Korean J Schizophr Res.
2023 Apr;26(1):24-31. 10.16946/kjsr.2023.26.1.24.
One-Year Clinical Outcomes After Diagnosis According to Early Medication Adherence in First-Episode Schizophrenia: A Nationwide, Health Insurance Data-Based Retrospective Cohort Study
- Affiliations
-
- 1Department of Psychiatry, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2542197
- DOI: http://doi.org/10.16946/kjsr.2023.26.1.24
Abstract
Objectives
Early pharmacologic intervention is considered necessary for improving the prognosis in patients with first-episode schizophrenia (FES). However, few nationwide population-based studies have focused on early medication adherence. We investigated the status of early adherence to antipsychotics and the effect of early adherence on later clinical outcomes in FES.
Methods
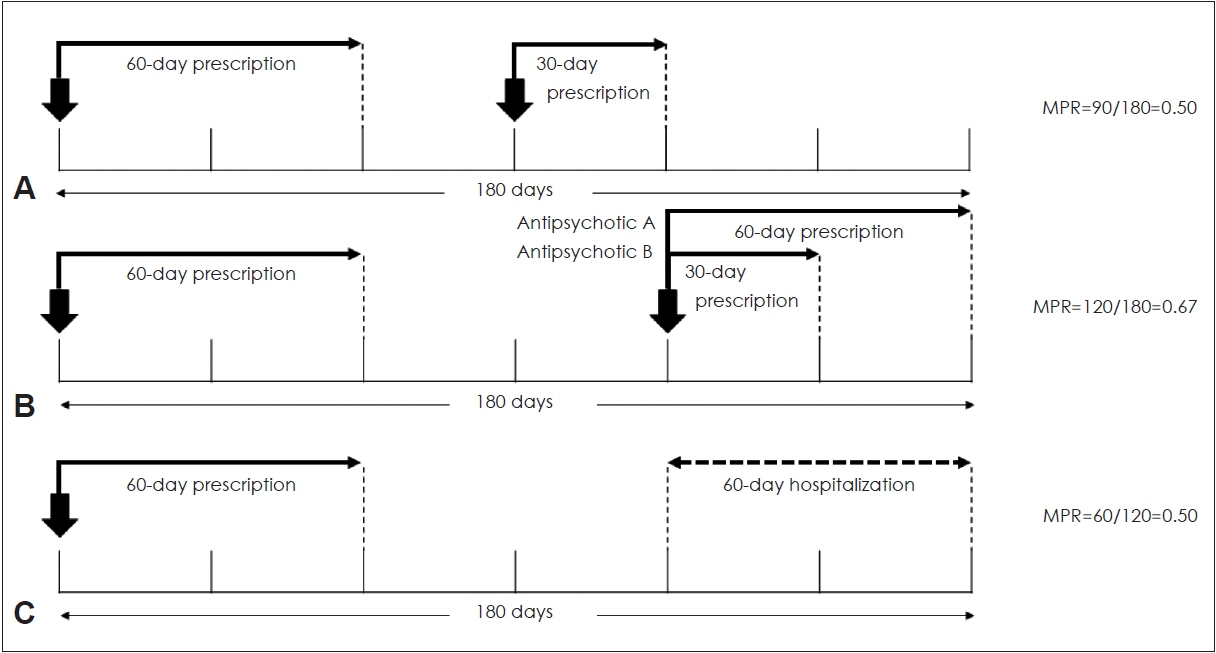
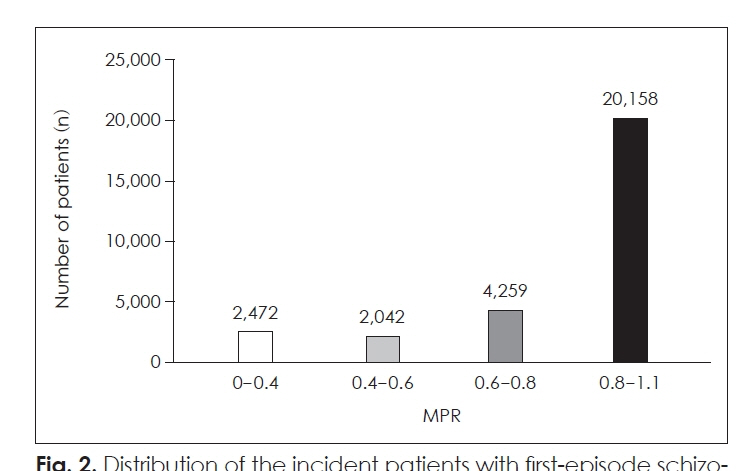
We used data from the South Korean Health Insurance Review Agency database (2009-2021). We selected 28,931 patients with FES who had a prescription record of at least one antipsychotic medication within 180 days after their diagnosis. We measured early medication adherence using the medication possession ratio (MPR) and compared demographic characteristics and results of psychiatric hospitalization between the adherence group (0.6≤MPR<1.1) and the non-adherence group (MPR<0.6).
