J Korean Med Sci.
2023 May;38(21):e163. 10.3346/jkms.2023.38.e163.
Preoperative Prognostic Nutritional Index Is a Prognostic Indicator of Cancer-Specific Survival in Patients Undergoing Endometrial Cancer Surgery
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Obstetrics and Gynecology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 3Department of Anesthesiology and Pain Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2542600
- DOI: http://doi.org/10.3346/jkms.2023.38.e163
Abstract
- Background
The prognostic nutritional index (PNI) reflects systemic inflammation and nutritional status. This study aimed to evaluate the effect of preoperative PNI on postoperative cancer-specific survival in patients with endometrial cancer (EC).
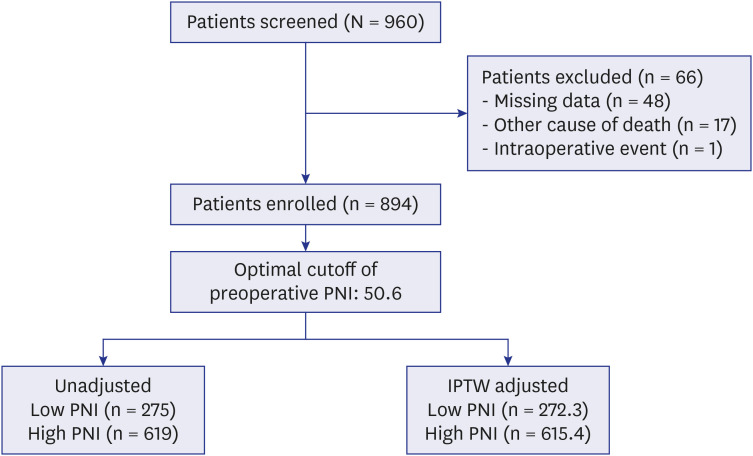
Methods
Demographic, laboratory, and clinical data were retrospectively collected from 894 patients who underwent surgical resection of EC. Preoperative PNIs were determined from the serum albumin concentration and total lymphocyte count, which were measured within 1 month before surgery. Patients were classified into high PNI (n = 619) and low PNI (n = 275) groups according to the preoperative PNI cut-off value of 50.6. The stabilized inverse probability of treatment weighting (IPTW) method was used to reduce bias: a weighting cohort divided into high PNI (n = 615.4) and low PNI (n = 272.3) groups. The primary outcome measure was postoperative cancer-specific survival.
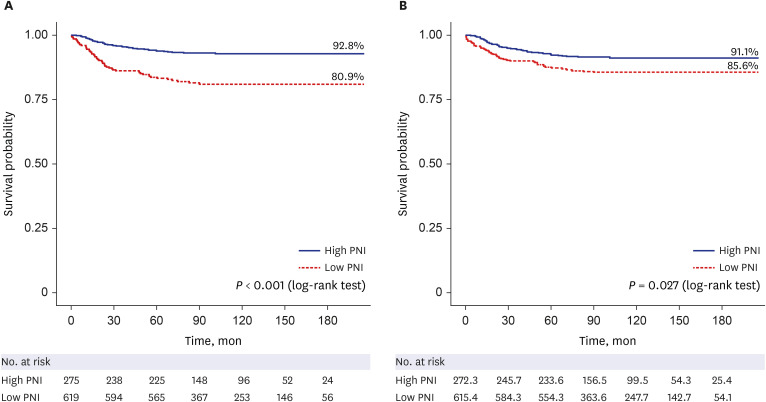
Results
The postoperative cancer-specific survival rate was higher in the high PNI group than the low PNI group in the unadjusted cohort (93.1% vs. 81.5%; proportion difference [95% confidence interval; 95% CI], 11.6% [6.6–16.6%]; P < 0.001) and in the IPTW- adjusted cohort (91.4% vs. 86.0%; 5.4% [0.8–10.2%]; P = 0.021). In the multivariate Cox proportional hazard regression model in the IPTW-adjusted cohort, high preoperative PNI (hazard ratio [95% CI], 0.60 [0.38–0.96]; P = 0.032) was an independent determinant of postoperative cancer-specific mortality. The multivariate-adjusted restricted cubic spline curve for the Cox regression model showed a significant negative association between preoperative PNI and postoperative cancer-specific mortality (P < 0.001).
