J Korean Neurosurg Soc.
2023 Mar;66(2):144-154. 10.3340/jkns.2022.0120.
Recanalization Rate and Clinical Outcomes of Intravenous Tissue Plasminogen Activator Administration for Large Vessel Occlusion Stroke Patients
- Affiliations
-
- 1Department of Neurosurgery, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Neurosurgery, Bucheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2539875
- DOI: http://doi.org/10.3340/jkns.2022.0120
Abstract
Objective
: Stroke caused from large vessel occlusion (LVO) has emerged as the most common stroke subtype worldwide. Intravenous tissue plasminogen activator administration (IV-tPA) and additional intraarterial thrombectomy (IA-Tx) is regarded as standard treatment. In this study, the authors try to find the early recanalization rate of IV-tPA in LVO stroke patients.
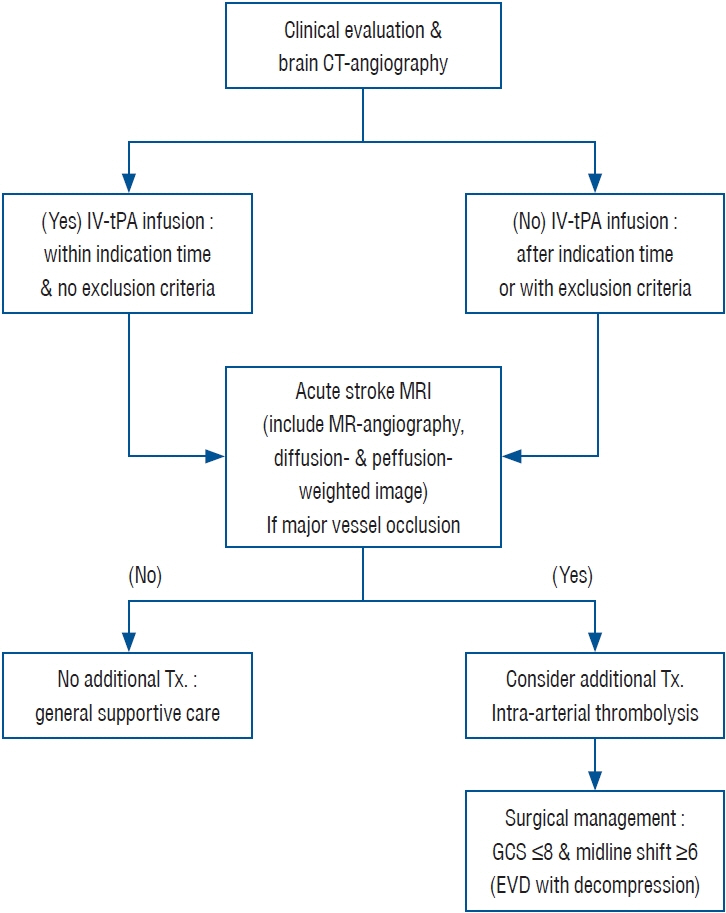
Methods
: Total 300 patients undertook IA-Tx with confirmed anterior circulation LVO, were analyzed retrospectively. Brain computed tomography angiography (CTA) was the initial imaging study and acute stroke magnetic resonance angiography (MRA) followed after finished IV-tPA. Early recanalization rate was evaluated by acute stroke MRA within 2 hours after the IV-tPA. In 167 patients undertook IV-tPA only and 133 non-recanalized patients by IV-tPA, additional IA-Tx tried (IV-tPA + IA-Tx group). And 131 patients, non-recanalized by IV-tPA (IV-tPA group) additional IA-Tx recommend and tried according to the patient condition and compliance.
