Neurointervention.
2023 Jul;18(2):114-122. 10.5469/neuroint.2023.00199.
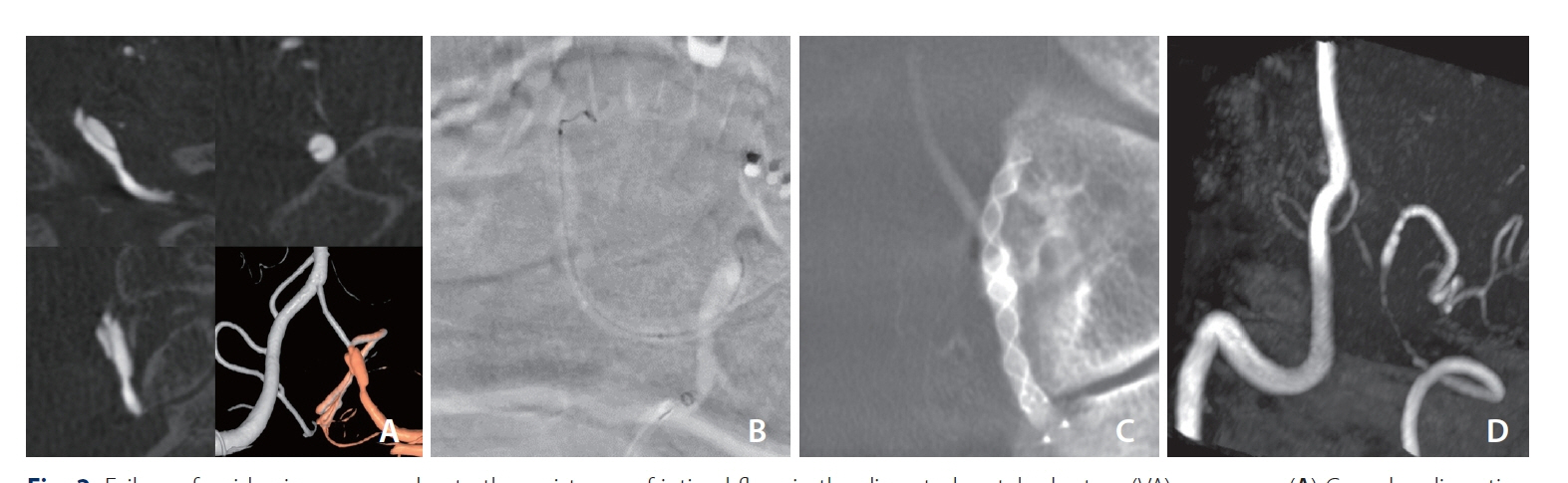
Flow Diverter Treatment Using a Flow Re-Direction Endoluminal Device for Unruptured Intracranial Vertebral Artery Dissecting Aneurysm: Single-Center Case Series and Technical Considerations
- Affiliations
-
- 1Neurointervention Clinic, Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Neurointervention, Gangnam St. Peter’s Hospital, Seoul, Korea
- 3Department of Radiology, Chung-Ang University Hospital, Seoul, Korea
- KMID: 2543366
- DOI: http://doi.org/10.5469/neuroint.2023.00199
Abstract
- Purpose
This study aimed to evaluate the effectiveness, safety, and technical considerations of flow diverter (FD) treatment using a Flow Re-direction Endoluminal Device (FRED) for unruptured intracranial vertebral artery dissecting aneurysms (VADAs).
Materials and Methods
We conducted a retrospective study of 23 patients with unruptured intracranial VADAs who underwent FD treatment using a FRED between June 2017 and August 2021. Symptoms, imaging findings, treatment strategies, and angiographic and clinical outcomes were evaluated. Dissections were categorized according to the dominance of the VA in which they occurred: dominant VA, co-dominant VA, and non-dominant VA.
Results
All patients successfully underwent FD treatment with either a FRED (n=11) or FRED Jr. (n=12). Complete occlusion rates were 78.3% at 6-month follow-up magnetic resonance angiography and 91.3% at 12-month. There were no instances of complications, recurrence, or retreatment during a median follow-up of 20 months. Dissections occurred in the dominant VA in 3 cases (13.0%), the co-dominant VA in 13 cases (56.5%), and the non-dominant VA in 7 cases (30.4%). Intimal flap and true lumen stenosis were observed in 39.1% and 30.4% of cases, respectively. Four cases required a bilateral VA approach due to technical difficulties, all in the non-dominant VA.
Conclusion
Flow diversion treatment using a FRED for unruptured intracranial VADAs proved feasible and safe, yielding satisfactory occlusion rates. Technical challenges were more likely in lesions involving non-dominant VAs in the acute or subacute stage, mainly due to associated intraluminal lesions compromising the arterial lumen.
