Ann Hepatobiliary Pancreat Surg.
2019 Nov;23(4):319-326. 10.14701/ahbps.2019.23.4.319.
Comparison of the clinical results of surgical resection for extrahepatic cholangiocarcinomas: Hilar cholangiocarcinoma and mid-to-distal cholangiocarcinoma
- Affiliations
-
- 1Department of Surgery, Korean Cancer Center Hospital, Seoul, Korea. gsceh@kirams.re.kr
- 2Department of Surgery, Dongnam Institution of Radiological and Medical Science, Busan, Korea.
- KMID: 2464319
- DOI: http://doi.org/10.14701/ahbps.2019.23.4.319
Abstract
- BACKGROUNDS/AIMS
Hilar cholangiocarcinomas (HLC) are known to have worse prognoses than mid-to-distal cholangiocarcinomas (CBDC). We analyzed the clinical results of surgical resections for extrahepatic cholangiocarcinomas to validate the differences in the prognoses of HLC and CBDC.
METHODS
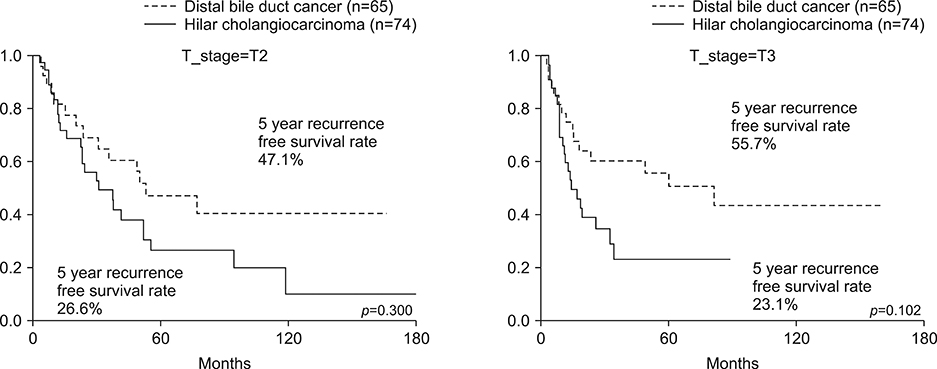
Two hundred and eighty-one patients underwent curative surgical resections for extrahepatic cholangiocarcinomas at the Department of Surgery in the Korea Cancer Center Hospital. Among them, we analyzed the T2 and T3 patients and compared the clinical results between those with HLC (n=74) and those with CBDC (n=65).
RESULTS
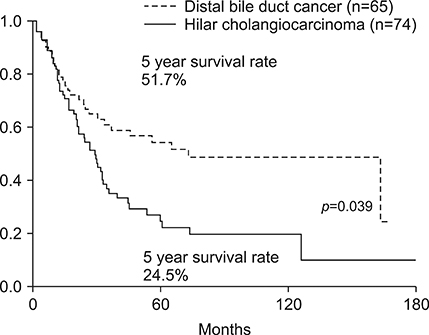
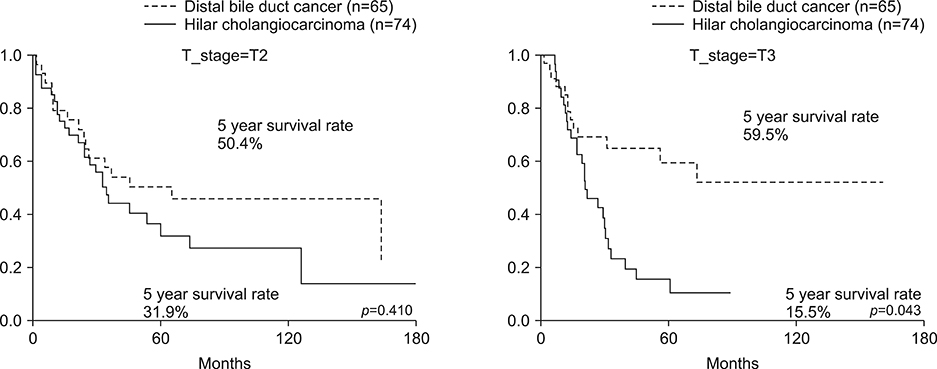
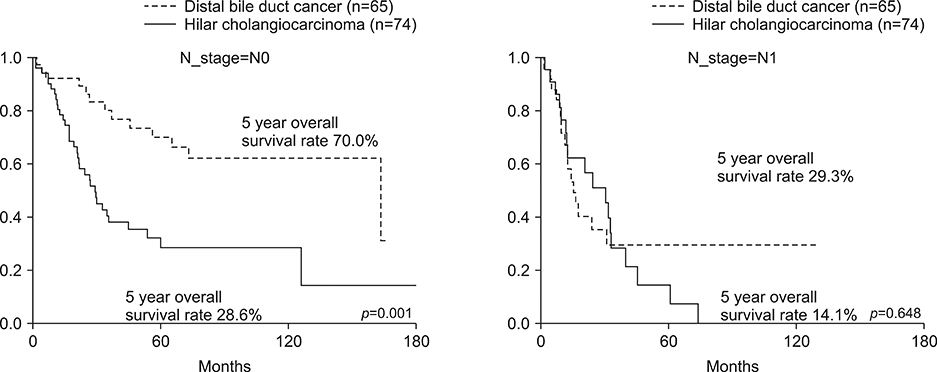
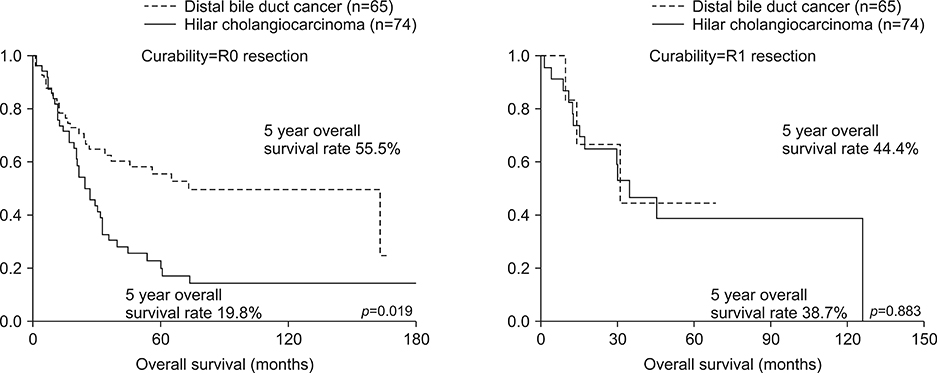
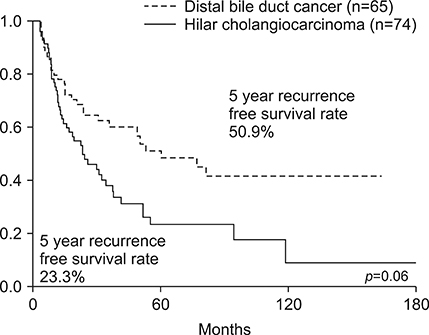
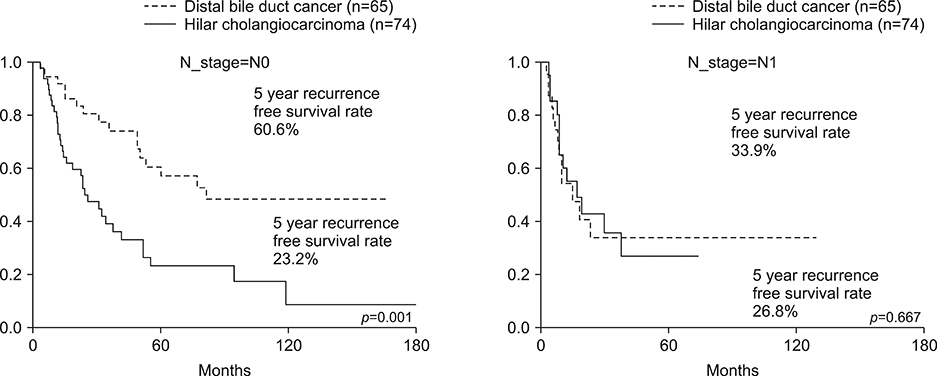
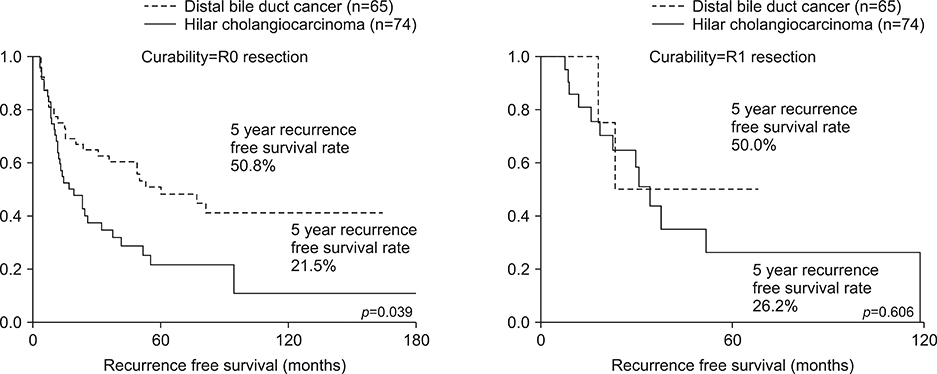
The rate of R1 resections was significantly higher in the HLC patients compared to the CBDC patients (31.1% vs 12.3%, p=0.006). The overall survival rate of the T2/T3 patients was lower in the HLC group than in the CBDC group (24.5% vs 51.7, p=0.039). The recurrence-free survival rate was 23.3% in the HCL patients and 50.9% in the CBDC patients (p=0.06). In the subgroup analysis, the survival rates were not different in patients who had lymph node metastases or in patients who underwent R1 resections between the HLC and CBDC patients. Poor independent prognostic factors for the overall and recurrence-free survival rates in the T2/T3 extrahepatic cholangiocarcinoma patients were the presence of lymph node metastases and the hilar locations of tumor.
