Blood Res.
2023 Mar;58(1):61-70. 10.5045/br.2023.2022197.
Impact of ABO blood group antigens on residual factor VIII levels and risk of inhibitor development in hemophilia A
- Affiliations
-
- 1Department of Hematology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
- 2Department of Paediatrics, Postgraduate Institute of Medical Education and Research, Chandigarh, India
- 3Department of Internal Medicine, Postgraduate Institute of Medical Education and Research, Chandigarh, India
- KMID: 2541066
- DOI: http://doi.org/10.5045/br.2023.2022197
Abstract
- Background
The clinical phenotype of hemophilia A (HA) does not always correlate with severity. Similarly, the presence of inhibitors does not necessarily increase the risk of bleeding. This paradox between clinical and laboratory findings may be partially attributed to non-modifiable factors, such as blood group, which is known to influence FVIII levels in healthy individuals. Our aim was to assess the effect of ABO blood group antigens on FVIII levels across the severity spectrum of HA and risk of inhibitor development.
Methods
Data of consecutive patients with HA who visited the coagulation unit of a northern Indian tertiary care hospital between 2010‒2021 were reviewed. Patients with missing blood group data, transfusion histories, or baseline FVIII levels were excluded.
Results
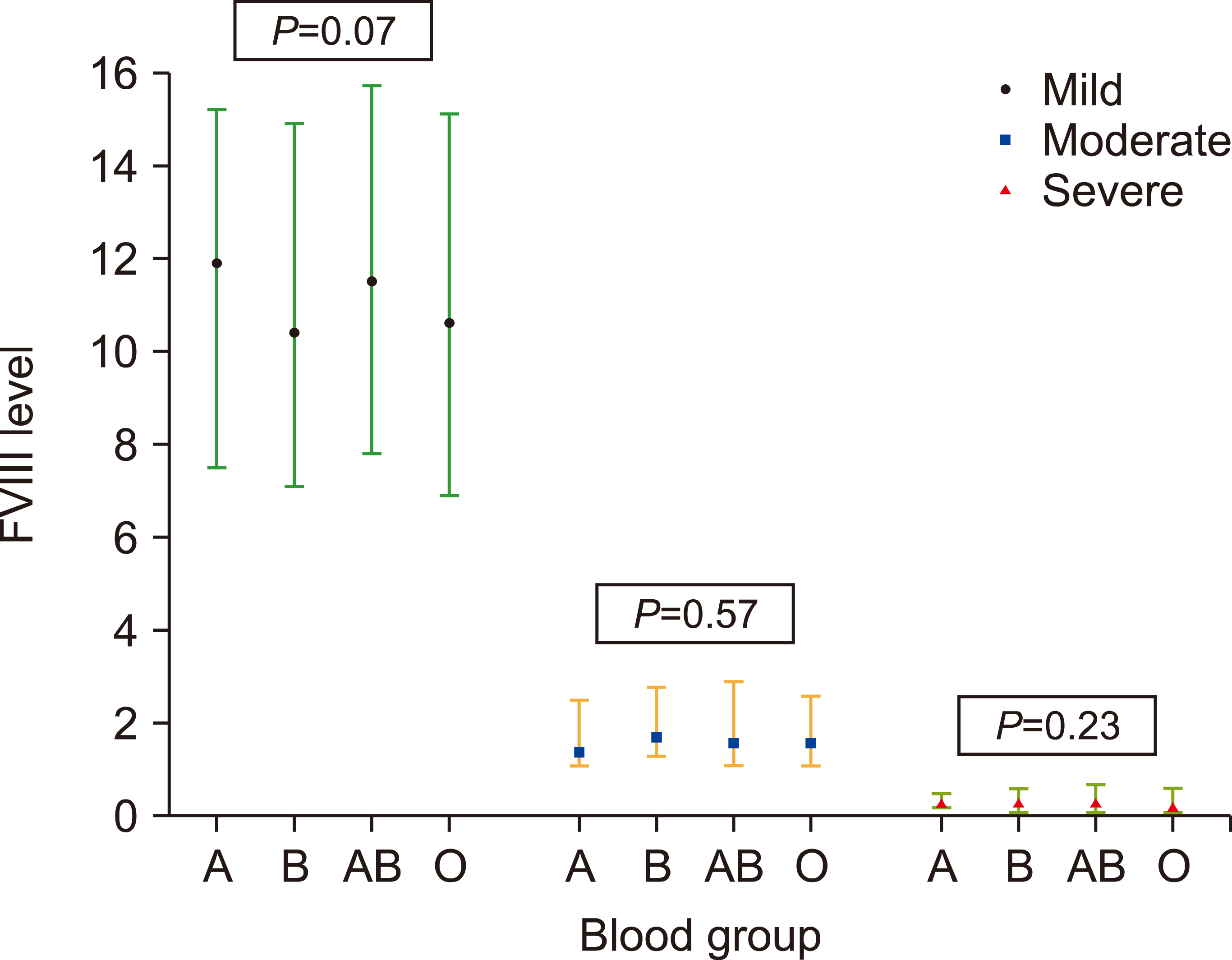
Mild, moderate, and severe HA was present in 41 (6.9%), 72 (12.2%), and 479 (80.9%) patients, respectively. There were no differences in the FVIII levels among the various blood groups across the HA severity spectrum. Inhibitors were administered to 35 patients (5.9%). In the multivariate analysis, blood group A was an independent risk factor for the development of inhibitors (adjusted odds ratio 2.70, P =0.04) after adjusting for age at onset of bleeding, FVIII transfusion, age at first FVIII transfusion, and severity of HA.
