Ann Hepatobiliary Pancreat Surg.
2022 Aug;26(3):211-219. 10.14701/ahbps.22-044.
Incidence, mortality, and survival of liver cancer using Korea central cancer registry database: 1999–2019
- Affiliations
-
- 1Department of Liver Transplantation and Hepatobiliary Surgery, Ajou University School of Medicine, Suwon, Korea
- 2Division of Cancer Registration and Surveillance, National Cancer Center, Goyang, Korea
- KMID: 2532636
- DOI: http://doi.org/10.14701/ahbps.22-044
Abstract
- Backgrounds/Aims
Historically, incidence and survival analysis and annual traits for primary liver cancer (LC) has not been investigated in a population-based study in Korea. The purpose of the current study is to determine incidence, survival rate of patients with primary LC in Korea.
Methods
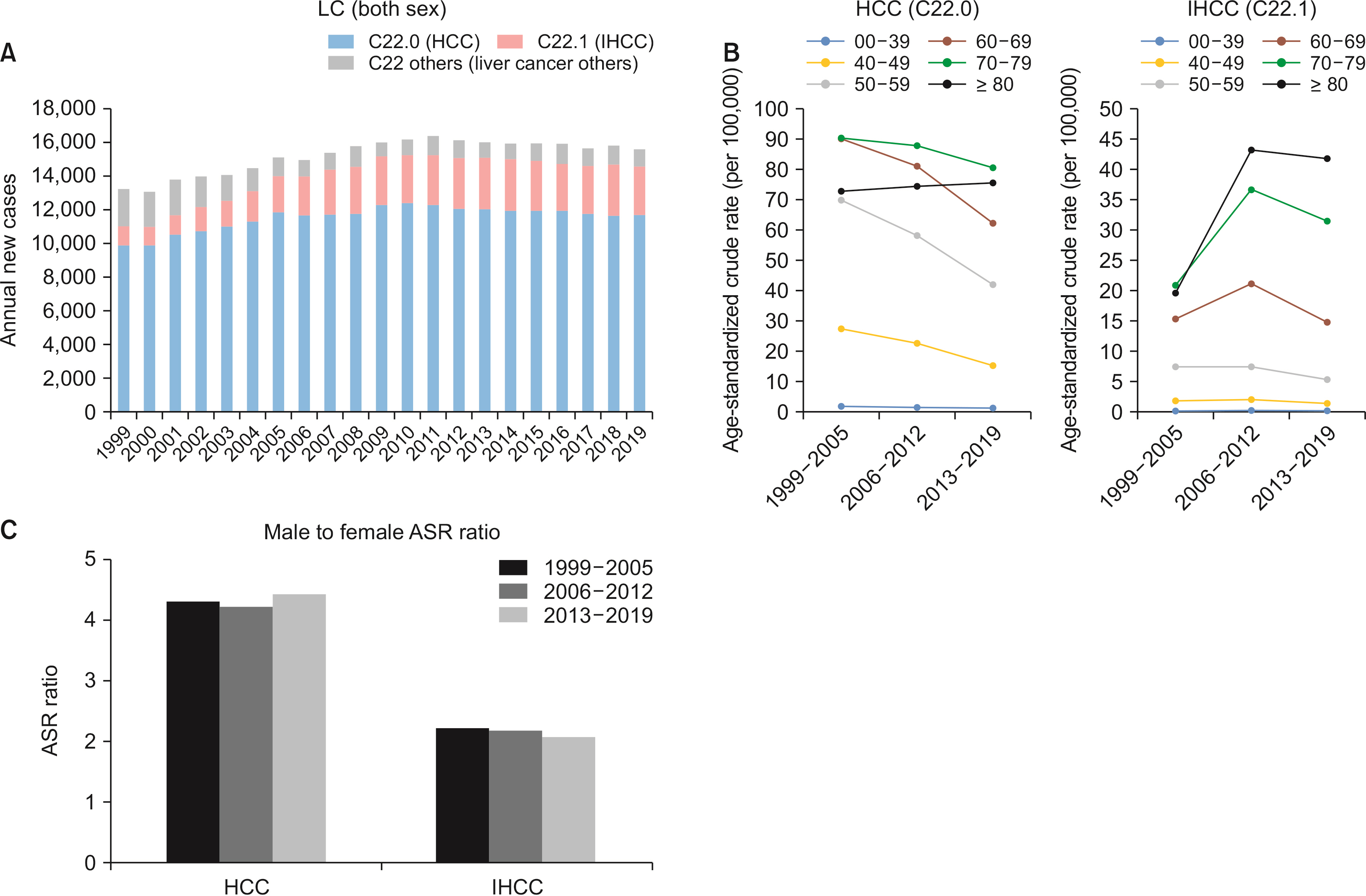
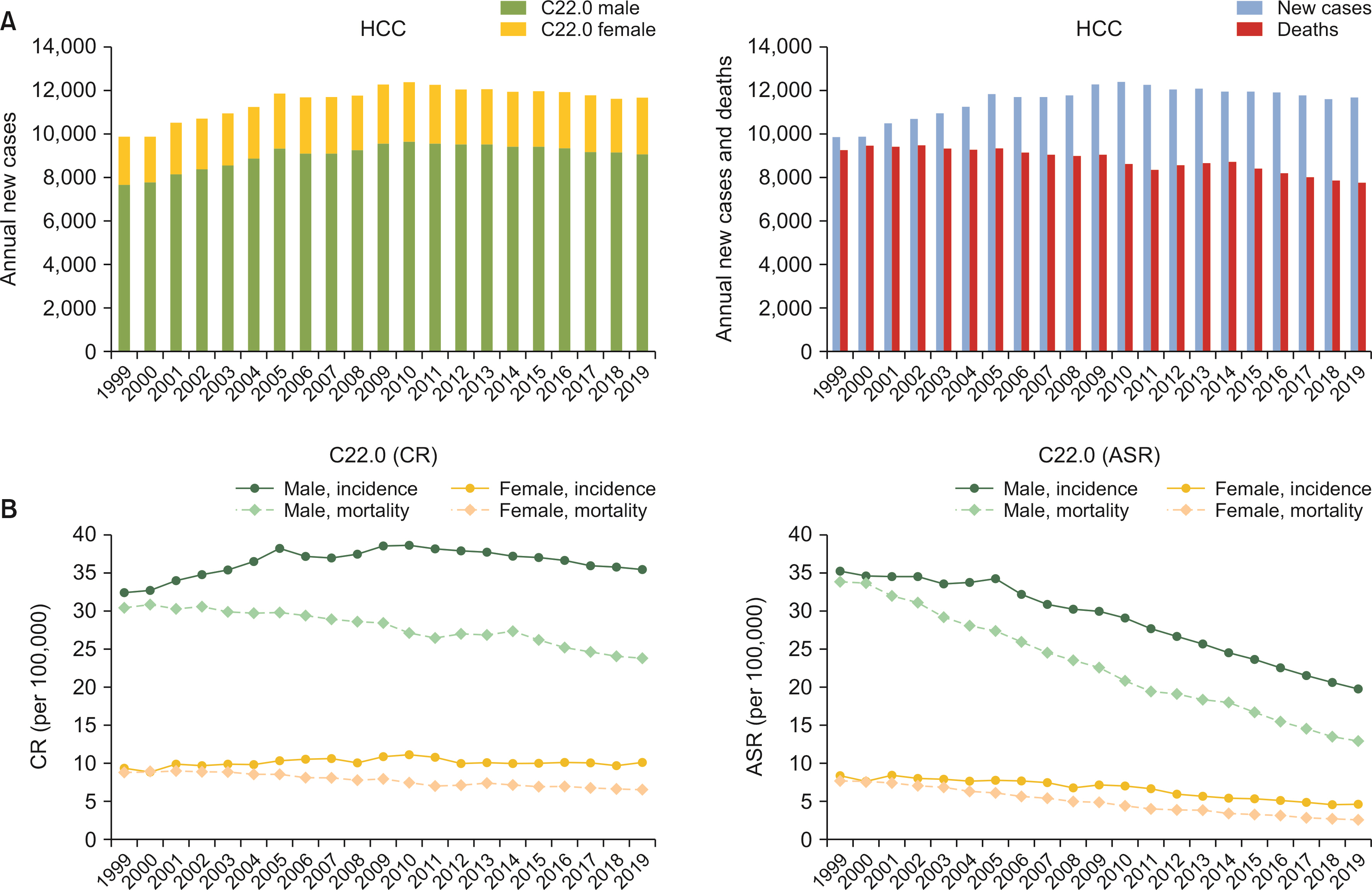
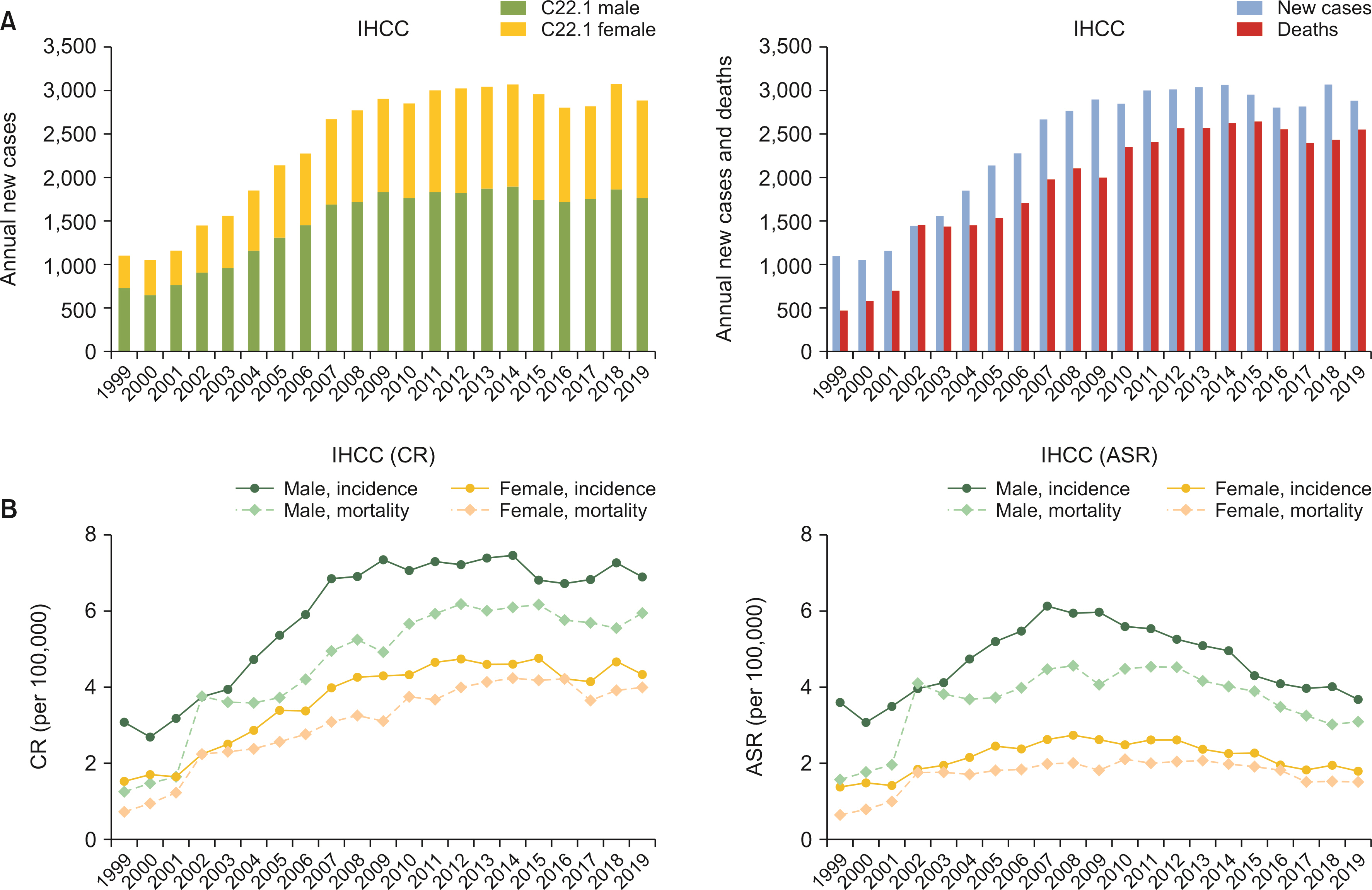
We conducted a retrospective cohort study using Korea Central Cancer Registry based on the Korea National Cancer Incidence Database. Statistical analysis including crude rate and age-standadized rate (ASR) of incidence and