CONCLUSIONS
HLC patients had poorer prognoses than CBDC patients. However, in patients with lymph node metastases, the prognosis was poor and was not different between the HLC and CBDC patients. Other adjuvant treatment methods are needed for extrahepatic cholangiocarcinoma patients with lymph node metastases to improve their prognoses.
MeSH Terms
Figure
Reference
-
1. Vauthey JN, Blumgart LH. Recent advances in the management of cholangiocarcinomas. Semin Liver Dis. 1994; 14:109–114.2. Kang HJ, Kwon SJ, Kwon TW, Kim GS, Kim NG, Kim DW, et al. Liver, GB, biliary, pancreas, spleen. Korean Surg Soc. Surgery. 2nd ed. Seoul: Gunja;2017. p. 760.3. Jung KW, Won YJ, Kong HJ, Lee ES. Community of Population-Based Regional Cancer Registries. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2015. Cancer Res Treat. 2018; 50:303–316.4. Lee HG, Lee SH, Yoo DD, Paik KY, Heo JS, Choi SH, et al. Carcinoma of the middle bile duct: is bile duct segmental resection appropriate? World J Gastroenterol. 2009; 15:5966–5971.5. Kloek JJ, Ten Kate FJ, Busch OR, Gouma DJ, van Gulik TM. Surgery for extrahepatic cholangiocarcinoma: predictors of survival. HPB (Oxford). 2008; 10:190–195.6. Marcano-Bonilla L, Mohamed EA, Mounajjed T, Roberts LR. Biliary tract cancers: epidemiology, molecular pathogenesis and genetic risk associations. Chin Clin Oncol. 2016; 5:61.7. Park JY, Kim HH, Park EK, Seoung JS, Hur YH, Koh YS, et al. Histopathologic prognostic factors for recurrence and survival after surgical resection of middle and distal bile duct cancer. Korean J Hepatobiliary Pancreat Surg. 2010; 14:165–172.8. Cidon EU. Resectable cholangiocarcinoma: reviewing the role of adjuvant strategies. Clin Med Insights Oncol. 