J Korean Neurosurg Soc.
2023 May;66(3):324-331. 10.3340/jkns.2022.0068.
Outcome Analysis of External Neurolysis in Posture-Induced Compressive Peroneal Neuropathy and the Utility of Magnetic Resonance Imaging in the Treatment Process
- Affiliations
-
- 1Department of Neurosurgery, Chuncheon Sacred Heart Hospital, College of Medicine, Hallym University, Chuncheon, Korea
- KMID: 2542018
- DOI: http://doi.org/10.3340/jkns.2022.0068
Abstract
Objective
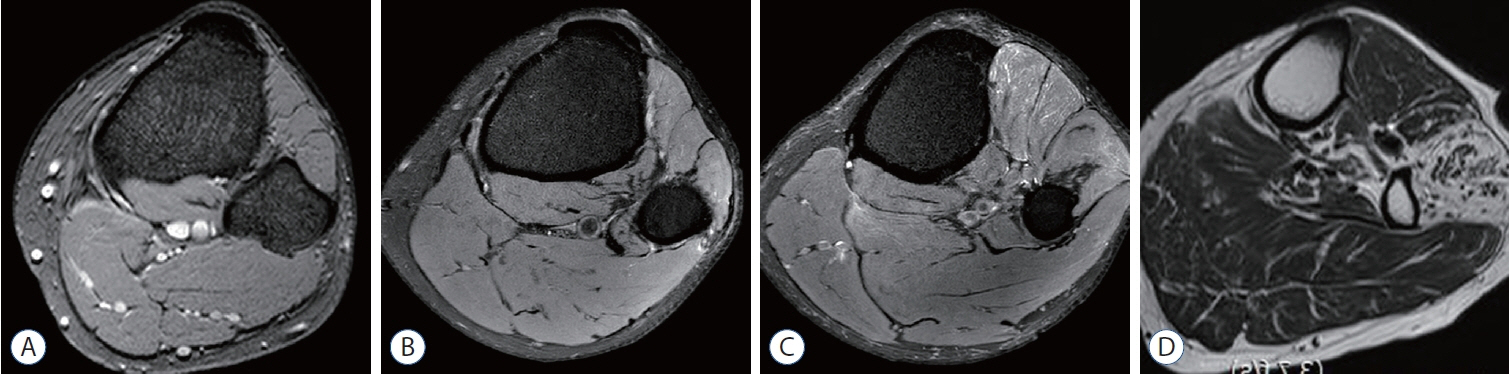
: We aimed to analyze the effectiveness of external neurolysis on the common peroneal nerve (CPN) in patients with posture-induced compressive peroneal neuropathy (PICPNe). Further, we aimed to examine the utility of magnetic resonance imaging (MRI) in assessing the severity of denervation status and predicting the postoperative prognosis.
Methods
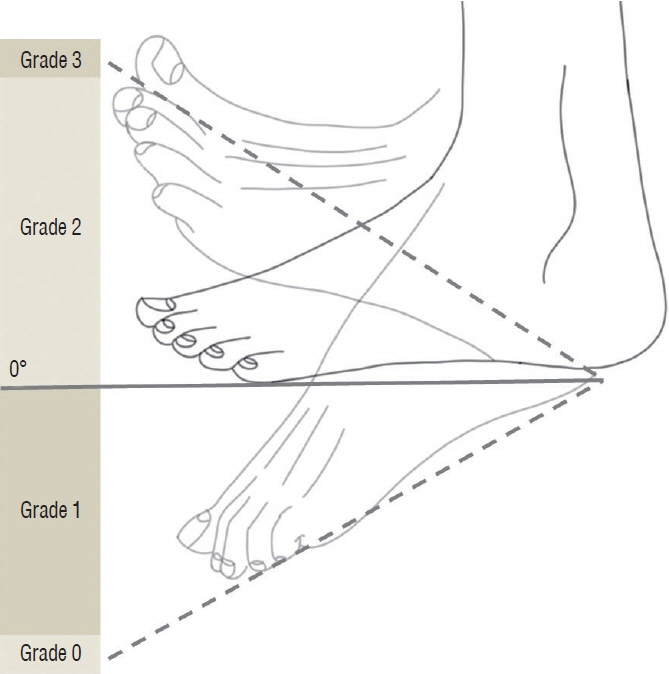
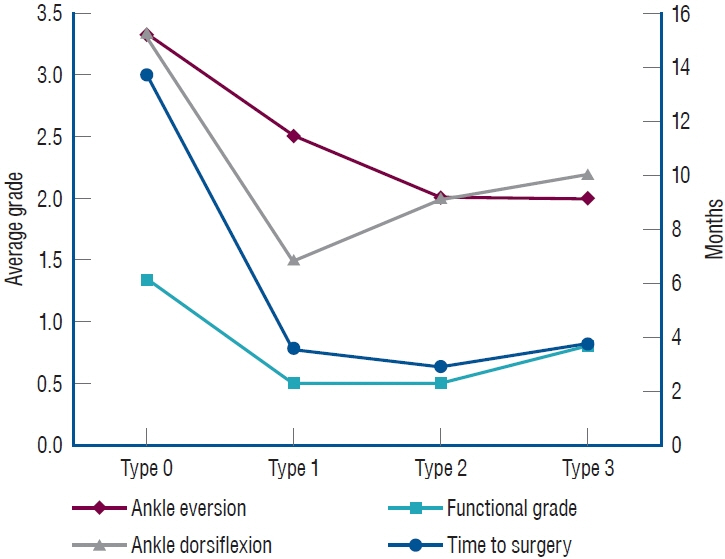
: We included 13 patients (eight males and five females) with foot drop who underwent CPN decompression between 2018 and 2020. We designed a grading system for assessing the postoperative functional outcome. Additionally, we performed MRI to evaluate the denervation status of the affected musculature and its effect on postoperative recovery.
