Clin Endosc.
2023 Mar;56(2):169-179. 10.5946/ce.2022.282.
Influence of biliary stents on the diagnostic outcome of endoscopic ultrasound–guided tissue acquisition from solid pancreatic lesions: a systematic review and meta-analysis
- Affiliations
-
- 1Department of Gastroenterology, Nizam’s Institute of Medical Sciences, Hyderabad, India
- 2Institute of Gastrosciences and Liver, Apollo Multispecialty Hospital, Kolkata, India
- 3Department of Gastroenterology, KM Cherian Institute of Medical Sciences, Kallissery, India
- 4Department of Digestive Disease and Clinical Nutrition, Tata Memorial Hospital, Mumbai, India
- KMID: 2540732
- DOI: http://doi.org/10.5946/ce.2022.282
Abstract
- Background/Aims
This meta-analysis analyzed the effect of an indwelling biliary stent on endoscopic ultrasound (EUS)–guided tissue acquisition from pancreatic lesions.
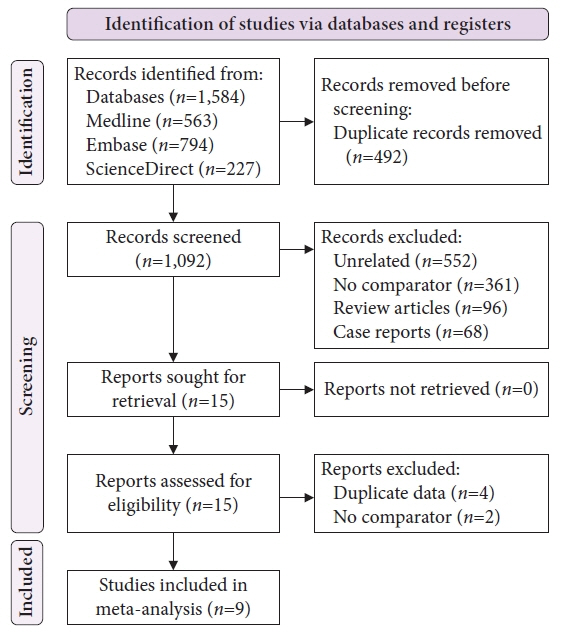
Methods
