Ann Hepatobiliary Pancreat Surg.
2023 May;27(2):151-157. 10.14701/ahbps.22-090.
Survival analysis of extrahepatic cholangiocarcinoma based on surveillance, epidemiology, and end results database
- Affiliations
-
- 1Department of Internal Medicine, East Carolina University, Greenville, NC, United States
- 2Department of Gastroenterology, Mather Hospital/Hofstra University School of Medicine, Port Jefferson, NY, United States
- 3Department of Internal Medicine, University of Health Sciences, Lahore, Punjab, Pakistan
- 4Department of Hepatology, Tampa General Hospital, Tampa, FL, United States
- KMID: 2542578
- DOI: http://doi.org/10.14701/ahbps.22-090
Abstract
- Backgrounds/Aims
Cholangiocarcinoma (CCA) can be classified as intrahepatic CCA or extrahepatic CCA (eCCA). We intended to analyze and reports the survival outcomes for eCCA.
Methods
Surveillance, epidemiology, and end results (SEER) registry, site recode C24.0, was used to select cases of eCCA from 2000 to 2018. Patients with incomplete data or ages <18 years were excluded.
Results
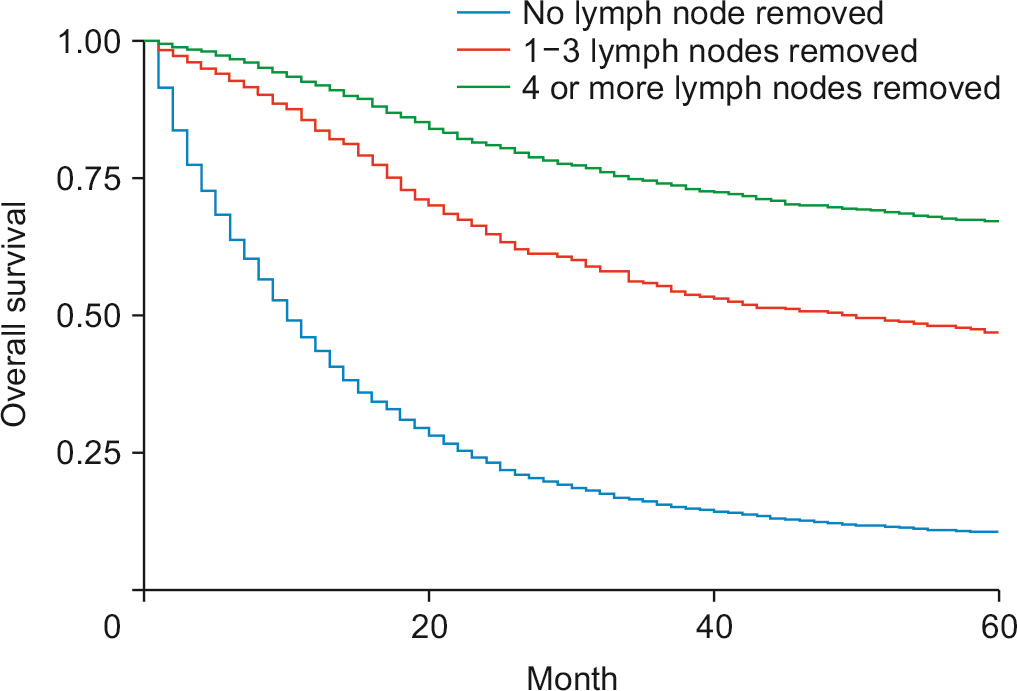
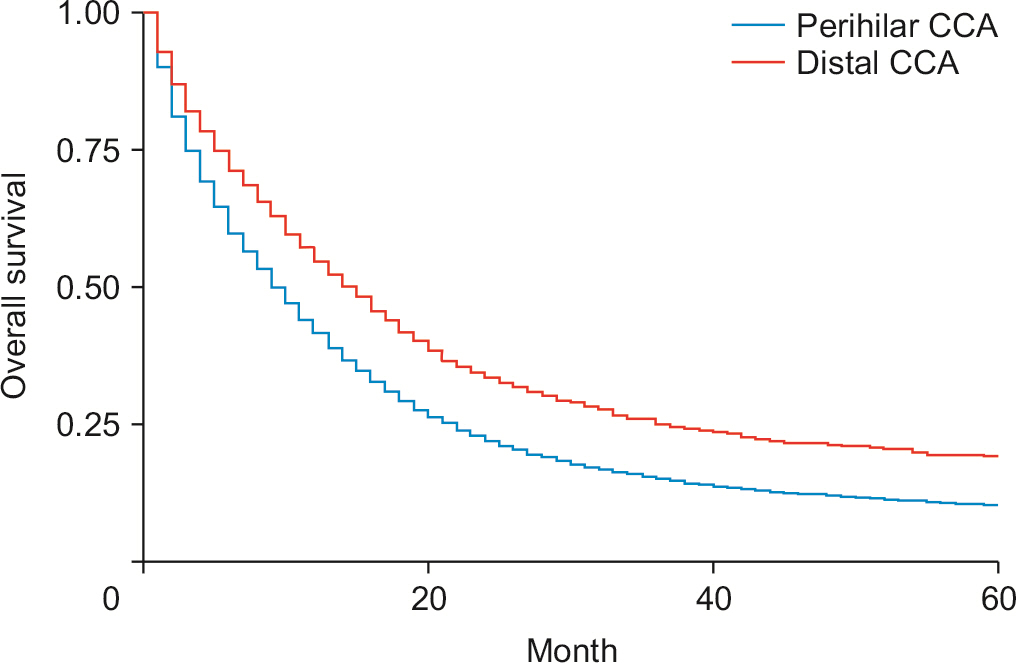
Male (52.69%) and White race (77.99%) predominated. Compared with 2000–2006, survival increased in 2013 (adjusted hazard ratio [HRadj]: 0.68, 95% confidence interval [CI] 0.58–0.70; p < 0.01). Surgery with chemoradiotherapy (HRadj: 0.69, 95% CI 0.60–0.7; p < 0.01) and surgery with chemotherapy (HRadj: 0.72, 