mortality was performed for LC patients registered with C22 code in International Classification of Diseases, tenth revision from 1999 to 2019. Subgroup analysis was performed for hepatocellular carcinoma (HCC, C22.0) and intrahepatic cholangiocarcinoma (IHCC, C22.1).
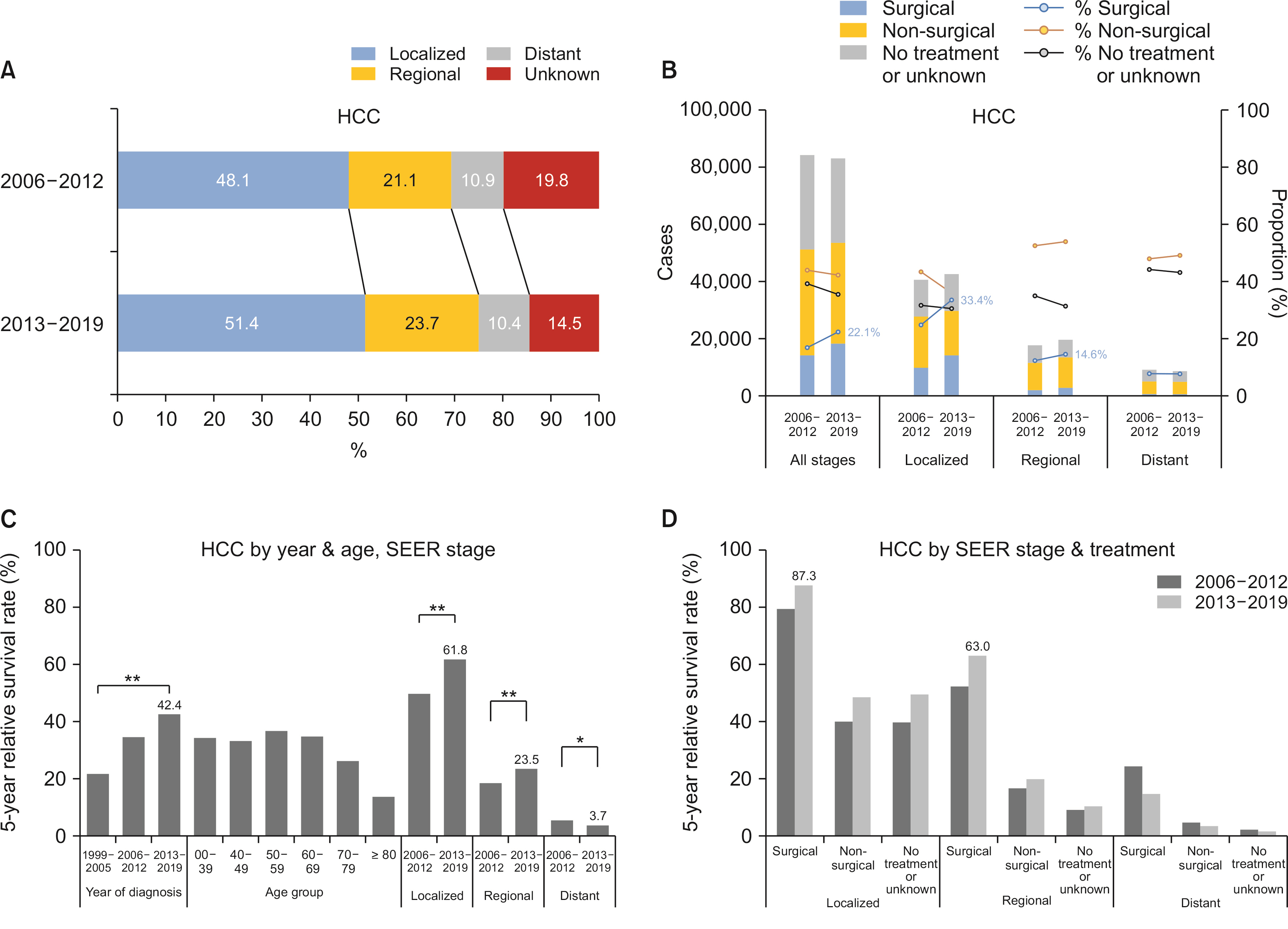
Results
The crude incidence rate of HCC (21.0 to 22.8 per 100,000) and IHCC (2.3 to 5.6 per 100,000) increased in the observed period from 1999 to 2019. The ASR decreased in HCC (20.7 to 11.9 per 100,000) but remained unchanged in IHCC (2.4 to 2.7 per 100,000). The proportion of HCC patients diagnosed in early stages (localized or regional Surveillance, Epidemiology, and End Results or SEER stage) increased significantly over time. As expected, 5-yeat survival rate of HCC was greatly improved, reaching 42.4% in the period between 2013 and 2019. This trait was more prominent in localized SEER stage. On the other hand, the proportion of IHCC patients diagnosed in localized stage remained unchanged (22.9% between 2013 and 2019), although ASR and 5-year survival rate showed minor improvements.
Conclusions
A great improvement in survival rate was observed in patients with newly diagnosed HCCs. It was estimated to be due to an increase in early detection rate. On the contrary, detection rate of an early IHCC was stagnant with a minor improvement in prognosis.
Figure
Cited by 1 articles
-
Incidence, mortality and survival of gallbladder, extrahepatic bile duct, and pancreatic cancer using Korea central cancer registry database: 1999-2019
Mee Joo Kang, E Hwa Yun, Kyu-Won Jung, Sang-Jae Park
Int J Stem Cells. 2022;26(3):220-228. doi: 10.14701/ahbps.22-041.