A literature search was performed to identify studies published between 2000 and July 2022 comparing the diagnostic outcomes of EUS-TA in patients with or without biliary stents. For non-strict criteria, samples reported as malignant or suspicious for malignancy were included, whereas for strict criteria, only samples reported as malignant were included in the analysis.
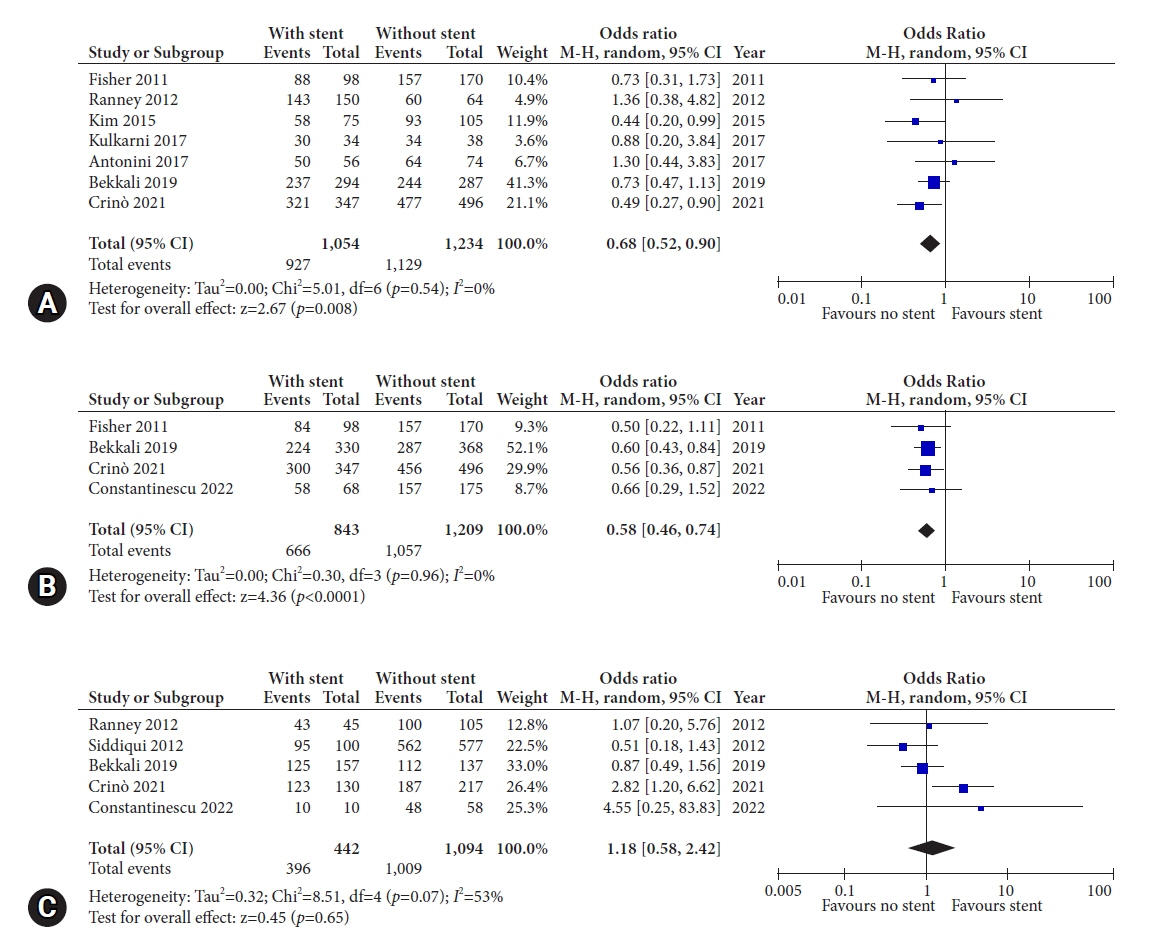
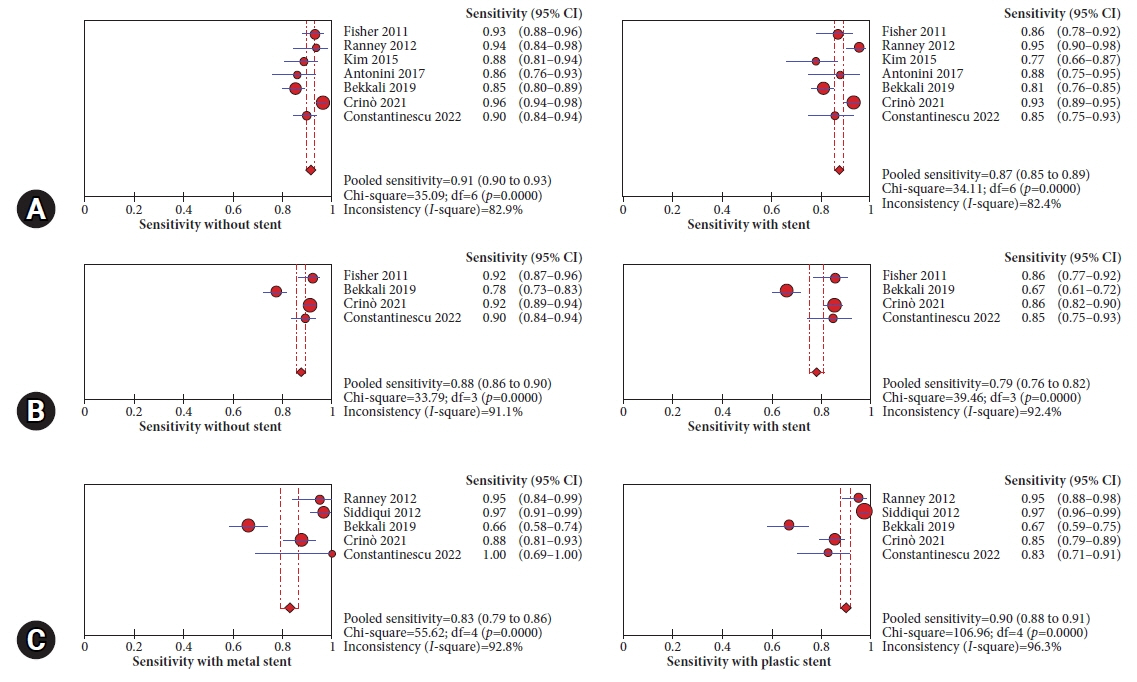
Results
Nine studies were included in this analysis. The odds of an accurate diagnosis were significantly lower in patients with indwelling stents using both non-strict (odds ratio [OR], 0.68; 95% confidence interval [CI], 0.52–0.90) and strict criteria (OR, 0.58; 95% CI, 0.46–0.74). The pooled sensitivity with and without stents were similar (87% vs. 91%) using non-strict criteria. However, patients with stents had a lower pooled sensitivity (79% vs. 88%) when using strict criteria. The sample inadequacy rate was comparable between groups (OR, 1.12; 95% CI, 0.76–1.65). The diagnostic accuracy and sample inadequacy were comparable between plastic and metal biliary stents.
