Neurointervention.
2023 Jul;18(2):140-144. 10.5469/neuroint.2023.00045.
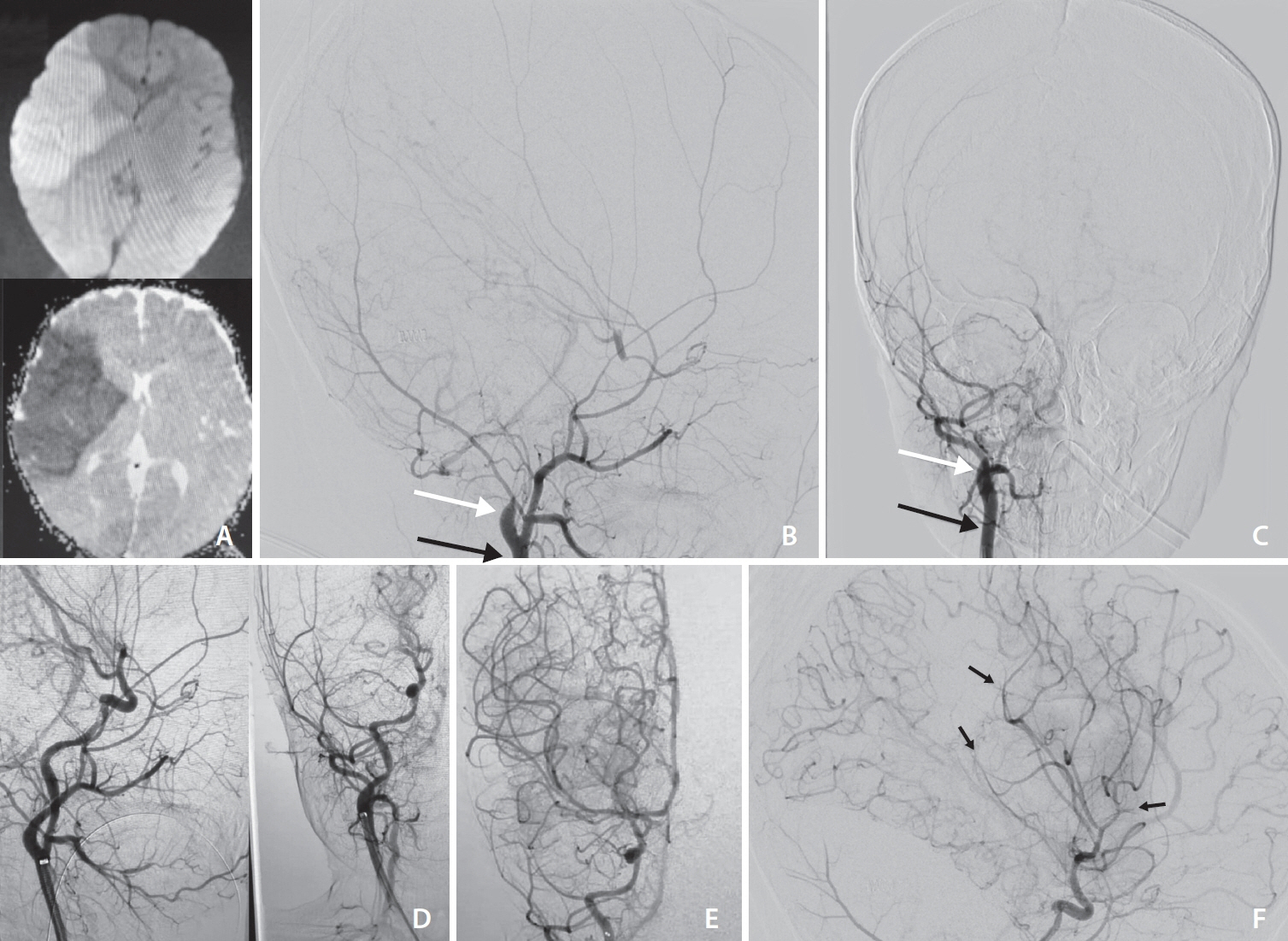
Mechanical Thrombectomy in a 12-Month-Old Infant with Acute Ischemic Stroke Possibly due to Internal Carotid Artery Dissection: A Case Report
- Affiliations
-
- 1Division of Neurovascular Intervention, Department of Neurosurgery, Mashhad University of Medical Sciences, Mashhad, Iran
- 2School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran
- 3Hematologic Malignancies Research Institute, Beckman Research Institute, City of Hope, Duarte, CA, USA
- 4Division of Stroke and Endovascular Neurosurgery, Department of Neurological Surgery, Keck School of Medicine, University of Southern California (USC), Los Angeles, CA, USA
- 5Department of Interventional Neuroradiology, Fondation Rothschild Hospital, Paris, France
- KMID: 2543370
- DOI: http://doi.org/10.5469/neuroint.2023.00045
Abstract
- Stroke in children is a rare but devastating disease. Although endovascular treatment has been reported to be safe and effective in the treatment of stroke with large vessel occlusion in this population, there are still limitations and controversies. In this case report, we describe a 12-month-old girl who was admitted to the hospital with acute onset of left-sided hemiplegia and confusion, which turned out to be due to a large infarct in the right middle cerebral artery territory, possibly caused by dissection of the right cervical internal carotid artery. Aspiration thrombectomy was successfully performed, and the patient was able to walk a few steps and raise her left upper extremity at the 12-month follow-up. The aspiration-only technique in thrombectomy may be safe and technically feasible to treat acute ischemic stroke with large vessel occlusion in children as young as 12 months, although large-volume prospective studies are needed.
