J Stroke.
2023 May;25(2):233-241. 10.5853/jos.2022.03489.
Thrombus Enhancement Sign for Differentiation of Embolism and Arteriosclerosis-Related Acute Large Vessel Occlusion
- Affiliations
-
- 1Department of Radiology, Shanghai Sixth People’s Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 2Department of Neurology, The First People’s Hospital of Kunshan, Kunshan, China
- 3Department of Radiology, The First People’s Hospital of Kunshan, Kunshan, China
- 4Department of Neurology, Shanghai Sixth People’s Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, Shanghai, China
- KMID: 2542474
- DOI: http://doi.org/10.5853/jos.2022.03489
Abstract
- Background and Purpose
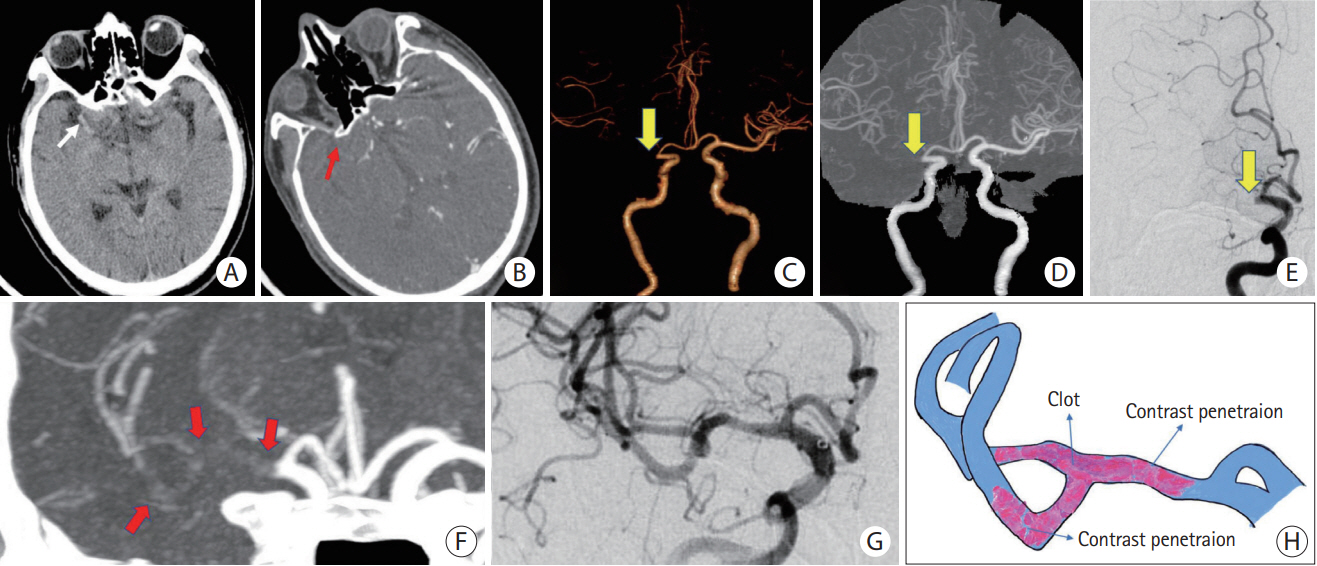
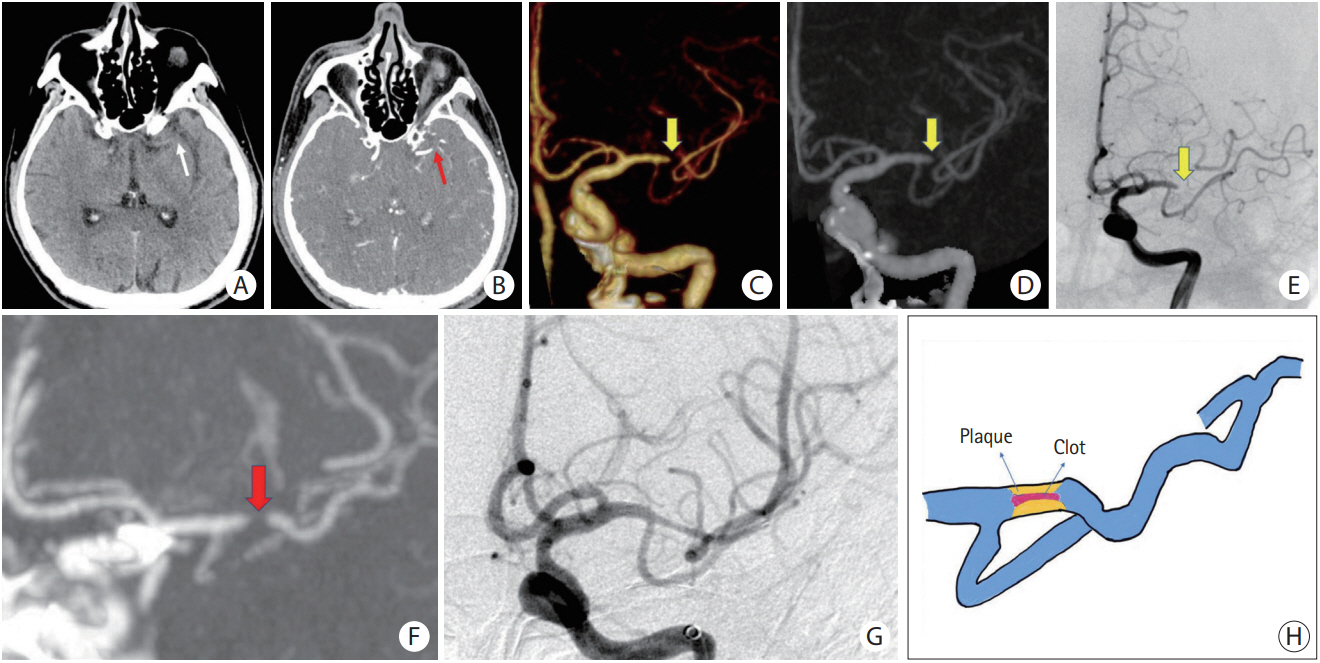
To evaluate whether the thrombus enhancement sign (TES) can be used to differentiate embolic large vessel occlusion (LVO) from in situ intracranial atherosclerotic stenosis (ICAS)-related LVO in the anterior circulation of patients with acute ischemic stroke (AIS).
Methods
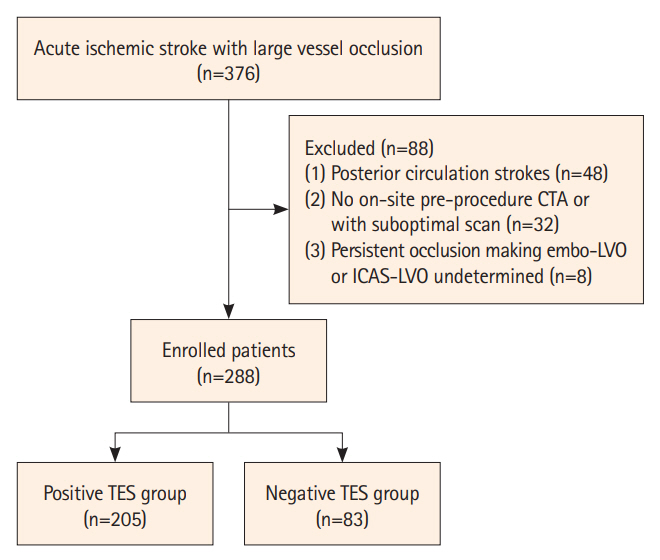
Patients with LVO in the anterior circulation who underwent both non-contrast computed tomography (CT) and CT angiography and mechanical thrombectomy were retrospectively enrolled. Both embolic LVO (embo-LVO) and in situ ICAS-related LVO (ICAS-LVO) were confirmed by two neurointerventional radiologists after reviewing the medical and imaging data. TES was assessed to predict embo-LVO or ICAS-LVO. The associations between occlusion type and TES, along with clinical and interventional parameters, were investigated using logistic regression analysis and a receiver operating characteristic curve.
Results
A total of 288 patients with AIS were included and divided into an embo-LVO group (n=235) and an ICAS-LVO group (n=53). TES was identified in 205 (71.2%) patients and was more frequently observed in those with embo-LVO, with a sensitivity of 83.8%, specificity of 84.9%, and area under the curve (AUC) of 0.844. Multivariate analysis showed that TES (odds ratio [OR], 22.2; 95% confidence interval [CI], 9.4–53.8; P<0.001) and atrial fibrillation (OR, 6.6; 95% CI, 2.8–15.8; P<0.001) were independent predictors of embolic occlusion. A predictive model that included both TES and atrial fibrillation yielded a higher diagnostic ability for embo-LVO, with an AUC of 0.899.