Conclusions
The presence of a biliary stent may negatively affect the diagnostic outcome of EUS-TA for pancreatic lesions.
Figure
Reference
-
1. Guarneri G, Gasparini G, Crippa S, et al. Diagnostic strategy with a solid pancreatic mass. Presse Med. 2019; 48(3 Pt 2):e125–e145.2. Dietrich CF, Jenssen C. Modern ultrasound imaging of pancreatic tumors. Ultrasonography. 2020; 39:105–113.3. Dewitt J, Devereaux BM, Lehman GA, et al. Comparison of endoscopic ultrasound and computed tomography for the preoperative evaluation of pancreatic cancer: a systematic review. Clin Gastroenterol Hepatol. 2006; 4:717–725.4. Gomes RM, Bal M, Patkar S, et al. Unexpected benign histopathology after pancreatoduodenectomy for presumed malignancy: accepting the inevitable. Langenbecks Arch Surg. 2016; 401:169–179.5. Manzia TM, Toti L, Lenci I, et al. Benign disease and unexpected histological findings after pancreaticoduodenectomy: the role of endoscopic ultrasound fine needle aspiration. Ann R Coll Surg Engl. 2010; 92:295–301.6. Asbun HJ, Conlon K, Fernandez-Cruz L, et al. When to perform a pancreatoduodenectomy in the absence of positive histology?: a consensus statement by the International Study Group of Pancreatic Surgery. Surgery. 2014; 155:887–892.7. Banafea O, Mghanga FP, Zhao J, et al. Endoscopic ultrasonography with fine-needle aspiration for histological diagnosis of solid pancreatic masses: a meta-analysis of diagnostic accuracy studies. BMC Gastroenterol. 2016; 16:108.8. Micames C, Jowell PS, White R, et al. Lower frequency of peritoneal carcinomatosis in patients with pancreatic cancer diagnosed by EUS-guided FNA vs. percutaneous FNA. Gastrointest Endosc. 2003; 58:690–695.9. Ross WA, Wasan SM, Evans DB, et al. Combined EUS with FNA and ERCP for the evaluation of patients with obstructive jaundice from presumed pancreatic malignancy. Gastrointest Endosc. 2008; 68:461–466.10. Gardner TB, Gordon SR. Combined EUS with FNA and ERCP for the evaluation of pancreatic adenocarcinoma in the very elderly. Gastrointest Endosc. 2009; 69:AB250.11. Cannon ME, Carpenter SL, Elta GH, et al. EUS compared with CT, magnetic resonance imaging, and angiography and the influence of biliary stenting on staging accuracy of ampullary neoplasms. Gastrointest Endosc. 1999; 50:27–33.12. Chen CH, Tseng LJ, Yang CC, et al. Preoperative evaluation of periampullary tumors by endoscopic sonography, transabdominal sonography, and computed tomography. J Clin Ultrasound. 2001; 29:313–321.13. Fusaroli P, Manta R, Fedeli P, et al. The influence of endoscopic biliary stents on the accuracy of endoscopic ultrasound for pancreatic head cancer staging. Endoscopy. 2007; 39:813–817.14. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021; 372:n71.15. Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011; 343:d5928.16. Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016; 355:i4919.17. Fisher JM, Gordon SR, Gardner TB. The impact of prior biliary stenting on the accuracy and complication rate of endoscopic ultrasound fine-needle aspiration for diagnosing pancreatic adenocarcinoma. Pancreas. 2011; 40:21–24.18. Ranney N, Phadnis M, Trevino J, et al. Impact of biliary stents on EUS-guided FNA of pancreatic mass lesions. Gastrointest Endosc. 2012; 76:76–83.19. Siddiqui AA, Fein M, Kowalski TE, et al. Comparison of the influence of plastic and fully covered metal biliary stents on the accuracy of EUS-FNA for the diagnosis of pancreatic cancer. Dig Dis Sci. 2012; 57:2438–2445.20. Kim JJ, Walia S, Lee SH, et al. Lower yield of endoscopic ultrasound-guided fine-needle aspiration in patients with pancreatic head mass with a biliary stent. Dig Dis Sci. 2015; 60:543–549.21. Antonini F, Fuccio L, Giorgini S, et al. Biliary plastic stent does not influence the accuracy of endoscopic ultrasound-guided sampling of pancreatic head masses performed with core biopsy needles. Dig Liver Dis. 2017; 49:898–902.22. Kulkarni AA, Singh S, Rao B, et al. Presence of an indwelling biliary stent in patients with pancreatic head masses: does it impact endoscopic ultrasound evaluation? Gastrointest Endosc. 