Results
The average early medication adherence was 0.82 by MPR, and the non-adherence group accounted for 15.6% of all subjects. From 1 to 2 years after diagnosis, the adherence group showed a higher number of psychiatric hospitalizations per hospitalized patient but a shorter duration than the non-adherence group. Additionally, the proportion of patients who experienced psychiatric hospitalizations was smaller in the adherence group.
Conclusion
In patients with FES, early medication adherence is associated with lower rates of psychiatric hospitalization and shorter hospitalization durations.
Keyword
Figure
Cited by 1 articles
-
Recent Insights in the Treatment for Clinical High Risk for Psychosis and Recent Onset Psychosis
Sunyoung Park, Young Tak Jo, Ji Sung Lee, JungSun Lee, Il Ho Park
Korean J Schizophr Res. 2024;27(2):35-48. doi: 10.16946/kjsr.2024.27.2.35.
Reference
-
1. Saha S, Chant D, Welham J, McGrath J. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005; 2:e141.
Article2. Chong HY, Teoh SL, Wu DB, Kotirum S, Chiou CF, Chaiyakunapruk N. Global economic burden of schizophrenia: a systematic review. Neuropsychiatr Dis Treat. 2016; 12:357–373.
Article3. Cho SJ, Kim J, Kang YJ, Lee SY, Seo HY, Park JE, et al. Annual Prevalence and Incidence of Schizophrenia and Similar Psychotic Disorders in the Republic of Korea: A National Health Insurance Data-Based Study. Psychiatry Investig. 2020; 17:61–70.
Article4. Jo M, Kim HJ, Rim SJ, Lee MG, Kim CE, Park S. The cost-of-illness trend of schizophrenia in South Korea from 2006 to 2016. PLoS One. 2020; 15:e0235736.
Article5. McGorry PD, Killackey E, Yung A. Early intervention in psychosis: concepts, evidence and future directions. World Psychiatry. 2008; 7:148–156.
Article6. Marshall M, Rathbone J. Early intervention for psychosis. Cochrane Database Syst Rev. 2011; CD004718.
Article7. Park JI, Jeon M. The Stigma of Mental Illness in Korea. J Korean Neuropsychiatr Assoc. 2016; 55:299–309.
Article8. Kane JM, Marder SR. Psychopharmacologic Treatment of Schizophrenia. Schizophrenia Bulletin. 1993; 19:287–302.
Article9. Dixon LB, Lehman AF, Levine J. Conventional Antipsychotic Medications for Schizophrenia. Schizophrenia Bulletin. 1995; 21:567–577.
Article10. Geddes J, Freemantle N, Harrison P, Bebbington P. Atypical antipsychotics in the treatment of schizophrenia: systematic overview and meta-regression analysis. BMJ. 2000; 321:1371.
Article11. Tiihonen J, Walhbeck K, Lönnqvist J, Klaukka T, Ioannidis JPA, Volavka J, et al. Effectiveness of antipsychotic treatments in a nationwide cohort of patients in community care after first hospitalisation due to schizophrenia and schizoaffective disorder: observational follow-up study. BMJ. 2006; 333:224.
Article12. Leucht S, Tardy M, Komossa K, Heres S, Kissling W, Salanti G, et al. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: a systematic review and meta-analysis. The Lancet. 2012; 379:2063–2071.
