Neurointervention.
2022 Nov;17(3):190-194. 10.5469/neuroint.2022.00318.
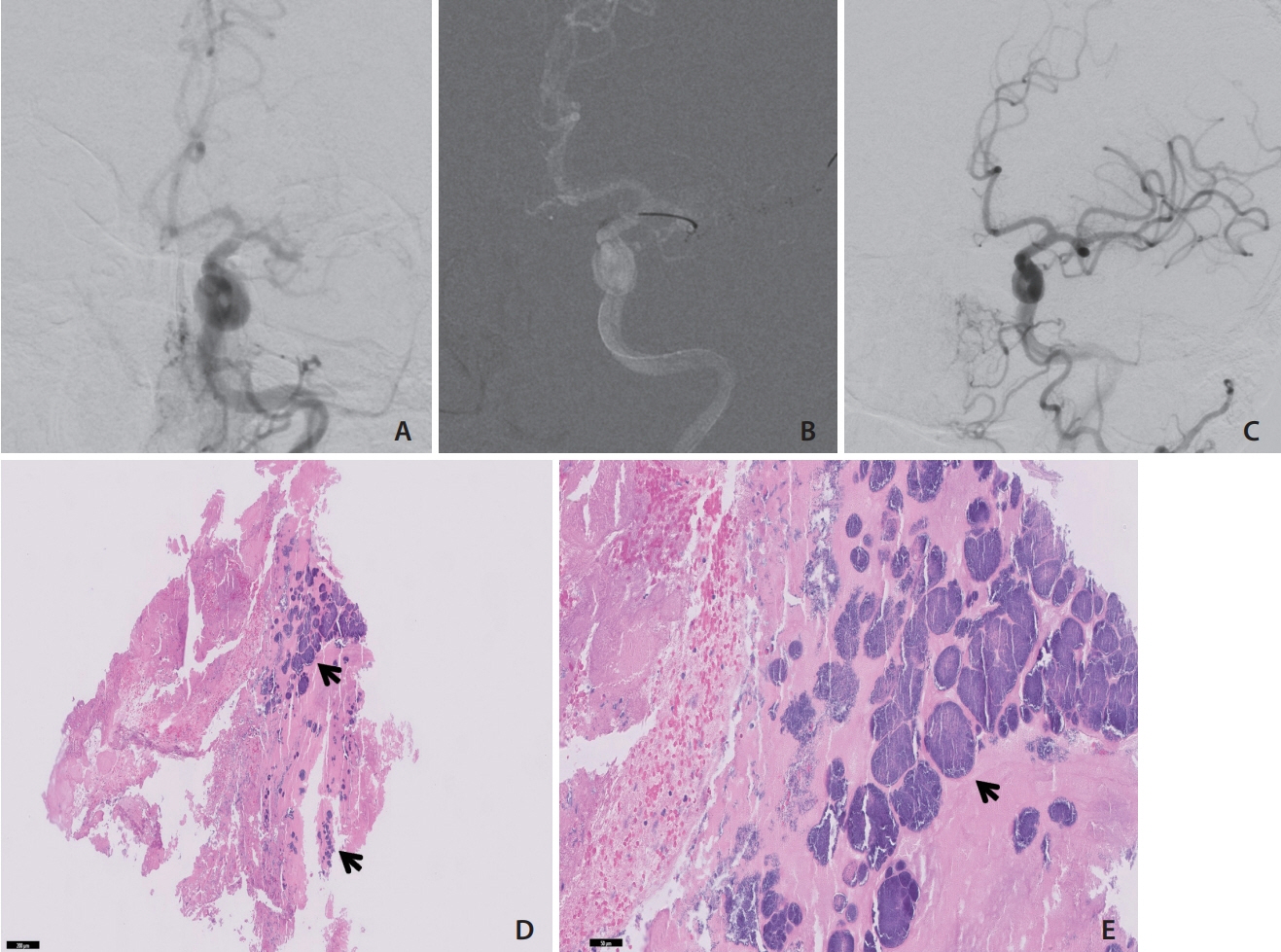
Mechanical Thrombectomy for Septic Embolism Secondary to Staphylococcus lugdunensis Bacteremia without Infective Endocarditis: A Case Report
- Affiliations
-
- 1Department of Neurosurgery, Baylor Scott & White Health, Scott and White Medical Center, Temple, TX, USA
- 2Department of Surgery, Texas A&M University College of Medicine, Temple, TX, USA
- KMID: 2535955
- DOI: http://doi.org/10.5469/neuroint.2022.00318
Abstract
- A cerebral large vessel occlusion due to septic embolism with resultant stroke is a known complication of infective endocarditis and can cause severe neurologic disability. However, septic embolism rarely occurs in the absence of infective endocarditis, and emboli due to different organisms may behave differently. As such, it is important to recognize the different pathogens that can cause septic embolism resulting in cerebral large vessel occlusion and to have data on successful treatments. We describe here a case of mechanical thrombectomy for septic embolism secondary to Staphylococcus lugdunensis bacteremia without infective endocarditis.
