Pediatr Emerg Med J.
2023 Apr;10(2):54-59. 10.22470/pemj.2022.00654.
Clinical characteristics of infants younger than 90 days diagnosed with invasive group B streptococcal infection in the emergency department
- Affiliations
-
- 1Department of Emergency Medicine, Ulsan University Hospital, Ulsan, Republic of Korea
- 2Department of Pediatrics, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Republic of Korea
- KMID: 2540909
- DOI: http://doi.org/10.22470/pemj.2022.00654
Abstract
- Purpose
We aimed to characterize invasive group B streptococcal infection (IGBSI) in young infants hospitalized through the emergency department.
Methods
We analyzed medical records of infants younger than 90 days with IGBSI, defined as group B streptococcus bacteremia or meningitis, who visited the emergency department from January 2009 through December 2021. Their clinical features were compared as per 2 criteria, neonates and meningitis. For the comparisons, we defined 2 composite outcomes, “clinically important abnormality (any of the followings: temperature > 38.5℃, leukocytes < 5,000/mm3 or > 15,000/mm3, absolute neutrophils > 4,000/mm3 or C-reactive protein > 2.0 mg/dL)”and “poor outcomes (any of the followings: intensive care unit, transfer, seizure or complications).”Percentages are rounded to the first decimal places.
Results
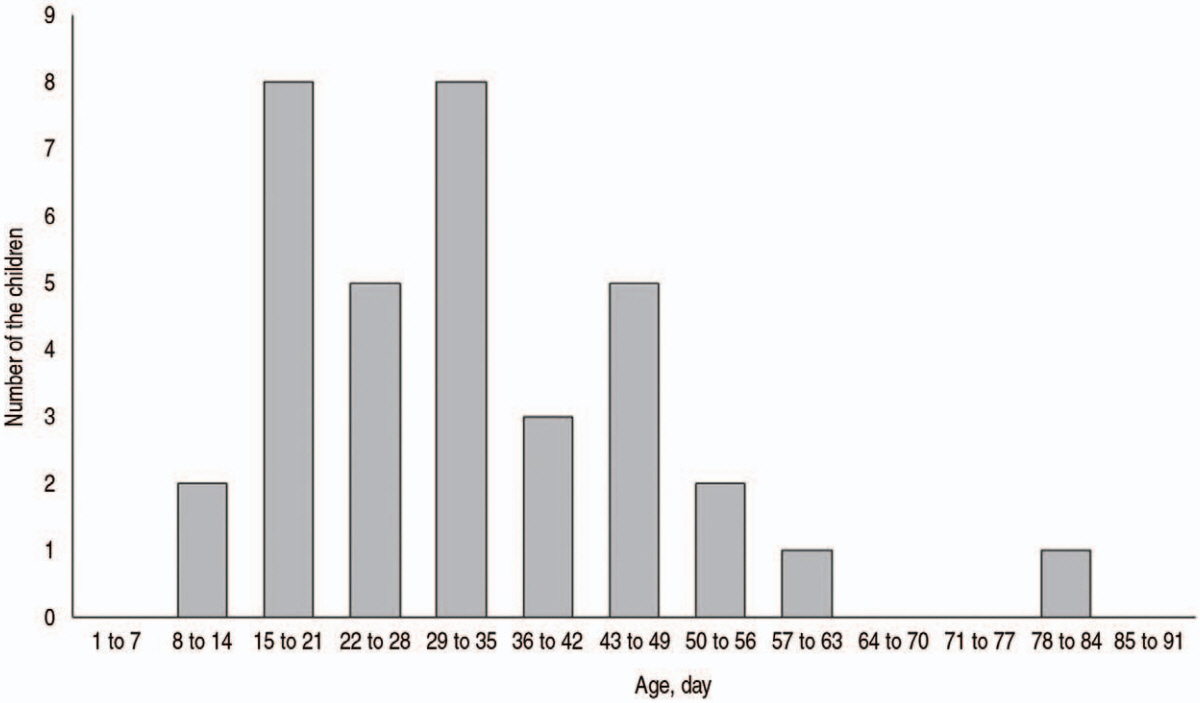
A total of 35 infants, of whom 15 (43%) were neonates and 17 (49%) were boys, had IGBSIs, including 23 infants (66%) with isolated bacteremia, 11 (31%) with bacteremia with meningitis, and 1 (3%) with isolated meningitis. Ill appearances were noted in 27 infants (77%) who encompassed all with meningitis. The other 8 infants (23%) looking well had 1 or more components of the clinically important abnormality. The neonates showed a higher frequency of vaginal delivery (87% vs. 35%; P = 0.002) and a lower frequency of a temperature > 38.5℃, compared to their counterparts (47% vs. 80%; P = 0.040). The infants with meningitis had a longer median time required to visit (5.0 vs. 2.0 hours; P = 0.011), and higher frequencies of ill appearance (100% vs. 65%; P = 0.032), leukocytes < 5,000/mm3 (67% vs. 13%; P = 0.002), and the poor outcomes (75% vs. 0%; P < 0.001).