2016; 10:43–48.9. Vern-Gross TZ, Shivnani AT, Chen K, Lee CM, Tward JD, MacDonald OK, et al. Survival outcomes in resected extrahepatic cholangiocarcinoma: effect of adjuvant radiotherapy in a surveillance, epidemiology, and end results analysis. Int J Radiat Oncol Biol Phys. 2011; 81:189–198.10. Wakai T, Shirai Y, Moroda T, Yokoyama N, Hatakeyama K. Impact of ductal resection margin status on long-term survival in patients undergoing resection for extrahepatic cholangiocarcinoma. Cancer. 2005; 103:1210–1216.11. Kim JW, Jo S, Moon HJ, Heo JS, Choi SH, Joh JW, et al. Prognostic factors after major resection for distal extrahepatic cholangiocarcinoma. Korean J Gastroenterol. 2006; 47:144–152.12. Lee J, Koh DH. Molecular pathogenesis and the role of tumor markers in cholangiocarcinoma. Korean J Med. 2010; 79:597–604.13. Ryu JK. The epidemiology and risk factors of hilar cholangiocarcinoma. Korean J Med. 2010; 79:593–596.14. Patel T. Cholangiocarcinoma--controversies and challenges. Nat Rev Gastroenterol Hepatol. 2011; 8:189–200.15. Eun JR, Jang BI, Lee JY, Kim KO, Lee SH, Kim TN, et al. Clinical characteristics of intrahepatic cholangiocarcinoma and prognostic factors in patients who received non-surgical treatment. Korean J Gastroenterol. 2009; 54:227–234.16. Mao ZY, Guo XC, Su D, Wang LJ, Zhang TT, Bai L. Prognostic factors of cholangiocarcinoma after surgical resection: a retrospective study of 293 patients. Med Sci Monit. 2015; 21:2375–2381.17. Howell M, Valle JW. The role of adjuvant chemotherapy and radiotherapy for cholangiocarcinoma. Best Pract Res Clin Gastroenterol. 2015; 29:333–343.18. Ramírez-Merino N, Aix SP, Cortés-Funes H. Chemotherapy for cholangiocarcinoma: an update. World J Gastrointest Oncol. 2013; 5:171–176.19. Gabriel E, Gandhi S, Attwood K, Kuvshinoff B, Hochwald S, Iyer R. Gemcitabine and capecitabine for advanced biliary cancer. J Gastrointest Oncol. 2017; 8:728–736.20. Moureau-Zabotto L, Turrini O, Resbeut M, Raoul JL, Giovannini M, Poizat F, et al. Impact of radiotherapy in the management of locally advanced extrahepatic cholangiocarcinoma. BMC Cancer. 