95% CI 0.62–0.83; p < 0.01) improved survival over surgery alone. Compared with surgery without lymph node (LN) removal, surgery of four or more regional LN reduced the risk of death by 58% (HRadj: 0.42, 95% CI 0.36–0.51; p < 0.01). Compared with patients without surgery, patients who underwent bile duct excision (HRadj: 0.82, 95% CI 0.72–0.94; p < 0.01), simple or extended lobectomy (HRadj: 0.85, 95% CI 0.75–0.95; p = 0.009), and hepatectomy (HRadj: 0.80, 95% CI 0.72–0.88; p < 0.01) significantly improved survival. Patients with distal CCA had a 17% higher survival than perihilar CCA (HRadj: 0.83, 95% CI 0.74–0.92; p < 0.01) and LN dissection was equally beneficial for both subgroups (p < 0.01).
Conclusions
Surgery with chemoradiotherapy has a proven increase in the 5-year survival of the eCCA. LN resection, bile duct excision, lobectomy, and hepatectomy have better outcomes.
Keyword
Figure
Reference
-
1. Zhang H, Yang T, Wu M, Shen F. 2016; Intrahepatic cholangiocarcinoma: epidemiology, risk factors, diagnosis and surgical management. Cancer Lett. 379:198–205. DOI: 10.1016/j.canlet.2015.09.008. PMID: 26409434.
Article2. Ali H, Tedder B, Waqar SH, Mohamed R, Cate EL, Ali E. 2022; Changing incidence and survival of intrahepatic cholangiocarcinoma based on Surveillance, Epidemiology, and End Results Database (2000-2017). Ann Hepatobiliary Pancreat Surg. 26:235–243. DOI: 10.14701/ahbps.21-173. PMID: 35811455. PMCID: PMC9428430.
