J Yeungnam Med Sci.
2023 Apr;40(2):172-178. 10.12701/jyms.2022.00500.
Comparison of the efficacy of erector spinae plane block according to the difference in bupivacaine concentrations for analgesia after laparoscopic cholecystectomy: a retrospective study
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea
- KMID: 2541943
- DOI: http://doi.org/10.12701/jyms.2022.00500
Abstract
- Background
Laparoscopic cholecystectomy (LC) is a noninvasive surgery, but postoperative pain is a major problem. Studies have indicated that erector spinae plane block (ESPB) has an analgesic effect after LC. We aimed to compare the efficacy of different ESPB anesthetic concentrations in pain control in patients with LC.
Methods
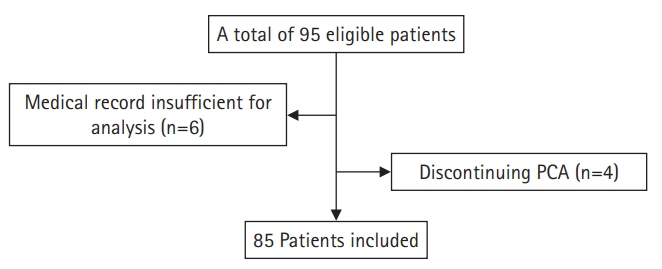
This retrospective study included patients aged 20 to 75 years scheduled for LC with the American Society of Anesthesiologists physical status classification I or II. ESPB was administered using 0.375% bupivacaine in group 1 and 0.25% in group 2. Both groups received general anesthesia. Postoperative tramadol consumption and pain scores were compared and intraoperative and postoperative fentanyl requirements in the postanesthesia care unit (PACU) were measured.
Results
Eighty-five patients were included in this analysis. Tramadol consumption in the first 12 hours, second 12 hours, and total 24 hours was similar between groups (p>0.05). The differences between postoperative numeric rating scale (NRS) scores at rest did not differ significantly. The postoperative NRS scores upon bodily movement were not statistically different between the two groups, except at 12 hours. The mean intraoperative and postoperative fentanyl requirements in the PACU were similar. The difference in the requirement for rescue analgesics was not statistically significant (p=0.788).
Conclusion
Ultrasound-guided ESPB performed with different bupivacaine concentrations was effective in both groups for LC analgesia, with similar opioid consumption. A lower concentration of local anesthetic can be helpful for the safety of regional anesthesia and is recommended for the analgesic effect of ESPB in LC.
Keyword
Figure
Reference
-
References
1. Alexander JI. Pain after laparoscopy. Br J Anaesth. 1997; 79:369–78.2. Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology. 2013; 118:934–44.3. Shin HJ, Oh AY, Baik JS, Kim JH, Han SH, Hwang JW. Ultrasound-guided oblique subcostal transversus abdominis plane block for analgesia after laparoscopic cholecystectomy: a randomized, controlled, observer-blinded study. Minerva Anestesiol. 2014; 80:185–93.4. Kehlet H. Postoperative pain, analgesia, and recovery-bedfellows that cannot be ignored. Pain. 2018; 159(9 Suppl 1):S11–6.5. Fregoso G, Wang A, Tseng K, Wang J. Transition from acute to chronic pain: evaluating risk for chronic postsurgical pain. Pain Physician. 2019; 22:479–88.6. Safa R, Sadovnikoff N. Anesthesia for patients with concomitant cardiac and renal dysfunction. Anesthesiol Clin. 2016; 34:697–710.7. Erol DD, Yilmaz S, Polat C, Arikan Y. Efficacy of thoracic epidural analgesia for laparoscopic cholecystectomy. Adv Ther. 2008; 25:45–52.8. Aydin G, Aydin O. The efficacy of ultrasound-guided paravertebral block in laparoscopic cholecystectomy. Medicina (Kaunas). 2018; 54:75.9. Altıparmak B, Korkmaz Toker M, Uysal AI, Kuşçu Y, Gümüş Demirbilek S. Ultrasound-guided erector spinae plane block versus oblique subcostal transversus abdominis plane block for postoperative analgesia of adult patients undergoing laparoscopic cholecystectomy: randomized, controlled trial. J Clin Anesth. 2019; 57:31–6.10. Aygun H, Kavrut Ozturk N, Pamukcu AS, Inal A, Kiziloglu I, Thomas DT, et al. Comparison of ultrasound guided erector spinae plane block and quadratus lumborum block for postoperative analgesia in laparoscopic cholecystectomy patients; a prospective randomized study. J Clin Anesth. 2020; 62:109696.11. Tulgar S, Kapakli MS, Senturk O, Selvi O, Serifsoy TE, Ozer Z. Evaluation of ultrasound-guided erector spinae plane block for postoperative analgesia in laparoscopic cholecystectomy: a prospective, randomized, controlled clinical trial. J Clin Anesth. 2018; 49:101–6.12. Cesur S, Y R Ko Lu HU, Aksu C, Ku A. Bilateral versus unilateral erector spinae plane block for postoperative analgesia in laparoscopic cholecystectomy: a randomized controlled study. Braz J Anesthesiol. 2023; 73:72–7.13. Vrsajkov V, Ilić N, Uvelin A, Ilić R, Lukić-Šarkanović M, Plećaš-Đurić A. Erector spinae plane block reduces pain after laparoscopic cholecystectomy. Anaesthesist. 