Conclusion
Unlike what is observed in healthy individuals, blood group did not influence residual FVIII levels across the severity spectrum of HA. Patients in group A had a higher risk of developing inhibitors.
Figure
Reference
-
1. Ewald DR, Sumner SC. 2016; Blood type biochemistry and human disease. Wiley Interdiscip Rev Syst Biol Med. 8:517–35. DOI: 10.1002/wsbm.1355. PMID: 27599872. PMCID: PMC5061611.
Article2. Liumbruno GM, Franchini M. 2013; Beyond immunohaematology: the role of the ABO blood group in human diseases. Blood Transfus. 11:491–9. DOI: 10.2450/2013.0152-13. PMID: 24120598. PMCID: PMC3827391.3. Wu O, Bayoumi N, Vickers MA, Clark P. 2008; ABO(H) blood groups and vascular disease: a systematic review and meta-analysis. J Thromb Haemost. 6:62–9. DOI: 10.1111/j.1538-7836.2007.02818.x. PMID: 17973651.4. Jenkins PV, O'Donnell JS. 2006; ABO blood group determines plasma von Willebrand factor levels: a biologic function after all? Transfusion. 46:1836–44. DOI: 10.1111/j.1537-2995.2006.00975.x. PMID: 17002642.5. Lenting PJ, Christophe OD, Denis CV. 2015; von Willebrand factor biosynthesis, secretion, and clearance: connecting the far ends. Blood. 125:2019–28. DOI: 10.1182/blood-2014-06-528406. PMID: 25712991.
Article6. Rejtő J, Königsbrügge O, Grilz E, et al. 2020; Influence of blood group, von Willebrand factor levels, and age on factor VIII levels in non-severe haemophilia A. J Thromb Haemost. 18:1081–6. DOI: 10.1111/jth.14770. PMID: 32073230. PMCID: PMC7318586.7. Loomans JI, van Velzen AS, Eckhardt CL, et al. 2017; Variation in baseline factor VIII concentration in a retrospective cohort of mild/moderate hemophilia A patients carrying identical F8 mutations. J Thromb Haemost. 15:246–54. DOI: 10.1111/jth.13581. PMID: 27943580.8. Srivastava A, Santagostino E, Dougall A, et al. 2020; WFH guidelines for the management of hemophilia, 3rd edition. Haemophilia . 26(Suppl 6):1–158. DOI: 10.1111/hae.14046. PMID: 32744769.
Article9. Franchini M, Coppola A, Santoro C, et al. 2021; ABO blood group and inhibitor risk in severe hemophilia A patients: a study from the Italian Association of Hemophilia Centers. Semin Thromb Hemost. 47:84–9. DOI: 10.1055/s-0040-1718870. PMID: 33525041.
Article10. Franchini M, Coppola A, Mengoli C, et al. 2017; Blood group O protects against inhibitor development in severe hemophilia A patients. Semin Thromb Hemost. 43:69–74. DOI: 10.1055/s-0036-1592166. PMID: 27825181.11. Arshad S, Singh A, Awasthi NP, Kumari S, Husain N. 2018; Clinicopathological parameters influencing inhibitor development in patients with hemophilia A receiving on-demand therapy. Ther Adv Hematol. 9:213–26. DOI: 10.1177/2040620718785363. PMID: 30181842. PMCID: PMC6116755.12. Desch KC. 2018; Regulation of plasma von Willebrand factor. F1000Res. 7:96. DOI: 10.12688/f1000research.13056.1. PMID: 29416854. PMCID: PMC5782404. PMID: 0234ff01d6e94056bd14507d01010b9d.13. Mehic D, Hofer S, Jungbauer C, et al. 2020; Association of ABO blood group with bleeding severity in patients with bleeding of unknown cause. Blood Adv. 4:5157–64. DOI: 10.1182/bloodadvances.2020002452. PMID: 33095871. PMCID: PMC7594405.14. Franchini M, Crestani S, Frattini F, Sissa C, Bonfanti C. 2014; ABO blood group and von Willebrand factor: biological implications. Clin Chem Lab Med. 52:1273–6. DOI: 10.1515/cclm-2014-0564. PMID: 24945431.15. Kepa S, Horvath B, Reitter-Pfoertner S, et al. 2015; Parameters influencing FVIII pharmacokinetics in patients with severe and moderate haemophilia A. Haemophilia. 21:343–50. DOI: 10.1111/hae.12592. PMID: 25582282.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Genetic Risk Factors of Hemophilia A
- An Autoplex Treatment in a Hemophilia A Patient with High Titer of Anticoagulant FVIII Antibody
- Acquired Hemophilia: Successfully Treated with Plasma Exchange in a Patient with Hightiter Inhibitors
- Laparoscopic Cholecystectomy in a Hemophiliac Patient with Factor VIII Inhibitor
- The prevalence and risk factors of inhibitor development of FVIII in previously treated patients with hemophilia A