Article3. Blechacz B, Komuta M, Roskams T, Gores GJ. 2011; Clinical diagnosis and staging of cholangiocarcinoma. Nat Rev Gastroenterol Hepatol. 8:512–522. DOI: 10.1038/nrgastro.2011.131. PMID: 21808282. PMCID: PMC3331791.
Article4. Liao P, Cao L, Chen H, Pang SZ. 2021; Analysis of metastasis and survival between extrahepatic and intrahepatic cholangiocarcinoma: a large population-based study. Medicine (Baltimore). 100:e25635. DOI: 10.1097/MD.0000000000025635. PMID: 33879742. PMCID: PMC8078350.5. Marcano-Bonilla L, Mohamed EA, Mounajjed T, Roberts LR. 2016; Biliary tract cancers: epidemiology, molecular pathogenesis and genetic risk associations. Chin Clin Oncol. 5:61. DOI: 10.21037/cco.2016.10.09. PMID: 27829275.
Article6. Forner A, Vidili G, Rengo M, Bujanda L, Ponz-Sarvisé M, Lamarca A. 2019; Clinical presentation, diagnosis and staging of cholangiocarcinoma. Liver Int. 39 Suppl 1:98–107. DOI: 10.1111/liv.14086. PMID: 30831002.
Article7. Welzel TM, McGlynn KA, Hsing AW, O'Brien TR, Pfeiffer RM. 2006; Impact of classification of hilar cholangiocarcinomas (Klatskin tumors) on the incidence of intra- and extrahepatic cholangiocarcinoma in the United States. J Natl Cancer Inst. 98:873–875. DOI: 10.1093/jnci/djj234. PMID: 16788161.
Article8. Surveillance Research Program, NCIs Division of Cancer Control and Population Sciences. SEER Registries [Internet]. Washington, D.C.: National Cancer Institute;2021. cited 2021 Sep 29. Available from: https://seer.cancer.gov/.9. Surveillance Research Program, National Cancer Institute. SEER*Stat software version 8.3.9.2 [Internet]. Washington, D.C.: National Cancer Institute;2021. cited 2021 Sep 29. Available from: https://seer.cancer.gov/seerstat/.10. Brar G, Greten TF, Graubard BI, McNeel TS, Petrick JL, McGlynn KA, et al. 2020; Hepatocellular carcinoma survival by etiology: a SEER-medicare database analysis. Hepatol Commun. 4:1541–1551. DOI: 10.1002/hep4.1564. PMID: 33024922. PMCID: PMC7527688.
Article11. Ali H, Pamarthy R, Vallabhaneni M, Sarfraz S, Ali H, Rafique H. Pancreatic cancer incidence trends in the United States from 2000-2017: analysis of Surveillance, Epidemiology and End Results (SEER) database. F1000Res. 2021; 10:529. DOI: 10.12688/f1000research.54390.1. PMID: 34527218. PMCID: PMC8411275.
Article12. Mao K, Liu J, Sun J, Zhang J, Chen J, Pawlik TM, et al. 2016; Patterns and prognostic value of lymph node dissection for resected perihilar cholangiocarcinoma. J Gastroenterol Hepatol. 31:417–426. DOI: 10.1111/jgh.13072. PMID: 26250532. PMCID: PMC4732906.
Article13. Zhang Y, Wu Z, Wang X, Li C, Chang J, Jiang W, et al. 2020; Development and external validation of a nomogram for predicting the effect of tumor size on survival of patients with perihilar cholangiocarcinoma. BMC Cancer. 20:1044. DOI: 10.1186/s12885-020-07501-0. PMID: 33126868. PMCID: PMC7596930.
Article14. Liu WW, Tu JF, Ying XH, Chen ZJ, Wang YB. 2022; Postoperative survival of extrahepatic and intrahepatic cholangiocarcinoma after surgery: a population-based cohort. BMJ Open. 12:e049789. DOI: 10.1136/bmjopen-2021-049789. PMID: 35414539. PMCID: PMC9006842.