2021; 70(Suppl 1):48–52.14. Ozdemir H, Araz C, Karaca O, Turk E. Comparison of ultrasound-guided erector spinae plane block and subcostal transversus abdominis plane block for postoperative analgesia after laparoscopic cholecystectomy: a randomized, controlled trial. J Invest Surg. 2022; 35:870–7.15. Liu H, Brown M, Sun L, Patel SP, Li J, Cornett EM, et al. Complications and liability related to regional and neuraxial anesthesia. Best Pract Res Clin Anaesthesiol. 2019; 33:487–97.16. Albrecht E, Chin KJ. Advances in regional anaesthesia and acute pain management: a narrative review. Anaesthesia. 2020; 75(Suppl 1):e101–10.17. Blichfeldt-Eckhardt MR, Ording H, Andersen C, Licht PB, Toft P. Early visceral pain predicts chronic pain after laparoscopic cholecystectomy. Pain. 2014; 155:2400–7.18. Kumar K, Kirksey MA, Duong S, Wu CL. A review of opioid-sparing modalities in perioperative pain management: methods to decrease opioid use postoperatively. Anesth Analg. 2017; 125:1749–60.19. Daghmouri MA, Akremi S, Chaouch MA, Mesbahi M, Amouri N, Jaoua H, et al. Bilateral erector spinae plane block for postoperative analgesia in laparoscopic cholecystectomy: a systematic review and meta-analysis of randomized controlled trials. Pain Pract. 2021; 21:357–65.20. Rosenberg PH, Veering BT, Urmey WF. Maximum recommended doses of local anesthetics: a multifactorial concept. Reg Anesth Pain Med. 2004; 29:564–75.21. Barrington MJ, Watts SA, Gledhill SR, Thomas RD, Said SA, Snyder GL, et al. Preliminary results of the Australasian Regional Anaesthesia Collaboration: a prospective audit of more than 7000 peripheral nerve and plexus blocks for neurologic and other complications. Reg Anesth Pain Med. 2009; 34:534–41.22. Barrington MJ, Kluger R. Ultrasound guidance reduces the risk of local anesthetic systemic toxicity following peripheral nerve blockade. Reg Anesth Pain Med. 2013; 38:289–99.23. El-Boghdadly K, Pawa A. The erector spinae plane block: plane and simple. Anaesthesia. 2017; 72:434–8.24. Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016; 41:621–7.25. Murouchi T, Iwasaki S, Yamakage M. Chronological changes in ropivacaine concentration and analgesic effects between transversus abdominis plane block and rectus sheath block. Reg Anesth Pain Med. 2015; 40:568–71.26. Toju K, Shiraishi K, Hakozaki T, Isosu T, Murakawa M. Plasma ropivacaine concentration following ultrasound-guided subcostal transversus abdominis plane block in adults. J Anesth. 2015; 29:146–8.27. El-Boghdadly K, Pawa A, Chin KJ. Local anesthetic systemic toxicity: current perspectives. Local Reg Anesth. 2018; 11:35–44.28. Miranda P, Corvetto MA, Altermatt FR, Araneda A, Echevarría GC, Cortínez LI. Levobupivacaine absorption pharmacokinetics with and without epinephrine during TAP block: analysis of doses based on the associated risk of local anaesthetic toxicity. Eur J Clin Pharmacol. 2016; 72:1221–7.29. Hamilton DL. Pneumothorax following erector spinae plane block. J Clin Anesth. 2019; 52:17.30. Piraccini E, Poggi P, Maitan S. An alternative approach to reduce the risk of pneumothorax during erector spinae plane block in low thoracic vertebral levels. J Clin Anesth. 2020; 59:14–5.31. Macfarlane AJ, Gitman M, Bornstein KJ, El-Boghdadly K, Weinberg G. Updates in our understanding of local anaesthetic systemic toxicity: a narrative review. Anaesthesia. 2021; 76(Suppl 1):27–39.32. Apfel CC, Heidrich FM, Jukar-Rao S, Jalota L, Hornuss C, Whelan RP, et al. Evidence-based analysis of risk factors for postoperative nausea and vomiting. Br J Anaesth. 2012; 109:742–53.33. Lee DH, Song T, Kim KH, Lee KW. Incidence, natural course, and characteristics of postlaparoscopic shoulder pain. Surg Endosc. 2018; 32:160–5.34. Barazanchi AW, MacFater WS, Rahiri JL, Tutone S, Hill AG, Joshi GP, et al. Evidence-based management of pain after laparoscopic cholecystectomy: a PROSPECT review update. Br J Anaesth. 2018; 121:787–803.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erector spinae plane block for pediatric hip surgery: a case report
- Erector spinae plane block for spinal surgery: a systematic review and meta-analysis
- Anatomical classification and clinical application of thoracic paraspinal blocks
- Erector Spinae Plane Block in Patients with Low Back Pain
- Response to "Comment on Feasibility and efficacy of erector spinae plane block versus transversus abdominis plane block in laparoscopic bariatric surgery: a randomized comparative trial"