Conclusion
High preoperative PNI was associated with improved postoperative cancerspecific survival in patients undergoing surgery for EC.
Figure
Reference
-
1. Henley SJ, Ward EM, Scott S, Ma J, Anderson RN, Firth AU, et al. Annual report to the nation on the status of cancer, part I: National cancer statistics. Cancer. 2020; 126(10):2225–2249. PMID: 32162336.2. Gu B, Shang X, Yan M, Li X, Wang W, Wang Q, et al. Variations in incidence and mortality rates of endometrial cancer at the global, regional, and national levels, 1990-2019. Gynecol Oncol. 2021; 161(2):573–580. PMID: 33551200.3. Morice P, Leary A, Creutzberg C, Abu-Rustum N, Darai E. Endometrial cancer. Lancet. 2016; 387(10023):1094–1108. PMID: 26354523.4. Koskas M, Amant F, Mirza MR, Creutzberg CL. Cancer of the corpus uteri: 2021 update. Int J Gynaecol Obstet. 2021; 155:Suppl 1. (Suppl 1):45–60. PMID: 34669196.5. Abu-Rustum NR, Zhou Q, Gomez JD, Alektiar KM, Hensley ML, Soslow RA, et al. A nomogram for predicting overall survival of women with endometrial cancer following primary therapy: toward improving individualized cancer care. Gynecol Oncol. 2010; 116(3):399–403. PMID: 20022094.6. Kolehmainen AM, Pasanen A, Tuomi T, Koivisto-Korander R, Butzow R, Loukovaara M. American Society of Anesthesiologists physical status score as a predictor of long-term outcome in women with endometrial cancer. Int J Gynecol Cancer. 2019; 29(5):ijgc-2018-000118.7. Driver JA, Viswanathan AN. Frailty measure is more predictive of outcomes after curative therapy for endometrial cancer than traditional risk factors in women 60 and older. Gynecol Oncol. 2017; 145(3):526–530. PMID: 28359689.8. Pinar Cilesiz Goksedef B, Gorgen H, Baran SY, Api M, Cetin A. Preoperative serum CA 125 level as a predictor for metastasis and survival in endometrioid endometrial cancer. J Obstet Gynaecol Can. 2011; 33(8):844–850. PMID: 21846440.9. Ekici H, Malatyalioglu E, Kokcu A, Kurtoglu E, Tosun M, Celik H. Do leukocyte and platelet counts have benefit for evaluation of endometrial cancer? Asian Pac J Cancer Prev. 2015; 16(13):5305–5310. PMID: 26225670.10. Reijnen C, Visser NC, Kasius JC, Boll D, Geomini PM, Ngo H, et al. Improved preoperative risk stratification with CA-125 in low-grade endometrial cancer: a multicenter prospective cohort study. J Gynecol Oncol. 2019; 30(5):e70. PMID: 31328454.11. Mohri Y, Inoue Y, Tanaka K, Hiro J, Uchida K, Kusunoki M. Prognostic nutritional index predicts postoperative outcome in colorectal cancer. World J Surg. 2013; 37(11):2688–2692. PMID: 23884382.12. Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nippon Geka Gakkai Zasshi. 1984; 85(9):1001–1005. PMID: 6438478.13. Komura N, Mabuchi S, Yokoi E, Shimura K, Kawano M, Matsumoto Y, et al. Prognostic significance of the pretreatment prognostic nutritional index in patients with epithelial ovarian cancer. Oncotarget. 2019; 10(38):3605–3613. PMID: 31217896.14. Zhang W, Ye B, Liang W, Ren Y. Preoperative prognostic nutritional index is a powerful predictor of prognosis in patients with stage III ovarian cancer. Sci Rep. 2017; 7(1):9548. PMID: 28842710.15. Haraga J, Nakamura K, Omichi C, Nishida T, Haruma T, Kusumoto T, et al. Pretreatment prognostic nutritional index is a significant predictor of prognosis in patients with cervical cancer treated with concurrent chemoradiotherapy. Mol Clin Oncol. 2016; 5(5):567–574. PMID: 27900086.16. Kiuchi K, Hasegawa K, Ochiai S, Motegi E, Kuno T, Kosaka N, et al. Prognostic significance of inflammatory parameters and nutritional index in clinical stage IVB endometrial carcinomas. J Obstet Gynaecol. 