Obstet Gynecol Sci.
2023 May;66(3):230-240. 10.5468/ogs.22171.
A novel radiofrequency modulation therapy versus routine physiotherapy modalities in treatment of myofascial pelvic pain syndrome: a pilot randomized trial
- Affiliations
-
- 1Emam Khomeini Hospital Pelvic Floor Clinic, Tehran University of Medical Sciences, Tehran, Iran
- 2Yas University Hospital, Tehran University of Medical Sciences, Tehran, Iran
- 3Medical school, Tehran University of Medical Sciences, Tehran, Iran
- 4Department of Obstetrics and Gynecology, Yas University Hospital, Tehran University of Medical Science, Tehran, Iran
- 5Health Metrics Research Center, Iranian Institute for Health Sciences Research, ACECR, Tehran, Iran
- 6Non-Communicable Diseases Research Center, Imam Ali Hospital, Alborz University of Medical Sciences, Karaj, Iran
- 7Clinical Research Development Unit, Imam Ali Hospital, Alborz University of Medical Sciences, Karaj, Iran
- KMID: 2542229
- DOI: http://doi.org/10.5468/ogs.22171
Abstract
Objective
The current study aimed to compare the effectiveness of novel radiofrequency modulation (RM) therapy with a tailored physiotherapy course for patients with chronic pelvic pain (CPP) of myofascial origin, also known as myofascial pelvic pain syndrome (MPPS).
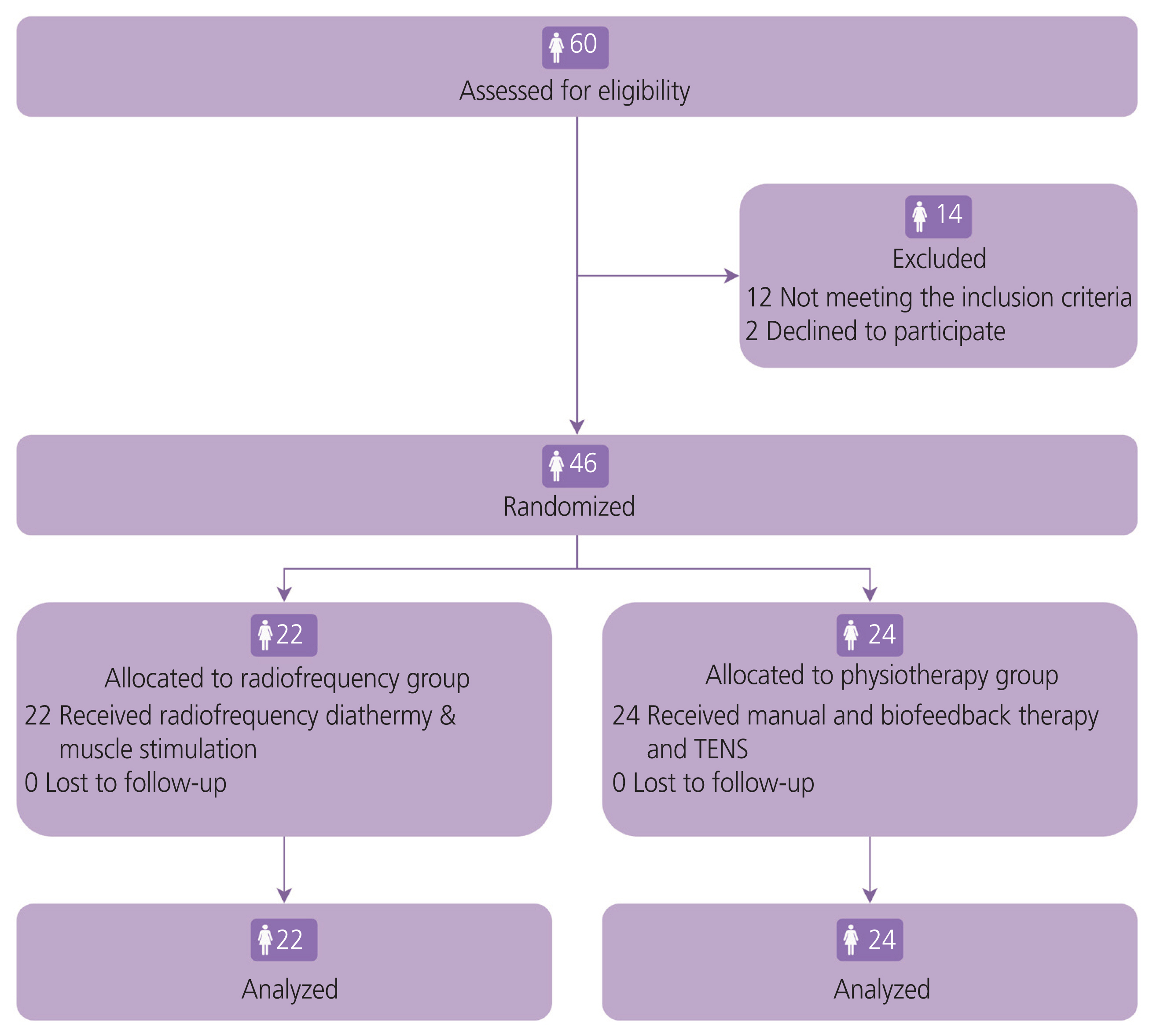
Methods
We enrolled 46 patients with myofascial CPP to compare the effectiveness of a 10-session routine physiotherapy course versus a 6-session RM with an integrated device (HIGGS) in alleviating MPPS morbidity and pelvic floor muscle (PFM) rehabilitation. The primary outcome was reduction in pelvic pain after the final session and in the follow-up period 3 months after the final intervention session.
