Korean Circ J.
2023 Mar;53(3):170-184. 10.4070/kcj.2022.0252.
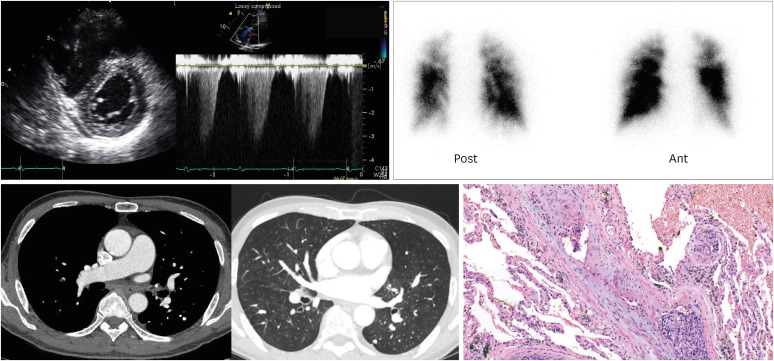
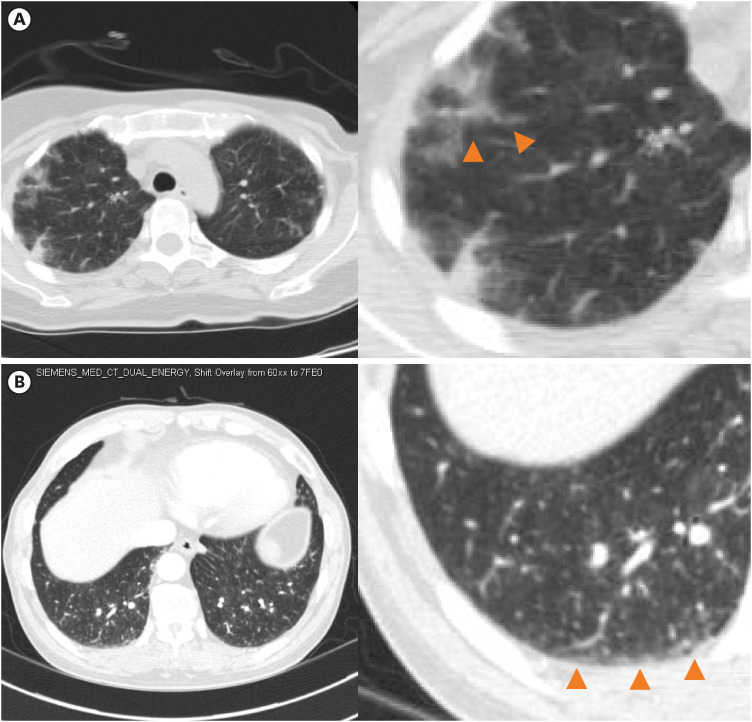
Clinical Course of Suspected Diagnosis of Pulmonary Tumor Thrombotic Microangiopathy: A 10-Year Experience of Rapid Progressive Right Ventricular Failure Syndrome in Advanced Cancer Patients
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Pathology and Translational Genomics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2540395
- DOI: http://doi.org/10.4070/kcj.2022.0252
Abstract
- Background and Objectives
Several cases involving severe right ventricular (RV) failure in advanced cancer patients have been found to be pulmonary tumor thrombotic microangiopathies (PTTMs). This study aimed to discover the nature of rapid RV failure syndrome with a suspected diagnosis of PTTM for better diagnosis, treatment, and prognosis prediction in clinical practice.
Methods
From 2011 to 2021, all patients with clinically suspected PTTM were derived from the one tertiary cancer hospital with more than 2000 in-hospital bed.