2019; 39(2):237–241. PMID: 30370797.17. Mirili C, Bilici M. Inflammatory prognostic markers in endometrial carcinoma: Systemic immune-inflammation index and prognostic nutritional index. Med Sci Discov. 2020; 7(1):351–359.18. Njoku K, Barr CE, Ramchander NC, Crosbie EJ. Impact of pre-treatment prognostic nutritional index and the haemoglobin, albumin, lymphocyte and platelet (HALP) score on endometrial cancer survival: a prospective database analysis. PLoS One. 2022; 17(8):e0272232. PMID: 35925991.19. Kim NR, So KA, Kim TJ, Lim K, Lee KH, Kim MK. Role of systematic lymphadenectomy in patients with intermediate to high-risk early stage endometrial cancer. J Gynecol Oncol. 2023; 34:e23. PMID: 36562131.20. Templeton AJ, McNamara MG, Šeruga B, Vera-Badillo FE, Aneja P, Ocaña A, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014; 106(6):dju124. PMID: 24875653.21. Hu B, Yang XR, Xu Y, Sun YF, Sun C, Guo W, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014; 20(23):6212–6222. PMID: 25271081.22. Desai RJ, Franklin JM. Alternative approaches for confounding adjustment in observational studies using weighting based on the propensity score: a primer for practitioners. BMJ. 2019; 367:l5657. PMID: 31645336.23. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021; 71(3):209–249. PMID: 33538338.24. Ha HI, Chang HK, Park SJ, Lim J, Won YJ, Lim MC. The incidence and survival of cervical, ovarian, and endometrial cancer in Korea, 1999-2017: Korea Central Cancer Registry. Obstet Gynecol Sci. 2021; 64(5):444–453. PMID: 34399564.25. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020; 70(1):7–30. PMID: 31912902.26. Aggarwal BB, Vijayalekshmi RV, Sung B. Targeting inflammatory pathways for prevention and therapy of cancer: short-term friend, long-term foe. Clin Cancer Res. 2009; 15(2):425–430. PMID: 19147746.27. Bambury RM, Teo MY, Power DG, Yusuf A, Murray S, Battley JE, et al. The association of pre-treatment neutrophil to lymphocyte ratio with overall survival in patients with glioblastoma multiforme. J Neurooncol. 2013; 114(1):149–154. PMID: 23780645.28. Sheehan KM, Sheahan K, O’Donoghue DP, MacSweeney F, Conroy RM, Fitzgerald DJ, et al. The relationship between cyclooxygenase-2 expression and colorectal cancer. JAMA. 1999; 282(13):1254–1257. PMID: 10517428.29. Coussens LM, Raymond WW, Bergers G, Laig-Webster M, Behrendtsen O, Werb Z, et al. Inflammatory mast cells up-regulate angiogenesis during squamous epithelial carcinogenesis. Genes Dev. 1999; 13(11):1382–1397. PMID: 10364156.30. Kusmartsev S, Gabrilovich DI. Immature myeloid cells and cancer-associated immune suppression. Cancer Immunol Immunother. 2002; 51(6):293–298. PMID: 12111117.31. Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A. Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis. 2009; 30(7):1073–1081. PMID: 19468060.32. Patel MV, Shen Z, Rodriguez-Garcia M, Usherwood EJ, Tafe LJ, Wira CR. Endometrial cancer suppresses CD8+ T cell-mediated cytotoxicity in postmenopausal women. Front Immunol. 2021; 12:657326. PMID: 33968059.33. Eckart A, Struja T, Kutz A, Baumgartner A, Baumgartner T, Zurfluh S, et al. Relationship of nutritional status, inflammation, and serum albumin levels during acute illness: a prospective study. Am J Med. 2020; 133(6):713–722.e7. PMID: 31751531.34. Jensen GL. Inflammation as the key interface of the medical and nutrition universes: a provocative examination of the future of clinical nutrition and medicine. JPEN J Parenter Enteral Nutr. 2006; 30(5):453–463. PMID: 16931617.35. Garcia-Martinez R, Caraceni P, Bernardi M, Gines P, Arroyo V, Jalan R. Albumin: pathophysiologic basis of its role in the treatment of cirrhosis and its complications. Hepatology. 