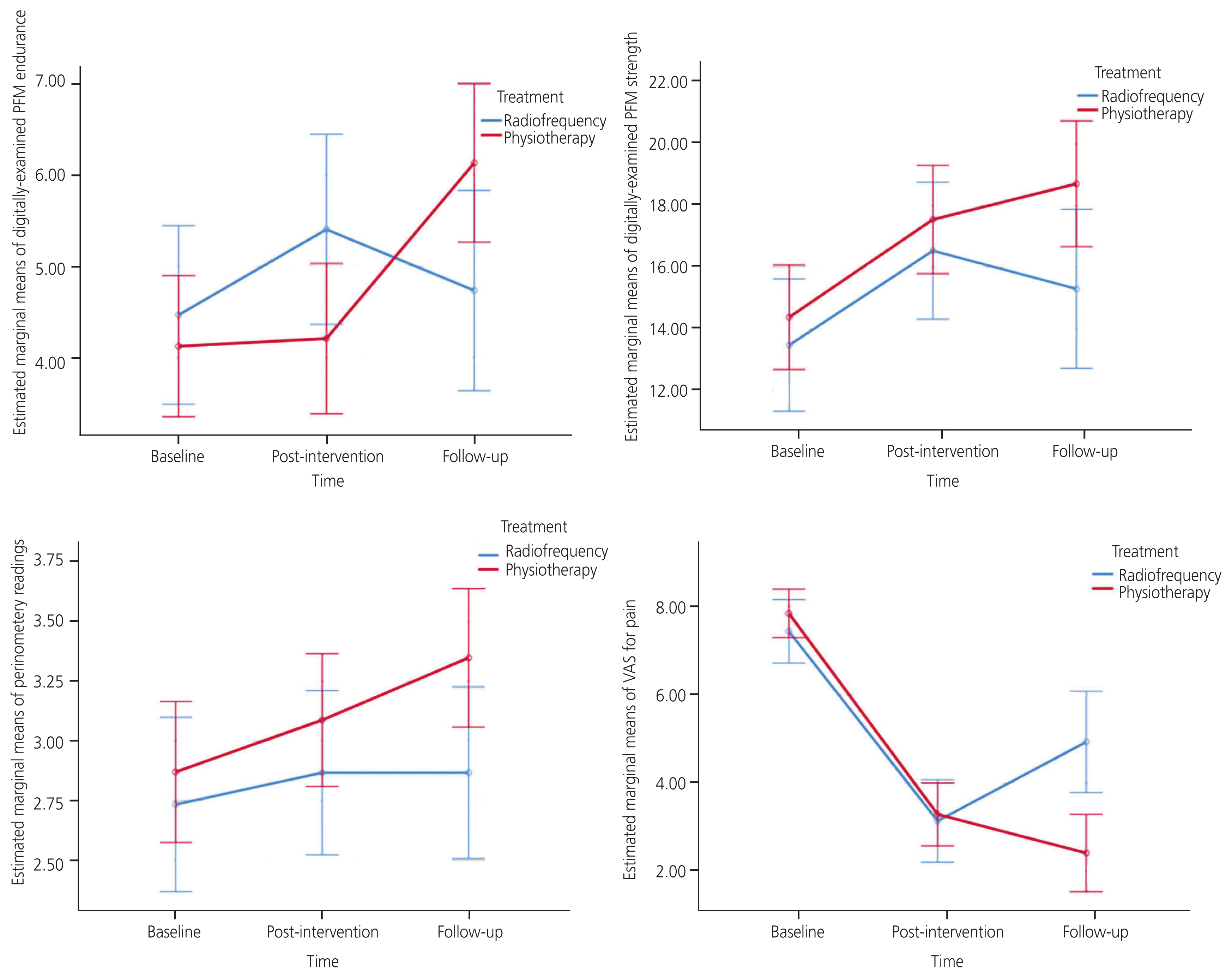
Results
The 6-session therapy in the RM group and the manual, biofeedback, and transcutaneous electrical nerve stimulation therapies in the physiotherapy group were similarly effective in reducing pain and improving PFM endurance after the final intervention session in each group, whereas perineometer readings and PFM strength were associated with greater improvements in the physiotherapy group.