Keyword
Figure
Reference
-
1. Debette S, Compter A, Labeyrie MA, Uyttenboogaart M, Metso TM, Majersik JJ, et al. Epidemiology, pathophysiology, diagnosis, and management of intracranial artery dissection. Lancet Neurol. 2015; 14:640–654.2. Putaala J, Metso AJ, Metso TM, Konkola N, Kraemer Y, Haapaniemi E, et al. Analysis of 1008 consecutive patients aged 15 to 49 with first-ever ischemic stroke: the Helsinki young stroke registry. Stroke. 2009; 40:1195–1203.3. Kwak JH, Choi JW, Park HJ, Chae EY, Park ES, Lee DH, et al. Cerebral artery dissection: spectrum of clinical presentations related to angiographic findings. Neurointervention. 2011; 6:78–83.4. Tsukahara T, Minematsu K. Overview of spontaneous cervicocephalic arterial dissection in Japan. Acta Neurochir Suppl. 2010; 107:35–40.5. Huang YC, Chen YF, Wang YH, Tu YK, Jeng JS, Liu HM. Cervicocranial arterial dissection: experience of 73 patients in a single center. Surg Neurol. 2009; 72 Suppl 2:S20–S27. discussion S27.6. Song Y, Park SI, Budianto P, Kwon B, Suh DC. Clinical manifestation and radiologic patterns of spontaneous cervicocephalic dissection according to the anatomic location: a single-center analysis in Korean patients. Neurointervention. 2022; 17:78–86.7. Song Y, Lee JK, Lee JO, Kwon B, Seo EJ, Suh DC. Whole exome sequencing in patients with phenotypically associated familial intracranial aneurysm. Korean J Radiol. 2022; 23:101–111.
Article8. Song Y, Kwon B, Al-Abdulwahhab AH, Nam YK, Ahn Y, Jeong SY, et al. Rare neurovascular diseases in Korea: classification and related genetic variants. Korean J Radiol. 2021; 22:1379–1396.
Article9. Mizutani T, Kojima H, Asamoto S, Miki Y. Pathological mechanism and three-dimensional structure of cerebral dissecting aneurysms. J Neurosurg. 2001; 94:712–717.
Article10. Chen M. Intracranial dissections. In : Baumgartner RW, Bogousslavsky J, Caso V, Paciaroni M, editors. Handbook on cerebral artery dissection. Karger;2005. p. 160–173.11. Catapano JS, Ducruet AF, Cadigan MS, Farhadi DS, Majmundar N, Nguyen CL, et al. Endovascular treatment of vertebral artery dissecting aneurysms: a 20-year institutional experience. J Neurointerv Surg. 2022; 14:257–261.
Article12. Sönmez Ö, Brinjikji W, Murad MH, Lanzino G. Deconstructive and reconstructive techniques in treatment of vertebrobasilar dissecting aneurysms: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2015; 36:1293–1298.
Article13. Cagnazzo F, Lefevre PH, Derraz I, Dargazanli C, Gascou G, di Carlo DT, et al. Flow-diversion treatment for unruptured nonsaccular intracranial aneurysms of the posterior and distal anterior circulation: a meta-analysis. AJNR Am J Neuroradiol. 2020; 41:134–139.
Article14. Krings T, Choi IS. The many faces of intracranial arterial dissections. Interv Neuroradiol. 2010; 16:151–160.
Article15. Oh HS, Bae JW, Hong CE, Kim KM, Yoo DH, Kang HS, et al. Flow diverter in unruptured intracranial vertebral artery dissecting aneurysm. Front Neurol. 2022; 13:912863.
Article16. Liu P, Li Z, Hu L, Liu Y, Li P, Zhu W, et al. Clinical characteristics, endovascular choices, and surgical outcomes of intracranial vertebral artery dissecting aneurysms: a consecutive series of 196 patients. J Neurosurg. 2022; 138:215–222.
Article17. Li L, Xu GQ, Gao HL, Gao BL, Zhang K, Wang ZL, et al. Endovascular treatment of intracranial vertebral artery unruptured dissecting aneurysms: comparison of flow diversion and stent-assisted coiling or stenting alone. Front Neurol. 2022; 13:919866.
Article18. Lee W, Han HJ, Kim J, Park KY, Kim YB, Jang CK, et al. Flow diverter for the treatment of large (>10 mm) vertebral artery dissecting aneurysms. Acta Neurochir (Wien). 2022; 164:1247–1254.
Article19. Kim CH, Lee CH, Kim YH, Sung SK, Son DW, Lee SW, et al. Flow diverter devices for the treatment of unruptured vertebral artery dissecting aneurysm. J Korean Neurosurg Soc. 2021; 64:891–900.