Results
: Early recanalization rate of LVO after IV-tPA was 12.0% (36/300). In recanalized patients, favorable outcome (modified Rankin Scale, 0–2) was 69.4% (25/36) while it was 32.1% (42/131, p<0.001) in non-recanalized patients. Among 133 patients, nonrecanalized after intravenous recombinant tissue plasminogen activator and undertook additional IA-Tx, the clinical outcome was better than not undertaken additional IA-Tx (favorable outcome was 42.9% vs. 32.1%, p=0.046). Analysis according to the perfusion/diffusion (P/D)-mismatching or not, in patient with IV-tPA with IA-Tx (133 patients), favorable outcome was higher in P/ D-mismatching patient (52/104; 50.0%) than P/D-matching patients (5/29; 17.2%; p=0.001). Which treatment tired, P/D-mismatching was favored in clinical outcome (iv-tPA only, p=0.008 and IV-tPA with IA-Tx, p=0.001).
Conclusion
: The P/D-mismatching influences on the recanalization and clinical outcomes of IV-tPA and IA-Tx. The authors would like to propose that we had better prepare IA-Tx when LVO is diagnosed on initial diagnostic imaging. Furthermore, if the patient shows P/D-mismatching on MRA after IV-tPA, additional IA-Tx improves treatment results and lessen the futile recanalization.
Keyword
Figure
Reference
-
References
1. Abe O, Aoki S, Shirouzu I, Kunimatsu A, Hayashi N, Masumoto T, et al. MR imaging of ischemic penumbra. Eur J Radiol. 46:67–78. 2003.2. Albers GW, Thijs VN, Wechsler L, Kemp S, Schlaug G, Skalabrin E, et al. Magnetic resonance imaging profiles predict clinical response to early reperfusion: the diffusion and perfusion imaging evaluation for understanding stroke evolution (DEFUSE) study. Ann Neurol. 60:508–517. 2006.3. Aoki J, Kimura K, Shibazaki K, Sakamoto Y. DWI-ASPECTS as a predictor of dramatic recovery after intravenous recombinant tissue plasminogen activator administration in patients with middle cerebral artery occlusion. Stroke. 44:534–537. 2013.4. Astrup J, Siesjö BK, Symon L. Thresholds in cerebral ischemia - the ischemic penumbra. Stroke. 12:723–725. 1981.5. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 372:11–20. 2015.6. Berrouschot J, Sterker M, Bettin S, Köster J, Schneider D. Mortality of space-occupying (‘malignant’) middle cerebral artery infarction under conservative intensive care. Intensive Care Med. 24:620–623. 1998.7. Bhatia R, Hill MD, Shobha N, Menon B, Bal S, Kochar P, et al. Low rates of acute recanalization with intravenous recombinant tissue plasminogen activator in ischemic stroke: real-world experience and a call for action. Stroke. 41:2254–2258. 2010.8. Broderick JP, Berkhemer OA, Palesch YY, Dippel DW, Foster LD, Roos YB, et al. Endovascular therapy is effective and safe for patients with severe ischemic stroke: pooled analysis of interventional management of stroke III and multicenter randomized clinical trial of endovascular therapy for acute ischemic stroke in the Netherlands data. Stroke. 46:3416–3422. 2015.9. Butcher KS, Parsons M, MacGregor L, Barber PA, Chalk J, Bladin C, et al. Refining the perfusion-diffusion mismatch hypothesis. Stroke. 36:1153–1159. 2005.10. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 372:1009–1018. 2015.11. Caplan LR. Intracranial large artery occlusive disease. Curr Neurol Neurosci Rep. 8:177–181. 2008.12. Caplan LR, Gorelick PB, Hier DB. Race, sex and occlusive cerebrovascular disease: a review. Stroke. 17:648–655. 1986.13. Chimowitz MI, Lynn MJ, Howlett-Smith H, Stern BJ, Hertzberg VS, Frankel MR, et al. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med. 352:1305–1316. 