Conclusion
The results of this study demonstrated comparable effectiveness of RM in the management of MPPS and improvement of PFM function compared to routine physiotherapy programs with fewer sessions of therapy.
Keyword
Figure
Reference
-
References
1. Howard FM. Chronic pelvic pain. Obstet Gynecol. 2003; 101:594–611.
Article2. Fall M, Baranowski AP, Elneil S, Engeler D, Hughes J, Messelink EJ, et al. EAU guidelines on chronic pelvic pain. Eur Urol. 2010; 57:35–48.
Article3. Ahangari A. Prevalence of chronic pelvic pain among women: an updated review. Pain Physician. 2014; 17:E141–7.4. Engeler DS, Baranowski AP, Dinis-Oliveira P, Elneil S, Hughes J, Messelink EJ, et al. The 2013 EAU guidelines on chronic pelvic pain: is management of chronic pelvic pain a habit, a philosophy, or a science? 10 years of development. European Urology. 2013; 64:431–9.
Article5. Divandari N, Manshadi FD, Shokouhi N, Vakili M, Jaberzadeh S. Effect of one session of tDCS on the severity of pain in women with chronic pelvic pain. J Bodyw Mov Ther. 2019; 23:678–82.
Article6. Newham AP, Van der Spuy ZM, Nugent F. Laparoscopic findings in women with chronic pelvic pain. S Afr Med J. 1996; 86:1200–3.7. Pastore EA, Katzman WB. Recognizing myofascial pelvic pain in the female patient with chronic pelvic pain. J Obstet Gynecol Neonatal Nurs. 2012; 41:680–91.
Article8. Sedighimehr N, Manshadi FD, Shokouhi N, Baghban AA. Pelvic musculoskeletal dysfunctions in women with and without chronic pelvic pain. J Bodyw Mov Ther. 2018; 22:92–6.
Article9. Spitznagle TM, Robinson CM. Myofascial pelvic pain. Obstet Gynecol Clin North Am. 2014; 41:409–32.
Article10. Masterson TA, Masterson JM, Azzinaro J, Manderson L, Swain S, Ramasamy R. Comprehensive pelvic floor physical therapy program for men with idiopathic chronic pelvic pain syndrome: a prospective study. Transl Androl Urol. 2017; 6:910–5.11. Küçük EV, Suçeken FY, Bindayl A, Boylu U, Onol FF, Gümüş E. Effectiveness of acupuncture on chronic prostatitis-chronic pelvic pain syndrome category IIIB patients: a prospective, randomized, nonblinded, clinical trial. Urology. 2015; 85:636–40.
Article12. Anderson RU, Wise D, Sawyer T, Nathanson BH, Nevin Smith J. Equal improvement in men and women in the treatment of urologic chronic pelvic pain syndrome using a multi-modal protocol with an internal myofascial trigger point wand. Appl Psychophysiol Biofeedback. 2016; 41:215–24.
Article13. Slocumb JC. Neurological factors in chronic pelvic pain: trigger points and the abdominal pelvic pain syndrome. Am J Obstet Gynecol. 1984; 149:536–43.
Article14. FitzGerald MP, Payne CK, Lukacz ES, Yang CC, Peters KM, Chai TC, et al. Randomized multicenter clinical trial of myofascial physical therapy in women with interstitial cystitis/painful bladder syndrome and pelvic floor tenderness. J Urol. 2012; 187:2113–8.
Article15. Fuentes-Márquez P, Cabrera-Martos I, Valenza MC. Physiotherapy interventions for patients with chronic pelvic pain: a systematic review of the literature. Physiother Theory Pract. 2019; 35:1131–8.
Article16. Chiarioni G, Nardo A, Vantini I, Romito A, Whitehead WE. Biofeedback is superior to electrogalvanic stimulation and massage for treatment of levator ani syndrome. Gastroenterology. 2010; 138:1321–9.