Conclusion
Young infants with ill-looking appearance or abnormality in any of the fever or inflammatory markers may have IGBSIs, particularly meningitis.
Keyword
Figure
Reference
-
References
1. Woll C, Neuman MI, Pruitt CM, Wang ME, Shapiro ED, Shah SS, et al. Epidemiology and etiology of invasive bacterial infection in infants ≤ 60 days old treated in emergency departments. J Pediatr. 2018; 200:210–7.2. Powell EC, Mahajan PV, Roosevelt G, Hoyle JD Jr, Gattu R, Cruz AT, et al. Epidemiology of bacteremia in febrile infants aged 60 days and younger. Ann Emerg Med. 2018; 71:211–6.3. Rhie K, Choi EH, Cho EY, Lee J, Kang JH, Kim DS, et al. Etiology of invasive bacterial infections in immunocompetent children in Korea (2006-2010): a retrospective multicenter study. J Korean Med Sci. 2018; 33:e45.4. Park KH, Kim KH, Kang JH, Kim KN, Kim DS, Kim YK, et al. Current status and clinical presentations of invasive neonatal Group B streptococcal infections in Korea. Pediatr Int. 2011; 53:236–9.5. Goldstein B, Giroir B, Randolph A; International Consensus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005; 6:2–8.6. Pantell RH, Roberts KB, Adams WG, Dreyer BP, Kuppermann N, O’Leary ST, et al. Evaluation and management of wellappearing febrile infants 8 to 60 days old. Pediatrics. 2021; 148:e2021052228.7. Kestenbaum LA, Ebberson J, Zorc JJ, Hodinka RL, Shah SS. Defining cerebrospinal fluid white blood cell count reference values in neonates and young infants. Pediatrics. 2010; 125:257–64.8. Dieckmann RA, Brownstein D, Gausche-Hill M. The pediatric assessment triangle: a novel approach for the rapid evaluation of children. Pediatr Emerg Care. 2010; 26:312–5.9. Gomez B, Mintegi S, Bressan S, Da Dalt L, Gervaix A, Lacroix L, et al. Validation of the “step-by-step” approach in the management of young febrile infants. Pediatrics. 2016; 138:e20154381.10. Fernández A, Ares MI, Garcia S, Martinez-Indart L, Mintegi S, Benito J. The validity of the pediatric assessment triangle as the first step in the triage process in a pediatric emergency department. Pediatr Emerg Care. 2017; 33:234–8.11. Woll C, Neuman MI, Aronson PL. Management of the febrile young infant: update for the 21st Century. Pediatr Emerg Care. 2017; 33:748–53.12. Ecclesia FG, Alonso Cadenas JA, Gómez B, Gangoiti I, Hernández-Bou S, de la Torre Espí M, et al. Late-onset group B streptococcus bacteremia evaluated in the pediatric emergency department and risk factors for severe infection. Pediatr Infect Dis J. 2022; 41:455–9.13. Michelson KA, Neuman MI, Pruitt CM, Desai S, Wang ME, DePorre AG, et al. Height of fever and invasive bacterial infection. Arch Dis Child. 2021; 106:594–6.14. de la Torre M, Gómez B, Velasco R; Group for Study of Febrile Infant of Spanish Pediatric Emergency Research Group (RISeuP-SPERG). Value of temperature for predicting invasive bacterial infection in febrile infants: a Spanish Pediatric Emergency Research Group (RISeuP-SPERG) study. Pediatr Emerg Care. 2022; 38:e1294–7.15. Madrid L, Seale AC, Kohli-Lynch M, Edmond KM, Lawn JE, Heath PT, et al. Infant group B streptococcal disease incidence and serotypes worldwide: systematic review and meta-analyses. Clin Infect Dis. 2017; 65(Suppl 2):S160–72.16. Tibussek D, Sinclair A, Yau I, Teatero S, Fittipaldi N, Richardson SE, et al. Late-onset group B streptococcal meningitis has cerebrovascular complications. J Pediatr. 2015; 166:1187–92.17. Choi SY, Kim JW, Ko JW, Lee YS, Chang YP. Patterns of ischemic injury on brain images in neonatal group B Streptococcal meningitis. Korean J Pediatr. 2018; 61:245–52.18. Bedford H, de Louvois J, Halket S, Peckham C, Hurley R, Harvey D. Meningitis in infancy in England and Wales: follow up at age 5 years. BMJ. 2001; 323:533–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical study of group B streptococcal infection in infants less than two months of age
- Usefulness of Low-Risk Criteria for Serious Bacterial Infections in Febrile Infants Younger than 90 Days of Age
- Characteristics of Meningitis in Febrile Infants Aged ≤90 Days
- Retrospective validation of the Step-by-Step approach for febrile infants younger than 90 days in the emergency department
- A Comparison of Clinical Characteristics between Adenoviral and Group A Streptococcal Pharyngitis in Children