Reference
-
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424. Erratum in: CA Cancer J Clin 2020;70:313. DOI: 10.3322/caac.21492. PMID: 30207593.2. Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. 2015; Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 136:E359–E386. DOI: 10.1002/ijc.29210. PMID: 25220842.3. Sia D, Villanueva A, Friedman SL, Llovet JM. 2017; Liver cancer cell of origin, molecular class, and effects on patient prognosis. Gastroenterology. 152:745–761. DOI: 10.1053/j.gastro.2016.11.048. PMID: 28043904.4. Kim BH, Park JW. 2018; Epidemiology of liver cancer in South Korea. Clin Mol Hepatol. 24:1–9. DOI: 10.3350/cmh.2017.0112. PMID: 29249129. PMCID: PMC5875192.5. Choi SI, Cho Y, Ki M, Kim BH, Lee IJ, Kim TH, et al. 2022; Better survival of patients with hepatitis B virus-related hepatocellular carcinoma in South Korea: changes in 16-years cohorts. PLoS One. 17:e0265668. DOI: 10.1371/journal.pone.0265668. PMID: 35324973. PMCID: PMC8947113.6. Kim BH, Lee D, Jung KW, Won YJ, Cho H. 2022; Cause of death and cause-specific mortality for primary liver cancer in South Korea: a nationwide population-based study in hepatitis B virus-endemic area. Clin Mol Hepatol. 28:242–253. DOI: 10.3350/cmh.2021.0355. PMID: 35130416. PMCID: PMC9013615.7. Kang MJ, Won YJ, Lee JJ, Jung KW, Kim HJ, Kong HJ, et al. 2022; Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2019. Cancer Res Treat. 54:330–344. DOI: 10.4143/crt.2022.128. PMID: 35313102. PMCID: PMC9016309.8. Yang MS, Park M, Back JH, Lee GH, Shin JH, Kim K, et al. 2022; Validation of cancer diagnosis based on the national health insurance service database versus the National Cancer Registry Database in Korea. Cancer Res Treat. 54:352–361. DOI: 10.4143/crt.2021.044. PMID: 34353000. PMCID: PMC9016317.9. Tanaka K, Ogura Y. 2004; "Small-for-size graft" and "small-for-size syndrome" in living donor liver transplantation. Yonsei Med J. 45:1089–1094. DOI: 10.3349/ymj.2004.45.6.1089. PMID: 15627301.10. Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, et al. 2011; Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 149:713–724. DOI: 10.1016/j.surg.2010.10.001. PMID: 21236455.11. Kang MJ, Lim J, Han SS, Park HM, Park SJ, Won YJ, et al. 2022; First course of treatment and prognosis of exocrine pancreatic cancer in Korea from 2006 to 2017. Cancer Res Treat. 54:208–217. DOI: 10.4143/crt.2021.421. PMID: 34030432. PMCID: PMC8756130.12. Strong RW. 2006; Living-donor liver transplantation: an overview. J Hepatobiliary Pancreat Surg. 13:370–377. DOI: 10.1007/s00534-005-1076-y. PMID: 17013709.13. Inomata Y, Uemoto S, Asonuma K, Egawa H. 2000; Right lobe graft in living donor liver transplantation. Transplantation. 69:258–264. DOI: 10.1097/00007890-200001270-00011. PMID: 10670636.14. Wong MC, Jiang JY, Goggins WB, Liang M, Fang Y, Fung FD, et al. 2017; International incidence and mortality trends of liver cancer: a global profile. Sci Rep. 7:45846. DOI: 10.1038/srep45846. PMID: 28361988. PMCID: PMC5374459.15. Yang S, Khang YH, Harper S, Davey Smith G, Leon DA, Lynch J. 2010; Understanding the rapid increase in life expectancy in South Korea. Am J Public Health. 100:896–903. DOI: 10.2105/AJPH.2009.160341. PMID: 20299661. PMCID: PMC2853609.16. Shin HR, Won YJ, Jung KW, Kong HJ, Yim SH, Lee JK, et al. 2005; Nationwide cancer incidence in Korea, 1999~2001; first result using the national cancer incidence database. Cancer Res Treat. 37:325–331. DOI: 10.4143/crt.2005.37.6.325. PMID: 19956367. PMCID: PMC2785938.17. Kang MJ, Lim J, Han SS, Park HM, Kim SW, Won YJ, et al. 2021; Impact of changes in the topographic classification of Klatskin tumor on incidence of intra- and extrahepatic bile duct cancer: a population-based national cancer registry study. J Hepatobiliary Pancreat Sci. 28:740–750. DOI: 10.1002/jhbp.916. PMID: 33615747.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2016
- Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2019
- Epidemiology of Gastric Cancer in Korea: Trends in Incidence and Survival Based on Korea Central Cancer Registry Data (1999–2019)
- Prediction of Cancer Incidence and Mortality in Korea, 2019
- Trend Analysis and Prediction of Hepatobiliary Pancreatic Cancer Incidence and Mortality in Korea