of gastric contents in anaesthesia. Br J Anaesth. 1999; 83:453–60.
Article2. Warner MA, Warner ME, Weber JG. Clinical significance of pulmonary aspiration during the perioperative period. Anesthesiology. 1993; 78:56–62.
Article3. Kim N, Kim KH, Kim JM, Choi SY, Na S. Early extracorporeal membrane oxygenation for massive aspiration during anesthesia induction. Korean J Crit Care Med. 2015; 30:109–14.
Article4. Harpole DH, Liptay MJ, DeCamp MM Jr., Mentzer SJ, Swanson SJ, Sugarbaker DJ. Prospective analysis of pneumonectomy: risk factors for major morbidity and cardiac dysrhythmias. Ann Thorac Surg. 1996; 61:977–82.
Article5. Diaz JV, Brower R, Calfee CS, Matthay MA. Therapeutic strategies for severe acute lung injury. Crit Care Med. 2010; 38:1644–50.
Article6. Enger T, Philipp A, Videm V, Lubnow M, Wahba A, Fischer M, et al. Prediction of mortality in adult patients with severe acute lung failure receiving venovenous extracorporeal membrane oxygenation: a prospective observational study. Crit Care. 2014; 18:R67.
Article7. Saueressig MG, Schwarz P, Schlatter R, Moreschi AH, Wender OC, Macedo-Neto AV. Extracorporeal membrane oxygenation for postpneumonectomy ARDS. J Bras Pneumol. 2014; 40:203–6.
Article8. Martucci G, Panarello G, Bertani A, Occhipinti G, Pintaudi S, Arcadipane A. Veno-venous ECMO in ARDS after post-traumatic pneumonectomy. Intensive Care Med. 2013; 39:2235–6.
Article9. Powell ES, Pearce AC, Cook D, Davies P, Bishay E, Bowler GM, et al. UK pneumonectomy outcome study (UKPOS): a prospective observational study of pneumonectomy outcome. J Cardiothorac Surg. 2009; 4:41.
Article10. Deslauriers J, Ugalde P, Miro S, Deslauriers DR, Ferland S, Bergeron S, et al. Long-term physiological consequences of pneumonectomy. Semin Thorac Cardiovasc Surg. 2011; 23:196–202.
Article11. Smulders SA, Smeenk FW, Janssen-Heijnen ML, Postmus PE. Actual and predicted postoperative changes in lung function after pneumonectomy: a retrospective analysis. Chest. 2004; 125:1735–41.12. Deslauriers J, Ugalde P, Miro S, Ferland S, Bergeron S, Lacasse Y, et al. Adjustments in cardiorespiratory function after pneumonectomy: results of the pneumonectomy project. J Thorac Cardiovasc Surg. 2011; 141:7–15.
Article13. Nugent AM, Steele IC, Carragher AM, McManus K, McGuigan JA, Gibbons JR, et al. Effect of thoracotomy and lung resection on exercise capacity in patients with lung cancer. Thorax. 1999; 54:334–8.
Article14. Larsen KR, Svendsen UG, Milman N, Brenøe J, Petersen BN. Cardiopulmonary function at rest and during exercise after resection for bronchial carcinoma. Ann Thorac Surg. 1997; 64:960–4.15. Pelletier C, Lapointe L, LeBlanc P. Effects of lung resection on pulmonary function and exercise capacity. Thorax. 1990; 45:497–502.
Article16. Vainshelboim B, Fox BD, Saute M, Sagie A, Yehoshua L, Fuks L, et al. Limitations in exercise and functional capacity in long-term postpneumonectomy patients. J Cardiopulm Rehabil Prev. 2015; 35:56–64.
Article17. Anand S. Aspiration pneumonitis and pneumonia. 2015. [2015 April]. Available from http://emedicine.medscape.com/article/296198-overview.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Whole Lung Lavage and Extracorporeal Membrane Oxygenation in a Patient with Pulmonary Alveolar Proteinosis and Lung Cancer
- Whole Lung Lavage in Pulmonary Alveolar Proteinosis associated with Lung Cancer Using Extracorporeal Membrane Oxygenation (ECMO)
- Early Extracorporeal Membrane Oxygenation for Massive Aspiration during Anesthesia Induction
- Percutaneous Extracorporeal Membrane Oxygenation (ECMO) for Acute Fulminant Myocarditis
- Sequential Bilateral Lung Transplantation with Extracorporeal Membrane Oxygenation (ECMO) Support: A case report