Keyword
Figure
Reference
-
1. Bettencourt S, Ferro JM. Acute ischemic stroke treatment in infective endocarditis: systematic review. J Stroke Cerebrovasc Dis. 2020; 29:104598.
Article2. Al-Mufti F, Schirmer CM, Starke RM, Chaudhary N, De Leacy R, Tjoumakaris SI, SNIS Standards and Guidelines Committee and SNIS Board of Directors, et al. Thrombectomy in special populations: report of the Society of NeuroInterventional Surgery Standards and Guidelines Committee. [published online ahead of print Jul 8, 2021]. J Neurointerv Surg. 2021.
Article3. Sonneville R, Mourvillier B, Bouadma L, Wolff M. Management of neurological complications of infective endocarditis in ICU patients. Ann Intensive Care. 2011; 1:10.
Article4. Kyaw H, Raju F, Shaikh AZ, Lin AN, Lin AT, Abboud J, et al. Staphylococcus lugdunensis endocarditis and cerebrovascular accident: a systemic review of risk factors and clinical outcome. Cureus. 2018; 10:e2469.
Article5. Elsaghir H, Al Khalili Y. Septic emboli. In : Abai B, Abu-Ghosh A, Acharya AB, Acharya U, Adhia SG, Sedeh PA, editors. StatPearls. Treasure Island (FL): StatPearls Publishing;2022.6. Stawicki SP, Firstenberg MS, Lyaker MR, Russell SB, Evans DC, Bergese SD, et al. Septic embolism in the intensive care unit. Int J Crit Illn Inj Sci. 2013; 3:58–63.
Article7. Bain MD, Hussain MS, Gonugunta V, Katzan I, Gupta R. Successful recanalization of a septic embolus with a balloon mounted stent after failed mechanical thrombectomy. J Neuroimaging. 2011; 21:170–172.
Article8. Hernández-Fernández F, Rojas-Bartolomé L, García-García J, Ayo-Martín Ó, Molina-Nuevo JD, Barbella-Aponte RA, et al. Histopathological and bacteriological analysis of thrombus material extracted during mechanical thrombectomy in acute stroke patients. Cardiovasc Intervent Radiol. 2017; 40:1851–1860.
Article9. Sabe MA, Shrestha NK, Gordon S, Menon V. Staphylococcus lugdunensis: a rare but destructive cause of coagulase-negative staphylococcus infective endocarditis. Eur Heart J Acute Cardiovasc Care. 2014; 3:275–280.
Article10. Ishidou M, Kanno K, Murata M, Hirose K, Ikai A, Sakamoto K. Fatal septic embolism due to Staphylococcus lugdunensis-induced bacteremia. Gen Thorac Cardiovasc Surg. 2021; 69:993–995.
Article11. Shah K, Jobanputra Y, Sharma P. Recurrent bacteremia in the setting of a coronary artery fistula. Cureus. 2020; 12:e9289.
Article12. Marnat G, Sibon I, Gory B, Richard S, Olindo S, Consoli A, ETIS Registry Investigators, et al. Safety and outcomes of mechanical thrombectomy for acute stroke related to infective endocarditis: a case-control study. Int J Stroke. 2021; 16:585–592. Erratum in: Int J Stroke 2021;16:NP3.
Article13. Feil K, Küpper C, Tiedt S, Dimitriadis K, Herzberg M, Dorn F, GSR Investigators, et al. Safety and efficacy of mechanical thrombectomy in infective endocarditis: a matched case-control analysis from the German stroke registry-endovascular treatment. Eur J Neurol. 2021; 28:861–867.
Article14. Holland TL, Baddour LM, Bayer AS, Hoen B, Miro JM, Fowler VG Jr. Infective endocarditis. Nat Rev Dis Primers. 2016; 2:16059.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Infective Endocarditis due to Staphylococcus lugdunensis
- A Case of Native Valve Infective Endocarditis Caused by Staphylococcus lugdunensis
- A Case of Pulmonary Artery Endarteritis due to Staphylococcus lugdunensis in Patient with Clinically Silent Patent Ductus Arteriosus
- A Case of Psoas Abscess Caused by Staphylococcus lugdunensis
- Septic Knee Arthritis Caused by Staphylococcus lugdunensis After Intraarticular Injection Therapy