Article15. Clements O, Eliahoo J, Kim JU, Taylor-Robinson SD, Khan SA. 2020; Risk factors for intrahepatic and extrahepatic cholangiocarcinoma: a systematic review and meta-analysis. J Hepatol. 72:95–103. DOI: 10.1016/j.jhep.2019.09.007. PMID: 31536748.
Article16. Tyson GL, El-Serag HB. 2011; Risk factors for cholangiocarcinoma. Hepatology. 54:173–184. DOI: 10.1002/hep.24351. PMID: 21488076. PMCID: PMC3125451.
Article17. Shaib Y, El-Serag HB. 2004; The epidemiology of cholangiocarcinoma. Semin Liver Dis. 24:115–125. DOI: 10.1055/s-2004-828889. PMID: 15192785.
Article18. ipa B Sr, Pairojkul C. 2008; Cholangiocarcinoma: lessons from Thailand. Curr Opin Gastroenterol. 24:349–356. DOI: 10.1097/MOG.0b013e3282fbf9b3. PMID: 18408464. PMCID: PMC4130346.
Article19. Lim JH. 2011; Liver flukes: the malady neglected. Korean J Radiol. 12:269–279. DOI: 10.3348/kjr.2011.12.3.269. PMID: 21603286. PMCID: PMC3088844.
Article20. Gad MM, Saad AM, Faisaluddin M, Gaman MA, Ruhban IA, Jazieh KA, et al. 2020; Epidemiology of cholangiocarcinoma; United States incidence and mortality trends. Clin Res Hepatol Gastroenterol. 44:885–893. DOI: 10.1016/j.clinre.2020.03.024. PMID: 32359831.
Article21. Molodecky NA, Kareemi H, Parab R, Barkema HW, Quan H, Myers RP, et al. 2011; Incidence of primary sclerosing cholangitis: a systematic review and meta-analysis. Hepatology. 53:1590–1599. DOI: 10.1002/hep.24247. PMID: 21351115.
Article22. Bird NTE, McKenna A, Dodd J, Poston G, Jones R, Malik H. 2018; Meta-analysis of prognostic factors for overall survival in patients with resected hilar cholangiocarcinoma. Br J Surg. 105:1408–1416. DOI: 10.1002/bjs.10921. PMID: 29999515.
Article23. Jang JY, Kim SW, Park DJ, Ahn YJ, Yoon YS, Choi MG, et al. 2005; Actual long-term outcome of extrahepatic bile duct cancer after surgical resection. Ann Surg. 241:77–84. DOI: 10.1097/01.sla.0000150166.94732.88. PMID: 15621994. PMCID: PMC1356849.
Article24. Hoehn RS, Wima K, Ertel AE, Meier A, Ahmad SA, Shah SA, et al. 2015; Adjuvant chemotherapy and radiation therapy is associated with improved survival for patients with extrahepatic cholangiocarcinoma. Ann Surg Oncol. 22 Suppl 3:S1133–S1139. DOI: 10.1245/s10434-015-4599-8. PMID: 25976862.
Article25. Ren F, Zhang J, Gao Z, Zhu H, Chen X, Liu W, et al. 2018; Racial disparities in the survival time of patients with hepatocellular carcinoma and intrahepatic cholangiocarcinoma between Chinese patients and patients of other racial groups: a population-based study from 2004 to 2013. Oncol Lett. 16:7102–7116. DOI: 10.3892/ol.2018.9550. PMID: 30546445. PMCID: PMC6256729.
Article26. Wang F, Liu Y, Zhang H. 2013; Loss of MTSS1 expression is an independent prognostic factor for Hilar cholangiocarcinoma. Pathol Oncol Res. 19:815–820. DOI: 10.1007/s12253-013-9649-6. PMID: 23852458.
Article27. Stewart SL, Kwong SL, Bowlus CL, Nguyen TT, Maxwell AE, Bastani R, et al. Racial/ethnic disparities in hepatocellular carcinoma treatment and survival in California, 1988-2012. World J Gastroenterol. 2016; 22:8584–8595. DOI: 10.3748/wjg.v22.i38.8584. PMID: 27784971. PMCID: PMC5064040.