2017; 85:AB439.23. Bekkali NL, Nayar MK, Leeds JS, et al. Impact of metal and plastic stents on endoscopic ultrasound-guided aspiration cytology and core histology of head of pancreas masses. Endoscopy. 2019; 51:1044–1050.24. Crinò SF, Conti Bellocchi MC, Antonini F, et al. Impact of biliary stents on the diagnostic accuracy of EUS-guided fine-needle biopsy of solid pancreatic head lesions: a multicenter study. Endosc Ultrasound. 2021; 10:440–447.25. Constantinescu A, Plotogea OM, Stan-Ilie M, et al. Impact of biliary stenting in endoscopic ultrasound-guided tissue acquisition among patients with pancreatic cancer. J Clin Ultrasound. 2022; 50:844–849.26. Bao PQ, Johnson JC, Lindsey EH, et al. Endoscopic ultrasound and computed tomography predictors of pancreatic cancer resectability. J Gastrointest Surg. 2008; 12:10–16.27. Nakai Y, Isayama H, Wang HP, et al. International consensus statements for endoscopic management of distal biliary stricture. J Gastroenterol Hepatol. 2020; 35:967–979.28. Arya N, Wyse JM, Jayaraman S, et al. A proposal for the ideal algorithm for the diagnosis, staging, and treatment of pancreas masses suspicious for pancreatic adenocarcinoma: results of a working group of the Canadian Society for Endoscopic Ultrasound. Endosc Ultrasound. 2020; 9:154–161.29. Polkowski M, Jenssen C, Kaye P, et al. Technical aspects of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Technical Guideline: March 2017. Endoscopy. 2017; 49:989–1006.30. Kamata K, Kitano M, Yasukawa S, et al. Histologic diagnosis of pancreatic masses using 25-gauge endoscopic ultrasound needles with and without a core trap: a multicenter randomized trial. Endoscopy. 2016; 48:632–638.31. Gimeno-García AZ, Elwassief A, Paquin SC, et al. Randomized controlled trial comparing stylet-free endoscopic ultrasound-guided fine-needle aspiration with 22-G and 25-G needles. Dig Endosc. 2014; 26:467–473.32. Fabbri C, Polifemo AM, Luigiano C, et al. Endoscopic ultrasound-guided fine needle aspiration with 22- and 25-gauge needles in solid pancreatic masses: a prospective comparative study with randomisation of needle sequence. Dig Liver Dis. 2011; 43:647–652.33. Oppong KW, Nayar MK, Bekkali NL, et al. Impact of prior biliary stenting on diagnostic performance of endoscopic ultrasound for mesenteric vascular staging in patients with head of pancreas and periampullary malignancy. BMJ Open Gastroenterol. 2022; 9:e000864.34. Ignee A, Jenssen C, Arcidiacono PG, et al. Endoscopic ultrasound elastography of small solid pancreatic lesions: a multicenter study. Endoscopy. 2018; 50:1071–1079.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic ultrasound-guided tissue acquisition: Needle types, technical issues, and sample handling
- Technical Advances in Endoscopic Ultrasound (EUS)-Guided Tissue Acquisition for Pancreatic Cancers: How Can We Get the Best Results with EUS-Guided Fine Needle Aspiration?
- Present and Future of Endoscopic Ultrasound-Guided Tissue Acquisition in Solid Pancreatic Tumors
- How to optimize the diagnostic yield of endoscopic ultrasoundguided fine-needle sampling in solid pancreatic lesions from a technical perspective
- Endoscopic Ultrasound-Guided Fine Needle Biopsy Needles Provide Higher Diagnostic Yield Compared to Endoscopic Ultrasound-Guided Fine Needle Aspiration Needles When Sampling Solid Pancreatic Lesions: A Meta-Analysis