Results
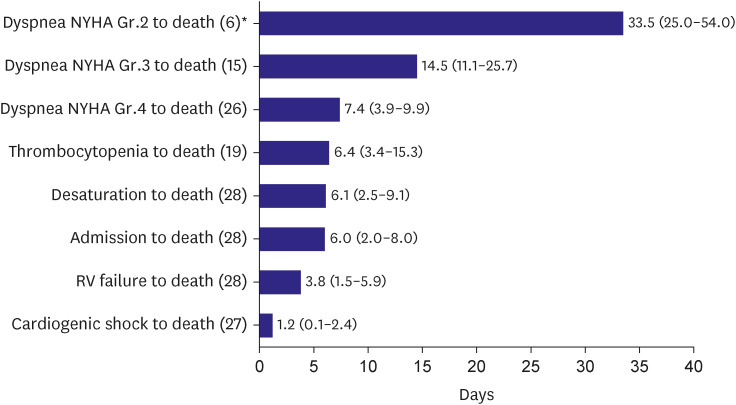
A total of 28 cases of clinically suspected PTTM with one biopsy confirmed case were included. The most common cancer types were breast (9/28, 32%) and the most common tissue type was adenocarcinoma (22/26, 85%). The time interval from dyspnea New York Heart Association (NYHA) Grade 2, 3, 4 to death, thrombocytopenia to death, desaturation to death, admission to death, RV failure to death, cardiogenic shock to death were 33.5 days, 14.5 days, 7.4 days, 6.4 days, 6.1 days, 6.0 days, 3.8 days and 1.2 days, respectively. The NYHA Grade 4 to death time was 7 days longer in those who received chemotherapy (7.1 days vs. 13.8 days, p value=0.030). However, anticoagulation, vasopressors or intensive care could not change clinical course.
Conclusions
Rapid RV failure syndrome with a suspected diagnosis of PTTM showed a rapid progressive course from symptom onset to death. Although chemotherapy was effective, increased life survival was negligible, and treatments other than chemotherapy did not help to improve the patient’s prognosis.
Keyword
Figure
Reference
-
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424. PMID: 30207593.2. Timp JF, Braekkan SK, Versteeg HH, Cannegieter SC. Epidemiology of cancer-associated venous thrombosis. Blood. 2013; 122:1712–1723. PMID: 23908465.3. Lyman GH, Culakova E, Poniewierski MS, Kuderer NM. Morbidity, mortality and costs associated with venous thromboembolism in hospitalized patients with cancer. Thromb Res. 2018; 164(Suppl 1):S112–S118. PMID: 29703467.4. Kane RD, Hawkins HK, Miller JA, Noce PS. Microscopic pulmonary tumor emboli associated with dyspnea. Cancer. 1975; 36:1473–1482. PMID: 1175142.5. Gonzalez-Vitale JC, Garcia-Bunuel R. Pulmonary tumor emboli and cor pulmonale in primary carcinoma of the lung. Cancer. 1976; 38:2105–2110. PMID: 991123.6. von Herbay A, Illes A, Waldherr R, Otto HF. Pulmonary tumor thrombotic microangiopathy with pulmonary hypertension. Cancer. 1990; 66:587–592. PMID: 2163747.7. Shiraiwa Y, Taniguchi Y, Hyoudou M, et al. A case of pulmonary tumor thrombotic microangiopathy following lymphedema on the lower extremities. Respir Med Case Rep. 2022; 37:101631. PMID: 35342709.8. Kamidani R, Kumada K, Okada H, et al. Postmortem diagnosis of pulmonary tumor thrombotic microangiopathy with rapid exacerbation in a patient with gastric cancer: a case report. Int J Emerg Med. 2021; 14:53. PMID: 34525938.9. Kawakami N, Moriya T, Kato R, et al. Pulmonary tumor thrombotic microangiopathy in occult early gastric cancer that was undetectable on upper endoscopy: a case report and review of similar cases. BMC Gastroenterol. 2021; 21:423. PMID: 34758740.10. Taylor FB Jr, Toh CH, Hoots WK, Wada H, Levi M. Scientific Subcommittee on Disseminated Intravascular Coagulation (DIC) of the International Society on Thrombosis and Haemostasis (ISTH). Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost. 2001; 86:1327–1330. PMID: 11816725.11. Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010; 23:685–713. PMID: 20620859.12. Miyano S, Izumi S, Takeda Y, et al. Pulmonary tumor thrombotic microangiopathy. J Clin Oncol. 2007; 25:597–599. PMID: 17290069.13. Kayatani H, Matsuo K, Ueda Y, et al. Pulmonary tumor thrombotic microangiopathy diagnosed antemortem and treated with combination chemotherapy. Intern Med. 2012; 51:2767–2770. PMID: 23037471.14. Imakura T, Tezuka T, Inayama M, et al. A long-term survival case of pulmonary tumor thrombotic microangiopathy due to gastric cancer confirmed by the early diagnosis based on a transbronchial lung biopsy. Intern Med. 2020; 59:1621–1627. PMID: 32612065.15. Kitamura A, Nishimura N, Jinta T, et al. A case of pulmonary tumor thrombotic microangiopathy diagnosed by transbronchial lung biopsy and treated with chemotherapy and long-term oxygen and anticoagulation therapies. Case Rep Pulmonol. 