Article13. Higashi K, Medic G, Littlewood KJ, Diez T, Granstrom O, De Hert M. Medication adherence in schizophrenia: factors influencing adherence and consequences of nonadherence, a systematic literature review. Ther Adv Psychopharmacol. 2013; 3:200–218.
Article14. Leclerc E, Noto C, Bressan RA, Brietzke E. Determinants of adherence to treatment in first-episode psychosis: a comprehensive review. Braz J Psychiatry. 2015; 37:168–176.
Article15. Knapp M, King D, Pugner K, Lapuerta P. Non-adherence to antipsychotic medication regimens: associations with resource use and costs. Br J Psychiatry. 2004; 184:509–516.
Article16. Rittmannsberger H, Pachinger T, Keppelmüller P, Wancata J. Medication adherence among psychotic patients before admission to inpatient treatment. Psychiatr Serv. 2004; 55:174–179.
Article17. Valenstein M, Copeland LA, Blow FC, McCarthy JF, Zeber JE, Gillon L, et al. Pharmacy Data Identify Poorly Adherent Patients with Schizophrenia at Increased Risk for Admission. Medical Care. 2002; 40:630–639.
Article18. Eaddy M, Grogg A, Locklear J. Assessment of compliance with antipsychotic treatment and resource utilization in a Medicaid population. Clin Ther. 2005; 27:263–272.
Article19. Lang K, Meyers JL, Korn JR, Lee S, Sikirica M, Crivera C, et al. Medication adherence and hospitalization among patients with schizophrenia treated with antipsychotics. Psychiatr Serv. 2010; 61:1239–1247.
Article20. Offord S, Lin J, Mirski D, Wong B. Impact of early nonadherence to oral antipsychotics on clinical and economic outcomes among patients with schizophrenia. Adv Ther. 2013; 30:286–297.
Article21. Kuwabara H, Saito Y, Mahlich J. Adherence and rehospitalizations in patients with schizophrenia: evidence from Japanese claims data. Neuropsychiatr Dis Treat. 2015; 11:935–940.22. Hardy M, Jackson C, Byrne J. Antipsychotic adherence and emergency department utilization among patients with schizophrenia. Schizophr Res. 2018; 201:347–351.
Article23. Cho MJ, Seong SJ, Park JE, Chung IW, Lee YM, Bae A, et al. Prevalence and Correlates of DSM-IV Mental Disorders in South Korean Adults: The Korean Epidemiologic Catchment Area Study 2011. Psychiatry Investig. 2015; 12:164–170.
Article24. Heo JU, Kim DW, Oh ST, Choi WJ, Park J. Clinical Characteristics, Drug Adherence to Antipsychotics and Medical Use Trends in Patients First Diagnosed with Psychotic Disorder: A Preliminary Study. Korean Journal of Schizophrenia Research. 2019; 22:42–50.
Article25. Cho SJ, Kim J, Lee JY, Sohn JH. Adherence to Antipsychotic Drugs by Medication Possession Ratio for Schizophrenia and Similar Psychotic Disorders in the Republic of Korea: A Retrospective Cohort Study. Clin Psychopharmacol Neurosci. 2022; 20:491–497.
Article26. Boden R, Brandt L, Kieler H, Andersen M, Reutfors J. Early non-adherence to medication and other risk factors for rehospitalization in schizophrenia and schizoaffective disorder. Schizophr Res. 2011; 133:36–41.
Article27. Kim JA, Yoon S, Kim LY, Kim DS. Towards Actualizing the Value Potential of Korea Health Insurance Review and Assessment (HIRA) Data as a Resource for Health Research: Strengths, Limitations, Applications, and Strategies for Optimal Use of HIRA Data. J Korean Med Sci. 2017; 32:718–728.
Article28. Steiner JF, Koepsell TD, Fihn SD, Inui TS. A general method of compliance assessment using centralized pharmacy records. Description and validation. Med Care. 1988; 26:814–823.
Article29. Valenstein M, Blow FC, Copeland LA, McCarthy JF, Zeber JE, Gillon L, et al. Poor antipsychotic adherence among patients with schizophrenia: medication and patient factors. Schizophr Bull. 2004; 30:255–264.