Article28. Barr Fritcher EG, Voss JS, Brankley SM, Campion MB, Jenkins SM, Keeney ME, et al. 2015; An optimized set of fluorescence in situ hybridization probes for detection of pancreatobiliary tract cancer in cytology brush samples. Gastroenterology. 149:1813–1824.e1. DOI: 10.1053/j.gastro.2015.08.046. PMID: 26327129.
Article29. Ebata T, Mizuno T, Yokoyama Y, Igami T, Sugawara G, Nagino M. 2018; Surgical resection for Bismuth type IV perihilar cholangiocarcinoma. Br J Surg. 105:829–838. DOI: 10.1002/bjs.10556. PMID: 28488733.
Article30. Valle J, Wasan H, Palmer DH, Cunningham D, Anthoney A, Maraveyas A, et al. 2010; Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N Engl J Med. 362:1273–1281. DOI: 10.1056/NEJMoa0908721. PMID: 20375404.
Article31. Primrose JN, Fox RP, Palmer DH, Malik HZ, Prasad R, Mirza D, et al. 2019; Capecitabine compared with observation in resected biliary tract cancer (BILCAP): a randomised, controlled, multicentre, phase 3 study. Lancet Oncol. 20:663–673. Erratum in: Lancet Oncol 2019;20:e242.
Article32. Darwish Murad S, Heimbach JK, Gores GJ, Rosen CB, Benson JT, Kim WR. 2013; Excellent quality of life after liver transplantation for patients with perihilar cholangiocarcinoma who have undergone neoadjuvant chemoradiation. Liver Transpl. 19:521–528. DOI: 10.1002/lt.23630. PMID: 23447435.
Article33. Buettner S, Galjart B, van Vugt JLA, Bagante F, Alexandrescu S, Marques HP, et al. 2017; Performance of prognostic scores and staging systems in predicting long-term survival outcomes after surgery for intrahepatic cholangiocarcinoma. J Surg Oncol. 116:1085–1095. DOI: 10.1002/jso.24759. PMID: 28703880.
Article34. Liu ZP, Zhang QY, Chen WY, Huang YY, Zhang YQ, Gong Y, et al. 2022; Evaluation of four lymph node classifications for the prediction of survival in hilar cholangiocarcinoma. J Gastrointest Surg. 26:1030–1040. DOI: 10.1007/s11605-021-05211-x. PMID: 34973138. PMCID: PMC9085675.
Article35. Kim HJ, Kim CY, Hur YH, Koh YS, Kim JC, Kim HJ, et al. 2014; Prognostic factors for survival after curative resection of distal cholangiocarcinoma: perineural invasion and lymphovascular invasion. Surg Today. 44:1879–1886. DOI: 10.1007/s00595-014-0846-z. PMID: 24535697.
Article36. Waseem D, Tushar P. 2017; Intrahepatic, perihilar and distal cholangiocarcinoma: management and outcomes. Ann Hepatol. 16:133–139. DOI: 10.5604/16652681.1226927. PMID: 28051802. PMCID: PMC5630455.
Article37. Valero V 3rd, Cosgrove D, Herman JM, Pawlik TM. 2012; Management of perihilar cholangiocarcinoma in the era of multimodal therapy. Expert Rev Gastroenterol Hepatol. 6:481–495. DOI: 10.1586/egh.12.20. PMID: 22928900. PMCID: PMC3538366.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changing incidence and survival of intrahepatic cholangiocarcinoma based on Surveillance, Epidemiology, and End Results Database (2000–2017)
- The epidemiology and risk factors of hilar cholangiocarcinoma
- Incidence, mortality, and survival of liver cancer using Korea central cancer registry database: 1999–2019
- Comparison of the clinical results of surgical resection for extrahepatic cholangiocarcinomas: Hilar cholangiocarcinoma and mid-to-distal cholangiocarcinoma
- Descriptive Epidemiology of Cholangiocarcinoma and Clonorchiasis in Korea