Korean J Gastroenterol.
2023 Apr;81(4):173-177. 10.4166/kjg.2023.030.
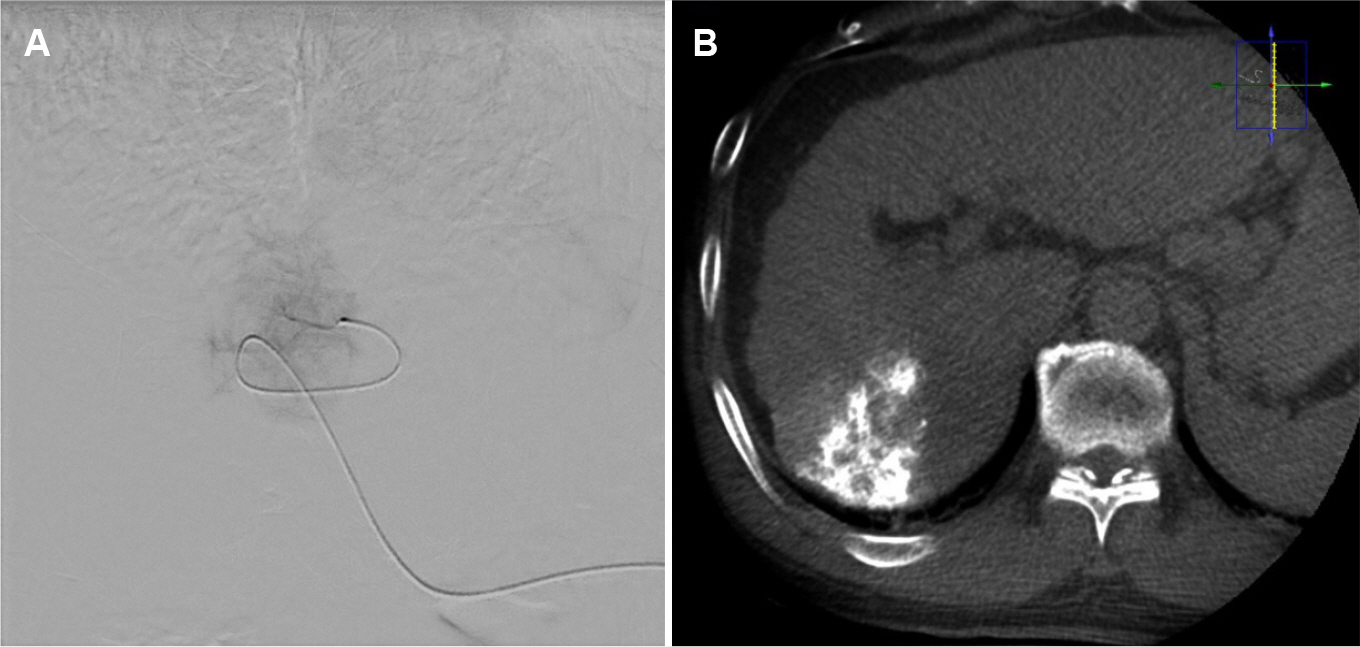
First Case of Atypical, Generalized Skin Rash after Transarterial Chemoembolization in a Patient with Hepatocellular Carcinoma
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Chonnam National University Hospital and Medical School, Gwangju, Korea
- 2Division of Gastroenterology, Departments of Radiology, Chonnam National University Hospital and Medical School, Gwangju, Korea
- 3Division of Gastroenterology, Departments of Dermatology, Chonnam National University Hospital and Medical School, Gwangju, Korea
- KMID: 2541780
- DOI: http://doi.org/10.4166/kjg.2023.030
Abstract
- Transarterial chemoembolization (TACE) is a widely used hepatocellular carcinoma (HCC) treatment. Some cases of supraumbilical skin rash after TACE in patients with HCC have been reported. To the best of the authors’ knowledge, there are no reports on atypical, generalized rashes caused by doxorubicin systemic absorption after TACE. This paper presents the case of a 64-year-old male with HCC who developed generalized macules and patches one day after a successful TACE procedure. A histology examination of a skin biopsy of a dark reddish patch on the knee revealed severe interface dermatitis. He was treated with a topical steroid, and all skin rashes improved within a week with no side effects. This report presents this rare case with a literature review on skin rash after TACE.