2005.14. Ciccone A, Valvassori L, Nichelatti M, Sgoifo A, Ponzio M, Sterzi R, et al. Endovascular treatment for acute ischemic stroke. N Engl J Med. 368:904–913. 2013.15. Davis S, Donnan GA. Time is penumbra: imaging, selection and outcome. the Johann Jacob Wepfer award 2014. Cerebrovasc Dis. 38:59–72. 2014.16. De Silva DA, Brekenfeld C, Ebinger M, Christensen S, Barber PA, Butcher KS, et al. The benefits of intravenous thrombolysis relate to the site of baseline arterial occlusion in the Echoplanar Imaging Thrombolytic Evaluation Trial (EPITHET). Stroke. 41:295–299. 2010.17. Furlan A, Higashida R, Wechsler L, Gent M, Rowley H, Kase C, et al. Intra-arterial prourokinase for acute ischemic stroke. the PROACT II study: a randomized controlled trial. prolyse in acute cerebral thromboembolism. JAMA. 282:2003–2011. 1999.18. Gorelick PB, Wong KS, Bae HJ, Pandey DK. Large artery intracranial occlusive disease: a large worldwide burden but a relatively neglected frontier. Stroke. 39:2396–2399. 2008.19. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 372:1019–1030. 2015.20. Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 359:1317–1329. 2008.21. Hacke W, Schwab S, Horn M, Spranger M, De Georgia M, von Kummer R. ‘Malignant’ middle cerebral artery territory infarction: clinical course and prognostic signs. Arch Neurol. 53:309–315. 1996.22. Hofmeijer J, Kappelle LJ, Algra A, Amelink GJ, van Gijn J, van der Worp HB, et al. Surgical decompression for space-occupying cerebral infarction (the Hemicraniectomy After Middle Cerebral Artery infarction with Life-threatening Edema Trial [HAMLET]): a multicentre, open, randomised trial. Lancet Neurol. 8:326–333. 2009.23. Hong KS, Ko SB, Yu KH, Jung C, Park SQ, Kim BM, et al. Update of the Korean clinical practice guidelines for endovascular recanalization therapy in patients with acute ischemic stroke. J Stroke. 18:102–113. 2016.24. Hutchinson PJ, Kolias AG, Timofeev IS, Corteen EA, Czosnyka M, Timothy J, et al. Trial of decompressive craniectomy for traumatic intracranial hypertension. N Engl J Med. 375:1119–1130. 2016.25. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 372:2296–2306. 2015.26. Khatri P, Abruzzo T, Yeatts SD, Nichols C, Broderick JP, Tomsick TA, et al. Good clinical outcome after ischemic stroke with successful revascularization is time-dependent. Neurology. 73:1066–1072. 2009.27. Kidwell CS, Jahan R, Gornbein J, Alger JR, Nenov V, Ajani Z, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 368:914–923. 2013.28. Larrue V, von Kummer RR, Müller A, Bluhmki E. Risk factors for severe hemorrhagic transformation in ischemic stroke patients treated with recombinant tissue plasminogen activator: a secondary analysis of the European-Australasian Acute Stroke Study (ECASS II). Stroke. 32:438–441. 2001.29. Lewandowski CA, Frankel M, Tomsick TA, Broderick J, Frey J, Clark W, et al. Combined intravenous and intra-arterial r-TPA versus intra-arterial therapy of acute ischemic stroke: Emergency Management of Stroke (EMS) bridging trial. Stroke. 30:2598–2605. 1999.30. Lin J, Frontera JA. Decompressive hemicraniectomy for large hemispheric strokes. Stroke. 52:1500–1510. 2021.31. Mazighi M, Serfaty JM, Labreuche J, Laissy JP, Meseguer E, Lavallée PC, et al. Comparison of intravenous alteplase with a combined intravenous-endovascular approach in patients with stroke and confirmed arterial occlusion (RECANALISE study): a prospective cohort study. Lancet Neurol. 8:802–809. 2009.32. Mishra SM, Dykeman J, Sajobi TT, Trivedi A, Almekhlafi M, Sohn SI, et al. Early reperfusion rates with IV tPA are determined by CTA clot characteristics. AJNR Am J Neuroradiol. 