Article17. Harvey MP, Watier A, Dufort Rouleau É, Léonard G. Non-invasive stimulation techniques to relieve abdominal/pelvic pain: is more always better? World J Gastroenterol. 2017; 23:3758–60.
Article18. Balogun JA, Okonofua FE. Management of chronic pelvic inflammatory disease with shortwave diathermy. A case report. Phys Ther. 1988; 68:1541–5.19. Lamina S, Hanif S. Shortwave diathermy in the management of chronic pelvic inflammatory disease pain. J Niger Soc Phys Sci. 2008; 16:31–6.20. Lamina S, Hanif S, Gagarawa YS. Short wave diathermy in the symptomatic management of chronic pelvic inflammatory disease pain: a randomized controlled trial. Physiother Res Int. 2011; 16:50–6.
Article21. Sanses TV, Chelimsky G, McCabe NP, Zolnoun D, Janata J, Elston R, et al. The pelvis and beyond: musculoskeletal tender points in women with chronic pelvic pain. Clin J Pain. 2016; 32:659–65.22. Dehghan MF, Ghanbari Z, Foroutan M, Kouhpayehzadeh EJ, Moshtaghi Z. Chronic pelvic pain frequency among a group of Iranian employed women. Tehran Univ Med J. 2009; 66:767–73.23. Seidi F, Rajabi R, Ebrahimi TI, Tavanai AR, Moussavi SJ. The Iranian flexible ruler reliability and validity in lumbar lordosis measurements. World J Sport Sci. 2009; 2:95–9.24. Laycock J. Clinical evaluation of the pelvic floor. Schussler B, Laycock J, Norton P, Stanton SL, editors. Pelvic floor re-education. 2nd ed. London: Springer-Verlag;1994. p. 42–8.25. Whitehead AL, Julious SA, Cooper CL, Campbell MJ. Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Stat Methods Med Res. 2016; 25:1057–73.
Article26. Masiero S, Pignataro A, Piran G, Duso M, Mimche P, Ermani M, et al. Short-wave diathermy in the clinical management of musculoskeletal disorders: a pilot observational study. Int J Biometeorol. 2020; 64:981–8.
Article27. Low J. Dosage of some pulsed shortwave clinical trials. Physiotherapy. 1995; 81:611–6.
Article28. Shields N, Gormley J, O’Hare N. Short-wave diathermy: current clinical and safety practices. Physiother Res Int. 2002; 7:191–202.
Article29. Vural M. Pelvic pain rehabilitation. Turk J Phys Med Rehabil. 2018; 64:291–9.
Article30. Bedaiwy MA, Patterson B, Mahajan S. Prevalence of myofascial chronic pelvic pain and the effectiveness of pelvic floor physical therapy. J Reprod Med. 2013; 58:504–10.31. Yaraghi M, Ghazizadeh S, Mohammadi F, Ashtiani EM, Bakhtiyari M, Mareshi SM, et al. Comparing the effectiveness of functional electrical stimulation via sexual cognitive/behavioral therapy of pelvic floor muscles versus local injection of botulinum toxin on the sexual functioning of patients with primary vaginismus: a randomized clinical trial. Int Urogynecol J. 2019; 30:1821–8.
Article32. de Oliveira Bernardes N, Bahamondes L. Intravaginal electrical stimulation for the treatment of chronic pelvic pain. J Reprod Med. 2005; 50:267–72.33. Noor N, Roy KK, Zangmo R, Das A, Rai R, Kumari A, et al. Role of para-cervical block in reducing immediate postoperative pain after total laparoscopic hysterectomy: a prospective randomized placebo-controlled trial. Obstet Gynecol Sci. 2021; 64:122–9.
Article34. Comba C, Demirayak G, Erdogan SV, Karaca I, Demir O, Guler O, et al. Comparison of pain and proper sample status according to usage of tenaculum and analgesia: a randomized clinical trial. Obstet Gynecol Sci. 2020; 63:506–13.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment Experience of Pulsed Radiofrequency Under Ultrasound Guided to the Trapezius Muscle at Myofascial Pain Syndrome: A Case Report
- Effects of Intramuscular Electrical Stimulation Using Inversely Placed Electrodes on Myofascial Pain Syndrome in the Shoulder: A Case Series
- Obturator Internus Myofascial Pain: A Cause of Undiagnosed Chronic Pelvic Pain Syndrome: Case reports
- Response to: Influence of Tensioner’s Mobilization on the Centralization of Symptoms in Cervicobrachial Pain Syndrome: A Randomized Controlled Trial
- Botulinum Toxin-Type A in Cervical Myofascial Pain Syndrome: A report of 3 cases