Keyword
Figure
Reference
-
1. Reig M, Forner A, Rimola J, et al. 2022; BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. J Hepatol. 76:681–693. DOI: 10.1016/j.jhep.2021.11.018. PMID: 34801630. PMCID: PMC8866082.2. Clark TW. 2006; Complications of hepatic chemoembolization. Semin Intervent Radiol. 23:119–125. DOI: 10.1055/s-2006-941442. PMID: 21326755. PMCID: PMC3036366.3. Kanzaki H, Nouso K, Miyahara K, et al. 2009; A case of hepatocellular carcinoma with skin injury of the upper abdominal wall after transcatheter arterial chemoembolization: a case report. Cases J. 2:7197. DOI: 10.4076/1757-1626-2-7197. PMID: 19918514. PMCID: PMC2769344.4. Lee E, Kim GM, Kim SY. 2009; Fixed drug eruption mimicking supraumbilical skin rash: one of rare complication of transarterial chemoembolization. J Eur Acad Dermatol Venereol. 23:324–325. DOI: 10.1111/j.1468-3083.2008.02863.x. PMID: 18631209.5. Byun JW, Han SH, Song HJ, et al. 2009; A case of supraumbilical skin rash after chemoembolization for hepatocellular carcinoma. J Eur Acad Dermatol Venereol. 23:1458–1459. DOI: 10.1111/j.1468-3083.2009.03252.x. PMID: 19453804.6. Hama Y, Iwasaki Y, Kusano S. 2000; Supraumbilical skin rash after chemoembolization for hepatocellular carcinoma. Eur Radiol. 10:1356. DOI: 10.1007/s003309900297. PMID: 10939508.7. Jang MS, Baek JW, Kang DY, Kang JS, Suh KS, Kim ST. 2011; Supraumbilical skin rash after transcatheter arterial chemoembolization: successful treatment with pentoxifylline. J Dermatol. 38:1188–1191. DOI: 10.1111/j.1346-8138.2011.01231.x. PMID: 21592200.8. Nagpal P, Bhalala M, Vidholia A, et al. 2016; Abdominal skin rash after TACE due to non-target embolization of hepatic falciform artery. ACG Case Rep J. 3:217–220. DOI: 10.14309/crj.2016.55. PMID: 27144210. PMCID: PMC4843162.9. Lin CC, Wu DK, Shih PM, Liu GC, Chuang WL. 2004; Supraumbilical skin rash and fat necrosis after transcatheter arterial chemoembolization: a case report. Kaohsiung J Med Sci. 20:36–40. DOI: 10.1016/S1607-551X(09)70082-8. PMID: 15481565.10. Kim HY, Bae SH, Park CH, et al. 2013; Supraumbilical subcutaneous fat necrosis after transcatheter arterial chemoembolization with drug-eluting beads: case report and review of the literature. Cardiovasc Intervent Radiol. 36:276–279. DOI: 10.1007/s00270-012-0356-6. PMID: 22382809.11. Marcacuzco Quinto A, Nutu OA, San Román Manso R, et al. 2018; Complications of transarterial chemoembolization (TACE) in the treatment of liver tumors. Cir Esp (Engl Ed). 96:560–567. English, Spanish. DOI: 10.1016/j.cireng.2018.10.017.12. Umemura T, Yamamura N, Nagata A, et al. 1998; Case report: Steatonecrosis in the upper abdomen following transcatheter arterial embolization for hepatocellular carcinoma. J Gastroenterol Hepatol. 13:471–474. DOI: 10.1111/j.1440-1746.1998.tb00670.x. PMID: 9641642.13. Brennan DD, Farrelly C, Cooney R, Norris S, McEniff N. 2005; Abdominal rash after transarterial chemoembolization via the right inferior phrenic artery. J Vasc Interv Radiol. 16:1269. DOI: 10.1097/01.RVI.0000179798.81815.60. PMID: 16151071.14. Grieshaber E, Nicotri T, Reina R, Rupley K, Wang A. 2014; Cutaneous embolization of doxorubicin drug-eluting beads. JAMA Dermatol. 150:1118–1120. DOI: 10.1001/jamadermatol.2014.305. PMID: 24989853.15. Elsayed AG, Martin JM, Pacioles T. 2018; Rash and subcutaneous fat necrosis after DEB-TACE with doxorubicin. BMJ Case Rep. 2018:bcr2017222394. DOI: 10.1136/bcr-2017-222394. PMID: 29305365. PMCID: PMC5775767.16. Kuan A, Khoo L, Yang SS, Chia HY, Lee JSS. 2020; Retiform purpura as a complication of microsphere emboli following transarterial chemoembolization for primary hepatocellular carcinoma: A case report and literature review. Am J Dermatopathol. 42:e108–e110. DOI: 10.1097/DAD.0000000000001586. PMID: 31809275.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of Hepatic Arterial Infusion Chemotherapy and Radiofrequency Ablation against Hepatocellular Carcinoma Refractory to Transarterial Chemoembolization and Vascular Variation: A Case Study
- Complications Related to Transarterial Treatment of Hepatocellular Carcinoma: A Comprehensive Review
- Supraumbilical Skin Rash as a Rare Complication of Transcatheter Arterial Chemoembolization in Patients with Hepatocellular Carcinoma
- Transarterial Chemoembolization in Patients with Hepatocellular Carcinoma and Extrahepatic Metastasis
- Rare Case of Pyogenic Brain Abscess after Transarterial Chemoembolization in a Patient with Hepatocellular Carcinoma: Case Report and Literature Review