35:2265–2272. 2014.33. Mlynash M, Lansberg MG, De Silva DA, Lee J, Christensen S, Straka M, et al. Refining the definition of the malignant profile: insights from the DEFUSE-EPITHET pooled data set. Stroke. 42:1270–1275. 2011.34. Muchada M, Rodriguez-Luna D, Pagola J, Flores A, Sanjuan E, Meler P, et al. Impact of time to treatment on tissue-type plasminogen activator-induced recanalization in acute ischemic stroke. Stroke. 45:2734–2738. 2014.35. National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 333:1581–1587. 1995.36. Paciaroni M, Agnelli G, Corea F, Ageno W, Alberti A, Lanari A, et al. Early hemorrhagic transformation of brain infarction: rate, predictive factors, and influence on clinical outcome: results of a prospective multicenter study. Stroke. 39:2249–2256. 2008.37. Paciaroni M, Balucani C, Agnelli G, Caso V, Silvestrelli G, Grotta JC, et al. Systemic thrombolysis in patients with acute ischemic stroke and Internal Carotid ARtery Occlusion: the ICARO study. Stroke. 43:125–130. 2012.38. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 49:e46–e110. 2018.39. Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke. 38:967–973. 2007.40. Ribo M, Alvarez-Sabín J, Montaner J, Romero F, Delgado P, Rubiera M, et al. Temporal profile of recanalization after intravenous tissue plasminogen activator: selecting patients for rescue reperfusion techniques. Stroke. 37:1000–1004. 2006.41. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 372:2285–2295. 2015.42. Seners P, Turc G, Maïer B, Mas JL, Oppenheim C, Baron JC. Incidence and predictors of early recanalization after intravenous thrombolysis: a systematic review and meta-analysis. Stroke. 47:2409–2412. 2016.43. Tsivgoulis G, Katsanos AH, Schellinger PD, Köhrmann M, Varelas P, Magoufis G, et al. Successful reperfusion with intravenous thrombolysis preceding mechanical thrombectomy in large-vessel occlusions. Stroke. 49:232–235. 2018.44. Wardlaw JM, Murray V, Berge E, del Zoppo G, Sandercock P, Lindley RL, et al. Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis. Lancet. 379:2364–2372. 2012.45. Wei XE, Zhao YW, Lu J, Li MH, Li WB, Zhou YJ, et al. Timing of recanalization and outcome in ischemic-stroke patients treated with recombinant tissue plasminogen activator. Acta Radiol. 56:1119–1126. 2015.46. Yoo DS, Kim DS, Cho KS, Huh PW, Park CK, Kang JK. Ventricular pressure monitoring during bilateral decompression with dural expansion. J Neurosurg. 91:953–959. 1999.47. Yoo DS, Won YD, Huh PW, Shin HE, Kim KT, Kang SG, et al. Therapeutic results of intra-arterial thrombolysis after full-dose intravenous tissue plasminogen activator administration. AJNR Am J Neuroradiol. 31:1536–1540. 2010.48. Yoon W, Seo JJ, Kim JK, Cho KH, Park JG, Kang HK. Contrast enhancement and contrast extravasation on computed tomography after intraarterial thrombolysis in patients with acute ischemic stroke. Stroke. 35:876–881. 2004.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recanalization Rate and its Associated Factors after Intravenous Tissue Plasminogen Activator Thrombolysis for Acute Major Cerebral Arterial Occlusion
- Previous and Recent Evidence of Endovascular Therapy in Acute Ischemic Stroke
- Clinical Results of the Intra-Arterial Thrombolysis with Stent Retriever Device Weather Perfusion Diffusion Mismatching and Intravenous Tissue Plasminogen Activator Administration
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom
- Emergency management of stroke in the era of mechanical thrombectomy