2013; 13:568.21. Blom D, Schwartz SI. Surgical treatment and outcomes in carcinoma of the extrahepatic bile ducts: the University of Rochester experience. Arch Surg. 2001; 136:209–215.22. Reding R, Buard JL, Lebeau G, Launois B. Surgical management of 552 carcinomas of the extrahepatic bile ducts (gallbladder and periampullary tumors excluded). Results of the French surgical association survey. Ann Surg. 1991; 213:236–241.23. Park SW, Park YS, Chung JB, Kang JK, Kim KS, Choi JS, et al. Patterns and relevant factors of tumor recurrence for extrahepatic bile duct carcinoma after radical resection. Hepatogastroenterology. 2004; 51:1612–1618.24. Kim HJ, Bang S, Park SW, Song SY, Kim KS, Lee WJ, et al. Assessment of the definition of early extrahepatic bile duct cancer through the prognosis analysis who had received curative resection. Korean J Gastroenterol. 2007; 50:101–107.25. Baek JO, Kim YH, Kang GJ, IM TJ. Comparison of survival rates according to tumor location and surgical method in patients with extrahepatic bile duct cancer treated with curative resection. Paper presented at: 32st Korean hepatobiliarypancreas surgery symposium. 2010 Mar 26–27; Seoul, Korea. p. 133.26. Choi SB, Park SW, Kim KS, Choi JS, Lee WJ. The survival outcome and prognostic factors for middle and distal bile duct cancer following surgical resection. J Surg Oncol. 2009; 99:335–342.27. Yoshida T, Matsumoto T, Sasaki A, Morii Y, Aramaki M, Kitano S. Prognostic factors after pancreatoduodenectomy with extended lymphadenectomy for distal bile duct cancer. Arch Surg. 2002; 137:69–73.28. Kitagawa Y, Nagino M, Kamiya J, Uesaka K, Sano T, Yamamoto H, et al. Lymph node metastasis from hilar cholangiocarcinoma: audit of 110 patients who underwent regional and paraaortic node dissection. Ann Surg. 2001; 233:385–392.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiological Staging of Hilar Cholangiocarcinoma
- Preoperative Diagnosis and Management for Hilar Cholangiocarcinoma
- The epidemiology and risk factors of hilar cholangiocarcinoma
- Current Status and Recent Update of Imaging Evaluation for Peri-Hilar Cholangiocarcinoma
- Current Updates in the Surgical Management of Hilar Cholangiocarcinoma