Article20. Fu W, Ge H, Luo G, Meng X, Wang J, Jin H, et al. Treatment of unruptured vertebral artery aneurysm involving posterior inferior cerebellar artery with pipeline embolization device. Front Neurol. 2021; 12:622457.
Article21. Gölitz P, Struffert T, Hoelter P, Eyüpoglu I, Knossalla F, Doerfler A. Flow-diverting stents allow efficient treatment of unruptured, intradural dissecting aneurysms of the vertebral artery: an explanatory approach using in vivo flow analysis. Interv Neuroradiol. 2016; 22:76–83.
Article22. Debette S, Leys D. Cervical-artery dissections: predisposing factors, diagnosis, and outcome. Lancet Neurol. 2009; 8:668–678.
Article23. Shin JH, Suh DC, Choi CG, Leei HK. Vertebral artery dissection: spectrum of imaging findings with emphasis on angiography and correlation with clinical presentation. Radiographics. 2000; 20:1687–1696.
Article24. Songur A, Gonul Y, Ozen OA, Kucuker H, Uzun I, Bas O, et al. Variations in the intracranial vertebrobasilar system. Surg Radiol Anat. 2008; 30:257–264.
Article25. Kurniawan RG, Song Y, Kwon B, Ahn Y, Suh DC. Tailored antiplatelet agent medication in clopidogrel hyporesponsive patients before stent-assisted coiling: single-center experience. Neuroradiology. 2020; 62:1709–1715.
Article26. Suh DC, Choi YH, Park SI, Yun S, Jeong SY, Jeong S, et al. Outpatient day-care management of unruptured intracranial aneurysm: a retrospective cohort study. Korean J Radiol. 2022; 23:828–834.
Article27. Lee D, Song Y, Han M, Park D, Suh DC. Low-dose prasugrel in patients with resistance to clopidogrel for the treatment of cerebral aneurysms. Neurointervention. 2018; 13:124–127.
Article28. Lee D, Song Y, Shin JH, Suh DC. Low-dose prasugrel in patients with resistance to clopidogrel for the treatment of cerebral aneurysms: follow-up of over 6 months. Neurointervention. 2019; 14:68–70.
Article29. Kiyofuji S, Graffeo CS, Perry A, Murad MH, Flemming KD, Lanzino G, et al. Meta-analysis of treatment outcomes of posterior circulation non-saccular aneurysms by flow diverters. J Neurointerv Surg. 2018; 10:493–499.
Article30. Adeeb N, Ogilvy CS, Griessenauer CJ, Thomas AJ. Expanding the indications for flow diversion: treatment of posterior circulation aneurysms. Neurosurgery. 2020; 86(Suppl 1):S76–S84.
Article31. Lopes DK, Jang DK, Cekirge S, Fiorella D, Hanel RA, Kallmes DF, et al. Morbidity and mortality in patients with posterior circulation aneurysms treated with the pipeline embolization device: a subgroup analysis of the international retrospective study of the pipeline embolization device. Neurosurgery. 2018; 83:488–500.
Article32. Mizutani T, Miki Y, Kojima H, Suzuki H. Proposed classification of nonatherosclerotic cerebral fusiform and dissecting aneurysms. Neurosurgery. 1999; 45:253–259. discussion 259-260.
Article33. Guimaraens L, Vivas E, Saldaña J, Llibre JC, Gil A, Balaguer E, et al. Efficacy and safety of the dual-layer flow-diverting stent (FRED) for the treatment of intracranial aneurysms. J Neurointerv Surg. 2020; 12:521–525.
Article34. Ahmed SU, Mocco J, Zhang X, Kelly M, Doshi A, Nael K, et al. MRA versus DSA for the follow-up imaging of intracranial aneurysms treated using endovascular techniques: a meta-analysis. J Neurointerv Surg. 2019; 11:1009–1014.
Article35. Halitcan B, Bige S, Sinan B, Ilkay A, Ergun D, Fatih A, et al. The implications of magnetic resonance angiography artifacts caused by different types of intracranial flow diverters. J Cardiovasc Magn Reson. 2021; 23:69.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Migration of Pipeline Embolization Device Causing Rupture during Treatment of an Unruptured Vertebral Artery Dissecting Aneurysm
- Flow Diverter Device for Treatment of Cerebral Aneurysm with Short-Term Follow Up: Two Case Reports
- Treatment of Intracranial Aneurysms with Flow Re-direction Endoluminal Device - A Single Centre Experience with Short-term Follow-up Results
- Multiple telescopic stenting versus single flow diverter for the treatment of vertebral artery dissecting aneurysm
- Internal Carotid Artery Reconstruction with a “Mega Flow Diverterâ€: First Experience with the 6×50 mm DERIVO Embolization Device