2013; 2013:259080. PMID: 24069542.16. Fujishiro T, Shuto K, Shiratori T, et al. A case report of pulmonary tumor thrombotic microangiopathy (PTTM) caused by esophageal squamous cell carcinoma. Esophagus. 2013; 10:247–251. PMID: 24319402.17. Uruga H, Fujii T, Kurosaki A, et al. Pulmonary tumor thrombotic microangiopathy: a clinical analysis of 30 autopsy cases. Intern Med. 2013; 52:1317–1323. PMID: 23774540.18. Godbole R, Saggar R, Zider A, et al. Insights on pulmonary tumor thrombotic microangiopathy: a seven-patient case series. Pulm Circ. 2017; 7:813–820. PMID: 28782988.19. Kuwabara H, Yoshida S, Takasu T, et al. Pulmonary tumor thrombotic microangiopathy caused by gastric cancer. Ann Thorac Med. 2012; 7:168–169. PMID: 22924078.20. Godbole RH, Saggar R, Kamangar N. Pulmonary tumor thrombotic microangiopathy: a systematic review. Pulm Circ. 2019; 9:2045894019851000. PMID: 31032740.21. Yao DX, Flieder DB, Hoda SA. Pulmonary tumor thrombotic microangiopathy: an often missed antemortem diagnosis. Arch Pathol Lab Med. 2001; 125:304–305. PMID: 11175660.22. Chinen K, Kazumoto T, Ohkura Y, Matsubara O, Tsuchiya E. Pulmonary tumor thrombotic microangiopathy caused by a gastric carcinoma expressing vascular endothelial growth factor and tissue factor. Pathol Int. 2005; 55:27–31. PMID: 15660700.23. Kagata Y, Nakanishi K, Ozeki Y, Terahata S, Matsubara O. An immunohistochemical study of tumor thrombotic microangiopathy: the role of TF, FGF and VEGF. J Jpn Coll Angiol. 2003; 43:679–684.24. Frazier AA, Galvin JR, Franks TJ, Rosado-De-Christenson ML. From the archives of the AFIP: pulmonary vasculature: hypertension and infarction. Radiographics. 2000; 20:491–524. PMID: 10715347.25. Franquet T, Giménez A, Prats R, Rodríguez-Arias JM, Rodríguez C. Thrombotic microangiopathy of pulmonary tumors: a vascular cause of tree-in-bud pattern on CT. AJR Am J Roentgenol. 2002; 179:897–899. PMID: 12239033.26. Rossi SE, Franquet T, Volpacchio M, Giménez A, Aguilar G. Tree-in-bud pattern at thin-section CT of the lungs: radiologic-pathologic overview. Radiographics. 2005; 25:789–801. PMID: 15888626.27. He H, Stein MW, Zalta B, Haramati LB. Pulmonary infarction: spectrum of findings on multidetector helical CT. J Thorac Imaging. 2006; 21:1–7. PMID: 16538148.28. Galiè N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Rev Esp Cardiol (Engl Ed). 2016; 69:177. PMID: 26837729.29. Wahl SG, Karlsen J, Schulz B, Johansen H, Abusland AB. Former cancer patient in her 40s with chest pain and increasing dyspnoea. Tidsskr Nor Laegeforen. 2012; 132:1877–1880. PMID: 22986975.30. Mandaliya R, Farhat S, Uprety D, et al. Occult gastric cancer presenting as hypoxia from pulmonary tumor thrombotic microangiopathy. J Gastric Cancer. 2014; 14:142–146. PMID: 25061544.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fatal progressive right heart failure in a pancreatic cancer patient
- A Case of Locally Advanced Breast Cancer Complicated by Pulmonary Tumor Thrombotic Microangiopathy
- Pulmonary Tumor Thrombotic Microangiopathy Associated with Advanced Gastric Cancer Successfully Treated with Chemotherapy
- A Case of Pulmonary Tumor Thrombotic Microangiopathy in a Patient with Advanced Gastric Cancer
- A Case Report: Cavitary Infarction Caused by Pulmonary Tumor Thrombotic Microangiopathy in a Patient with Pancreatic Intraductal Papillary Mucinous Neoplasm