2013; 58(5):1836–1846. PMID: 23423799.36. MacDonald N. . Cancer cachexia and targeting chronic inflammation: a unified approach to cancer treatment and palliative/supportive care. J Support Oncol. 2007; 5(4):157–162. PMID: 17500503.37. Yeun JY, Kaysen GA. Factors influencing serum albumin in dialysis patients. Am J Kidney Dis. 1998; 32(6):Suppl 4. S118–S125.38. Gelin J, Moldawer LL, Lönnroth C, Sherry B, Chizzonite R, Lundholm K. Role of endogenous tumor necrosis factor α and interleukin 1 for experimental tumor growth and the development of cancer cachexia. Cancer Res. 1991; 51(1):415–421. PMID: 1703040.39. Aoyama T, Takano M, Miyamoto M, Yoshikawa T, Kato K, Sakamoto T, et al. Pretreatment neutrophil-to-lymphocyte ratio was a predictor of lymph node metastasis in endometrial cancer patients. Oncology. 2019; 96(5):259–267. PMID: 30893700.40. Ni L, Tao J, Xu J, Yuan X, Long Y, Yu N, et al. Prognostic values of pretreatment neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in endometrial cancer: a systematic review and meta-analysis. Arch Gynecol Obstet. 2020; 301(1):251–261. PMID: 31768743.41. Dong Y, Cheng Y, Wang J. The ratio of neutrophil to lymphocyte is a predictor in endometrial cancer. Open Life Sci. 2019; 14(1):110–118. PMID: 33817142.42. Haruma T, Nakamura K, Nishida T, Ogawa C, Kusumoto T, Seki N, et al. Pre-treatment neutrophil to lymphocyte ratio is a predictor of prognosis in endometrial cancer. Anticancer Res. 2015; 35(1):337–343. PMID: 25550569.43. Matsubara S, Mabuchi S, Takeda Y, Kawahara N, Kobayashi H. Prognostic value of pre-treatment systemic immune-inflammation index in patients with endometrial cancer. PLoS One. 2021; 16(5):e0248871. PMID: 33989285.44. Son J, Carr C, Yao M, Radeva M, Priyadarshini A, Marquard J, et al. Endometrial cancer in young women: prognostic factors and treatment outcomes in women aged ≤40 years. Int J Gynecol Cancer. 2020; 30(5):631–639. PMID: 32213530.45. Persson I, Adami HO, Malker B, Pettersson B. Long-term survival in endometrial cancer with special reference to age as a prognostic factor. Ups J Med Sci. 1984; 89(2):159–170. PMID: 6464244.46. Chang SJ, Kim WY, Yoon JH, Yoo SC, Chang KH, Ryu HS. Para-aortic lymphadenectomy improves survival in patients with intermediate to high-risk endometrial carcinoma. Acta Obstet Gynecol Scand. 2008; 87(12):1361–1369. PMID: 18951214.47. Li L, Tang M, Nie D, Gou J, Li Z. Para-aortic lymphadenectomy did not improve overall survival among women with type I endometrial cancer. Int J Gynaecol Obstet. 2020; 150(2):163–168. PMID: 32433783.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Correction of Affiliations in the Article “Preoperative Prognostic Nutritional Index Is a Prognostic Indicator of Cancer-Specific Survival in Patients Undergoing Endometrial Cancer Surgery”
- Prognostic Significance of Preoperative Controlling Nutritional Status Score in Patients Who Underwent Hepatic Resection for Hepatocellular Carcinoma
- Clinical significance and prognostic value of C-reactive protein/albumin ratio in gastric cancer
- Multivariate survival analysis of the patients with recurrent endometrial cancer
- An Analysis of the Metabolic Syndrome and the Clinicopathologic Prognostic Factors Affecting Survival in Patients with Uterine Endometrial Cancer