Conclusion
TES is an imaging marker with high predictive value for identifying embo- and ICAS-LVO in AIS and provides guidance for endovascular reperfusion therapy.
Keyword
Figure
Reference
-
References
1. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–1731.
Article2. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018; 378:11–21.3. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.
Article4. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50:e344–e418.
Article5. Gutierrez J, Turan TN, Hoh BL, Chimowitz MI. Intracranial atherosclerotic stenosis: risk factors, diagnosis, and treatment. Lancet Neurol. 2022; 21:355–368.
Article6. Holmstedt CA, Turan TN, Chimowitz MI. Atherosclerotic intracranial arterial stenosis: risk factors, diagnosis, and treatment. Lancet Neurol. 2013; 12:1106–1114.
Article7. Tsang ACO, Orru E, Klostranec JM, Yang IH, Lau KK, Tsang FCP, et al. Thrombectomy outcomes of intracranial atherosclerosis-related occlusions. Stroke. 2019; 50:1460–1466.
Article8. Jia B, Feng L, Liebeskind DS, Huo X, Gao F, Ma N, et al. Mechanical thrombectomy and rescue therapy for intracranial large artery occlusion with underlying atherosclerosis. J Neurointerv Surg. 2018; 10:746–750.
Article9. Vilela P, Rowley HA. Brain ischemia: CT and MRI techniques in acute ischemic stroke. Eur J Radiol. 2017; 96:162–172.
Article10. Kufner A, Erdur H, Endres M, Nolte CH, Scheel M, Schlemm L. Association between thrombus perviousness assessed on computed tomography and stroke cause. Stroke. 2020; 51:3613–3622.
Article11. Berndt M, Friedrich B, Maegerlein C, Moench S, Hedderich D, Lehm M, et al. Thrombus permeability in admission computed tomographic imaging indicates stroke pathogenesis based on thrombus histology. Stroke. 2018; 49:2674–2682.
Article12. Wei L, Zhu Y, Deng J, Li Y, Li M, Lu H, et al. Visualization of thrombus enhancement on thin-slab maximum intensity projection of CT angiography: an imaging sign for predicting stroke source and thrombus compositions. Radiology. 2021; 298:374–381.
Article13. He G, Deng J, Lu H, Wei L, Zhao Y, Zhu Y, et al. Thrombus enhancement sign on CT angiography is associated with the first pass effect of stent retrievers. J Neurointerv Surg. 2023; 15:146–152.
Article14. Humphries W, Hoit D, Doss VT, Elijovich L, Frei D, Loy D, et al. Distal aspiration with retrievable stent assisted thrombectomy for the treatment of acute ischemic stroke. J Neurointerv Surg. 2015; 7:90–94.
Article15. Puetz V, Dzialowski I, Hill MD, Subramaniam S, Sylaja PN, Krol A, et al. Intracranial thrombus extent predicts clinical outcome, final infarct size and hemorrhagic transformation in ischemic stroke: the clot burden score. Int J Stroke. 2008; 3:230–236.
Article16. Zaidat OO, Yoo AJ, Khatri P, Tomsick TA, von Kummer R, Saver JL, et al. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke. 2013; 44:2650–2663.
Article17. Lee JS, Hong JM, Kim JS. Diagnostic and therapeutic strategies for acute intracranial atherosclerosis-related occlusions. J Stroke. 2017; 19:143–151.
Article18. Tomasello A, Ribò M, Gramegna LL, Melendez F, Rosati S, Moreu M, et al. Procedural approaches and angiographic signs predicting first-pass recanalization in patients treated with mechanical thrombectomy for acute ischaemic stroke. Interv Neuroradiol. 2019; 25:491–496.
Article19. Lee JS, Hong JM, Lee KS, Suh HI, Choi JW, Kim SY. Primary stent retrieval for acute intracranial large artery occlusion due to atherosclerotic disease. J Stroke. 2016; 18:96–101.
Article20. Yoo J, Lee SJ, Hong JH, Kim YW, Hong JM, Kim CH, et al. Immediate effects of first-line thrombectomy devices for intracranial atherosclerosis-related occlusion: stent retriever versus contact aspiration. BMC Neurol. 2020; 20:283.
Article21. Suh HI, Hong JM, Lee KS, Han M, Choi JW, Kim JS, et al. Imaging predictors for atherosclerosis-related intracranial large artery occlusions in acute anterior circulation stroke. J Stroke. 2016; 18:352–354.