Article30. Weiden PJ, Kozma C, Grogg A, Locklear J. Partial compliance and risk of rehospitalization among California Medicaid patients with schizophrenia. Psychiatr Serv. 2004; 55:886–891.
Article31. Vollmer WM, Xu M, Feldstein A, Smith D, Waterbury A, Rand C. Comparison of pharmacy-based measures of medication adherence. BMC Health Serv Res. 2012; 12:155.
Article32. Grossman LS, Harrow M, Rosen C, Faull R, Strauss GP. Sex differences in schizophrenia and other psychotic disorders: a 20-year longitudinal study of psychosis and recovery. Compr Psychiatry. 2008; 49:523–529.
Article33. Vila-Rodriguez F, Ochoa S, Autonell J, Usall J, Haro JM. Complex interaction between symptoms, social factors, and gender in social functioning in a community-dwelling sample of schizophrenia. Psychiatr Q. 2011; 82:261–274.
Article34. Bozikas VP, Kosmidis MH, Peltekis A, Giannakou M, Nimatoudis I, Karavatos A, et al. Sex differences in neuropsychological functioning among schizophrenia patients. Aust N Z J Psychiatry. 2010; 44:333–341.
Article35. Vaskinn A, Sundet K, Simonsen C, Hellvin T, Melle I, Andreassen OA. Sex differences in neuropsychological performance and social functioning in schizophrenia and bipolar disorder. Neuropsychology. 2011; 25:499–510.
Article36. Yang J, Ko YH, Paik JW, Le MS, Han C, Joe SH, et al. Symptom severity and attitudes toward medication: impacts on adherence in outpatients with schizophrenia. Schizophr Res. 2012; 134:226–231.
Article37. Coldham EL, Addington J, Addington D. Medication adherence of individuals with a first episode of psychosis. Acta Psychiatr Scand. 2002; 106:286–290.
Article38. Häfner H, Maurer K, Löffler W, Riecher-Rössler A. The Influence of Age and Sex on the Onset and Early Course of Schizophrenia. The British Journal of Psychiatry. 1993; 162:80–86.
Article39. Burns T. Evolution of outcome measures in schizophrenia. The British Journal of Psychiatry. 2007; 191:s1–s6.
Article40. Burns T. Hospitalisation as an outcome measure in schizophrenia. The British Journal of Psychiatry. 2007; 191:s37–s41.
Article41. Addington DE, McKenzie E, Wang J. Validity of hospital admission as an outcome measure of services for first-episode psychosis. Psychiatr Serv. 2012; 63:280–282.
Article42. Woo JH, Grinspan Z, Shapiro J, Rhee SY. Frequent Users of Hospital Emergency Departments in Korea Characterized by Claims Data from the National Health Insurance: A Cross Sectional Study. PLOS ONE. 2016; 11:e0147450.
Article43. Blonde L, Khunti K, Harris SB, Meizinger C, Skolnik NS. Interpretation and Impact of Real-World Clinical Data for the Practicing Clinician. Adv Ther. 2018; 35:1763–1774.
Article44. Go DS, Shin KC, Paik JW, Kim KA, Yoon SJ. A Review of the Admission System for Mental Disorders in South Korea. Int J Environ Res Public Health. 2020; 17:9159.
Article45. Kim AM. Psychiatric hospitalization in Korea, 2011-2020: the impact of the Mental Health Act revision of 2017 in consideration of the COVID-19 pandemic. Asian J Psychiatr. 2022; 68:102934.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adherence to Antipsychotic Drugs by Medication Possession Ratio for Schizophrenia and Similar Psychotic Disorders in the Republic of Korea: A Retrospective Cohort Study
- A comparison of methods for the measurement of adherence to antihypertensive multidrug therapy and the clinical consequences: a retrospective cohort study using the Korean nationwide claims database
- Long-acting Injectable Antipsychotics in First-episode Schizophrenia
- Factors Affecting Medication Adherence in Patients with Rheumatoid Arthritis
- Association between Medication Adherence and Duration of Outpatient Treatment in Patients with Schizophrenia