Keyword
Figure
Reference
-
1. Shoirah H, Shallwani H, Siddiqui AH, Levy EI, Kenmuir CL, Jovin TG, et al. Endovascular thrombectomy in pediatric patients with large vessel occlusion. J Neurointerv Surg. 2019; 11:729–732.
Article2. Sporns PB, Fullerton HJ, Lee S, Kim H, Lo WD, Mackay MT, et al. Childhood stroke. Nat Rev Dis Primers. 2022; 8:12.
Article3. Bhogal P, Hellstern V, AlMatter M, Ganslandt O, Bäzner H, Aguilar Pérez M, et al. Mechanical thrombectomy in children and adolescents: report of five cases and literature review. Stroke Vasc Neurol. 2018; 3:245–252.
Article4. Ganesan V, Prengler M, McShane MA, Wade AM, Kirkham FJ. Investigation of risk factors in children with arterial ischemic stroke. Ann Neurol. 2003; 53:167–173.
Article5. Goeggel Simonetti B, Cavelti A, Arnold M, Bigi S, Regényi M, Mattle HP, et al. Long-term outcome after arterial ischemic stroke in children and young adults. Neurology. 2015; 84:1941–1947.
Article6. Ganesan V, Prengler M, Wade A, Kirkham FJ. Clinical and radiological recurrence after childhood arterial ischemic stroke. Circulation. 2006; 114:2170–2177.
Article7. Madaelil TP, Kansagra AP, Cross DT, Moran CJ, Derdeyn CP. Mechanical thrombectomy in pediatric acute ischemic stroke: clinical outcomes and literature review. Interv Neuroradiol. 2016; 22:426–431.
Article8. Kaur N, Patel S, Ayanbadejo MO, Hoffman H, Akano E, Anikpezie N, et al. Age-specific trends in intravenous thrombolysis and mechanical thrombectomy utilization in acute ischemic stroke in children under age 18. Int J Stroke. 2023; 18:469–476.
Article9. Staby I, Krogh J, Klose M, Baekdal J, Feldt-Rasmussen U, Poulsgaard L, et al. Pituitary function after transsphenoidal surgery including measurement of basal morning cortisol as predictor of adrenal insufficiency. Endocr Connect. 2021; 10:750–757.
Article10. Nash M, Rafay MF. Craniocervical arterial dissection in children: pathophysiology and management. Pediatr Neurol. 2019; 95:9–18.
Article11. Fullerton HJ, Johnston SC, Smith WS. Arterial dissection and stroke in children. Neurology. 2001; 57:1155–1160.
Article12. Stence NV, Fenton LZ, Goldenberg NA, Armstrong-Wells J, Bernard TJ. Craniocervical arterial dissection in children: diagnosis and treatment. Curr Treat Options Neurol. 2011; 13:636–648.
Article13. Scoville J, Joyce E, Harper J, Hunsaker J, Gren L, Porucznik C, et al. A survey and analysis of pediatric stroke protocols. J Stroke Cerebrovasc Dis. 2022; 31:106661.
Article14. Christi AY, Suroto NS, Bajamal Z, Al Fauzi A. Primary mechanical thrombectomy for anterior circulation stroke in children: report of two cases and literature review. Int J Surg Case Rep. 2021; 89:106655.
Article15. Sporns PB, Kemmling A, Hanning U, Minnerup J, Sträter R, Niederstadt T, et al. Thrombectomy in childhood stroke. J Am Heart Assoc. 2019; 8:e011335.
Article16. Sun LR, Felling RJ, Pearl MS. Endovascular mechanical thrombectomy for acute stroke in young children. J Neurointerv Surg. 2019; 11:554–558.
Article17. He L, Ladner TR, Pruthi S, Day MA, Desai AA, Jordan LC, et al. Rule of 5: angiographic diameters of cervicocerebral arteries in children and compatibility with adult neurointerventional devices. J Neurointerv Surg. 2016; 8:1067–1071.
Article18. Gandhe RU, Bhave CP, Kakde AS, Sathe KA. Endovascular aspiration of clot in a 3-year-old child with embolic infarct of right middle cerebral artery. Saudi J Anaesth. 2018; 12:643–645.
Article19. Aburto-Murrieta Y, Méndez B, Marquez-Romero JM. Extended time window mechanical thrombectomy for pediatric acute ischemic stroke. J Cent Nerv Syst Dis. 2022; 14:11795735221098140.
Article20. Sarraj A, Hassan AE, Abraham MG, Ortega-Gutierrez S, Kasner SE, Hussain MS, et al. Trial of endovascular thrombectomy for large ischemic strokes. N Engl J Med. 2023; 388:1259–1271.21. Yoshimura S, Sakai N, Yamagami H, Uchida K, Beppu M, Toyoda K, et al. Endovascular therapy for acute stroke with a large ischemic region. N Engl J Med. 2022; 386:1303–1313.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Simultaneous Onset of Ischemic and Hemorrhagic Stroke Due To Intracranial Artery Dissection
- Endovascular Revascularization Therapy in a Patient with Acute Ischemic Stroke due to Intracranial Multiple Large-vessel Occlusion
- Alternative Transcarotid Approach for Endovascular Treatment of Acute Ischemic Stroke Patients: A Case Series
- Endovascular recanalization therapy for patients with acute ischemic stroke with hidden aortic dissection: A case series
- Acute Ischemic Stroke Involving Both Anterior and Posterior Circulation Treated by Endovascular Revascularization for Acute Basilar Artery Occlusion via Persistent Primitive Trigeminal Artery