Article22. Kim YW, Hong JM, Park DG, Choi JW, Kang DH, Kim YS, et al. Effect of intracranial atherosclerotic disease on endovascular treatment for patients with acute vertebrobasilar occlusion. AJNR Am J Neuroradiol. 2016; 37:2072–2078.
Article23. Cho KH, Kim JS, Kwon SU, Cho AH, Kang DW. Significance of susceptibility vessel sign on T2*-weighted gradient echo imaging for identification of stroke subtypes. Stroke. 2005; 36:2379–2383.
Article24. Liebeskind DS, Sanossian N, Yong WH, Starkman S, Tsang MP, Moya AL, et al. CT and MRI early vessel signs reflect clot composition in acute stroke. Stroke. 2011; 42:1237–1243.
Article25. Kim SK, Yoon W, Heo TW, Park MS, Kang HK. Negative susceptibility vessel sign and underlying intracranial atherosclerotic stenosis in acute middle cerebral artery occlusion. AJNR Am J Neuroradiol. 2015; 36:1266–1271.
Article26. Baik SH, Kim JW, Kim BM, Kim DJ. Significance of angiographic clot meniscus sign in mechanical thrombectomy of basilar artery stroke. J Neurointerv Surg. 2020; 12:477–482.
Article27. Baek JH, Kim BM, Yoo J, Nam HS, Kim YD, Kim DJ, et al. Predictive value of computed tomography angiography-determined occlusion type in stent retriever thrombectomy. Stroke. 2017; 48:2746–2752.
Article28. Chen WH, Yi TY, Zhan AL, Wu YM, Lu YY, Li YM, et al. Stent-unsheathed effect predicts acute distal middle cerebral artery atherosclerotic disease-related occlusion. J Neurol Sci. 2020; 416:116957.
Article29. Kim JW, Lee BH. Usefulness of stent strut deformity during thrombectomy for predicting the stroke etiology in acute large artery occlusion. Clin Neurol Neurosurg. 2020; 198:106130.
Article30. Yi TY, Chen WH, Wu YM, Zhang MF, Zhan AL, Chen YH, et al. Microcatheter “first-pass effect” predicts acute intracranial artery atherosclerotic disease-related occlusion. Neurosurgery. 2019; 84:1296–1305.
Article31. Al Kasab S, Almallouhi E, Spiotta AM. Rescue endovascular treatment for emergent large vessel occlusion with underlying intracranial atherosclerosis: current state and future directions. Front Neurol. 2021; 12:734971.
Article32. Menon BK, Al-Ajlan FS, Najm M, Puig J, Castellanos M, Dowlatshahi D, et al. Association of clinical, imaging, and thrombus characteristics with recanalization of visible intracranial occlusion in patients with acute ischemic stroke. JAMA. 2018; 320:1017–1026.
Article33. Mishra SM, Dykeman J, Sajobi TT, Trivedi A, Almekhlafi M, Sohn SI, et al. Early reperfusion rates with IV tPA are determined by CTA clot characteristics. AJNR Am J Neuroradiol. 2014; 35:2265–2272.
Article34. Lee JS, Hong JM, Lee KS, Suh HI, Demchuk AM, Hwang YH, et al. Endovascular therapy of cerebral arterial occlusions: intracranial atherosclerosis versus embolism. J Stroke Cerebrovasc Dis. 2015; 24:2074–2080.
Article35. Hwang YH, Kim YW, Kang DH, Kim YS, Liebeskind DS. Impact of target arterial residual stenosis on outcome after endovascular revascularization. Stroke. 2016; 47:1850–1857.
Article36. Pistoia F, Sacco S, Tiseo C, Degan D, Ornello R, Carolei A. The epidemiology of atrial fibrillation and stroke. Cardiol Clin. 2016; 34:255–268.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A fluttering worm-like thrombus-in-transit in the right atrium: A sign of disastrous embolism
- Primary stent retrieval for acute intracranial large artery occlusion due to atherosclerotic disease
- Traditional Thrombus Composition and Related Endovascular Outcomes: Catching up with the Recent Evidence
- Mechanical Thrombectomy for Septic Embolism Secondary to Staphylococcus lugdunensis Bacteremia without Infective Endocarditis: A Case Report
- Endovascular Treatment of Large Vessel Occlusion Strokes Due to Intracranial Atherosclerotic Disease