Results
: The median time to surgery was 3 months. The median preoperative ankle dorsiflexion and eversion grades were both 3, while the average functional grade was 1. Posterior crural intermuscular septum was the most common cause of nerve compression, followed by deep tendinous fascia and anterior crural intermuscular septum. There was a significant postoperative improvement in the median postoperative ankle dorsiflexion and eversion grades and average postoperative functional (4, 5, and 2.38, respectively). Preoperative ankle eversion was significantly correlated with denervation status. Additionally, the devernation status on MRI was positively correlated with the outcome favorability. However, denervation atrophy led to a less favorable outcome.
Conclusion
: Among patients with intractable PICPNe despite conservative management, surgical intervention could clinically improve motor function and functional ability. Additionally, MRI examination of the affected muscle could help diagnose CPNe and assess the postoperative prognosis.
Keyword
Figure
Reference
-
References
1. Bendszus M, Koltzenburg M, Wessig C, Solymosi L. Sequential MR imaging of denervated muscle: experimental study. AJNR Am J Neuroradiol. 23:1427–1431. 2002.2. Bowley MP, Doughty CT. Entrapment neuropathies of the lower extremity. Med Clin North Am. 103:371–382. 2019.
Article3. Dellon AL, Ebmer J, Swier P. Anatomic variations related to decompression of the common peroneal nerve at the fibular head. Ann Plast Surg. 48:30–34. 2002.
Article4. Humphreys DB, Novak CB, Mackinnon SE. Patient outcome after common peroneal nerve decompression. J Neurosurg. 107:314–318. 2007.
Article5. Kim J, Ko HC, Son BC. Common peroneal nerve palsy due to deep tendinous fascia superficial to the soleus muscle: a case report. Nerve. 4:5–7. 2018.
Article6. Kishi M, Sakakibara R, Takahashi O, Nakamura H, Tateno F, Tsuyusaki Y, et al. Seiza-induced neuropathy: an occupational peroneal neuropathy in a Japanese lady. Neurol Sci. 38:1521–1522. 2017.
Article7. Maalla R, Youssef M, Ben Lassoued N, Sebai MA, Essadam H. Peroneal nerve entrapment at the fibular head: outcomes of neurolysis. Orthop Traumatol Surg Res. 99:719–722. 2013.
Article8. Ninković M, Ninković M. Neuromusculotendinous transfer: an original surgical concept for the treatment of drop foot with long-term followup. Plast Reconstr Surg. 132:438e–445e. 2013.9. Poage C, Roth C, Scott B. Peroneal nerve palsy: evaluation and management. J Am Acad Orthop Surg. 24:1–10. 2016.10. Souter J, Swong K, McCoyd M, Balasubramanian N, Nielsen M, Prabhu VC. Surgical results of common peroneal nerve neuroplasty at lateral fibular neck. World Neurosurg. 112:e465–e472. 2018.
Article11. Viddeleer AR, Sijens PE, van Ooyen PM, Kuypers PD, Hovius SE, Oudkerk M. Sequential MR imaging of denervated and reinnervated skeletal muscle as correlated to functional outcome. Radiology. 264:522–530. 2012.
Article12. Wilson C, Yaacoub AP, Bakare A, Bo N, Aasar A, Barbaro NM. Peroneal nerve decompression: institutional review and meta-analysis to identify prognostic associations with favorable and unfavorable surgical outcomes. J Neurosurg Spine. 30:714–721. 2019.
Article13. Yu JK, Yang JS, Kang SH, Cho YJ. Clinical characteristics of peroneal nerve palsy by posture. J Korean Neurosurg Soc. 53:269–273. 2013.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Common Peroneal Nerve Injuries
- Right Common Peroneal Neuropathy after Vaginal Delivery
- Anatomical Variants of “Short Head of Biceps Femoris Muscle†Associated with Common Peroneal Neuropathy in Korean Populations : An MRI Based Study
- Compression Neuropathy of Superficial Peroneal Nerve and Deep Peroneal Nerve Following Acupuncture Treatment: A Case Report
- Injury to the Left Sciatic and Right Common Peroneal Nerves Combined With Multifocal Rhabdomyolysis in a Survivor of the Itaewon Crowd Crush: A Case Report