J Cerebrovasc Endovasc Neurosurg.
2017 Dec;19(4):257-267. 10.7461/jcen.2017.19.4.257.
Clinical Results of the Intra-Arterial Thrombolysis with Stent Retriever Device Weather Perfusion Diffusion Mismatching and Intravenous Tissue Plasminogen Activator Administration
- Affiliations
-
- 1Department of Neurosurgery, Yeouido St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 2Department of Neurosurgery, Bucheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Bucheon, Korea.
- 3Department of Neurosurgery, St. Paul's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. yooman@catholic.ac.kr
- KMID: 2401778
- DOI: http://doi.org/10.7461/jcen.2017.19.4.257
Abstract
OBJECTIVE
Intraarterial thrombolysis (IA-Tx) with stent retriever is accepted as an additional treatment for selected patients and the clinical benefit is well reported. Each intravenous tissue plasminogen activator administration (IV-tPA) and perfusion diffusion mismatching (P/D-mismatching) is well known the beneficial effects for recanalization and clinical outcomes. In this report, authors analyzed the clinical outcomes of additional IA-Tx with retrieval stent device, according to the combined IV-tPA and P/D-mismatching or not.
METHODS
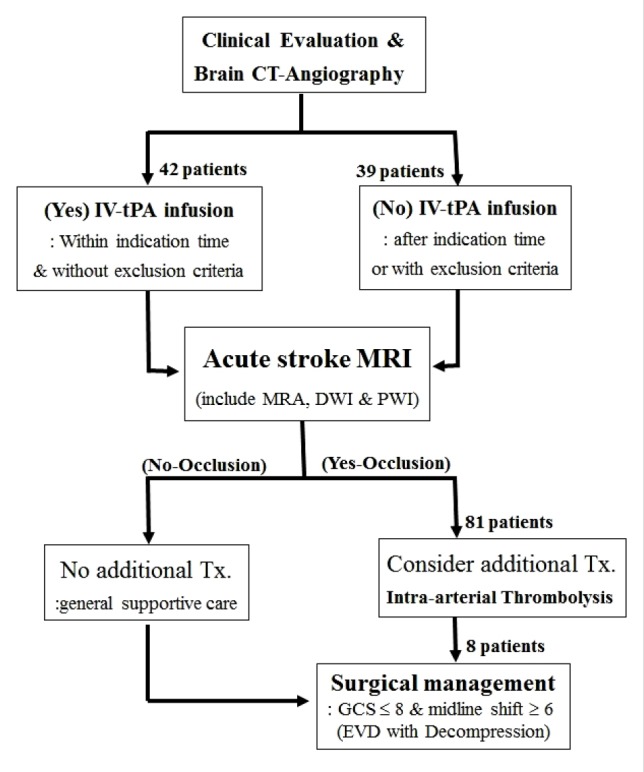
Eighty-one treated IA-Tx with the Solitaire stent retriever device, diagnosed as anterior circulation larger vessel occlusion were included in this study. Computed tomography-angiography (CTA) was done as an initial diagnostic image and acute stroke magnetic resonance image (MRI) followed after the IV-tPA. Forty-two patients were in the tPA group and 39 patients were in the non-tPA group. Recanalization rate, clinically significant hemorrhagic (sICH) and clinical outcomes were recorded according to the IV-tPA and P/D-mismatching.
RESULTS
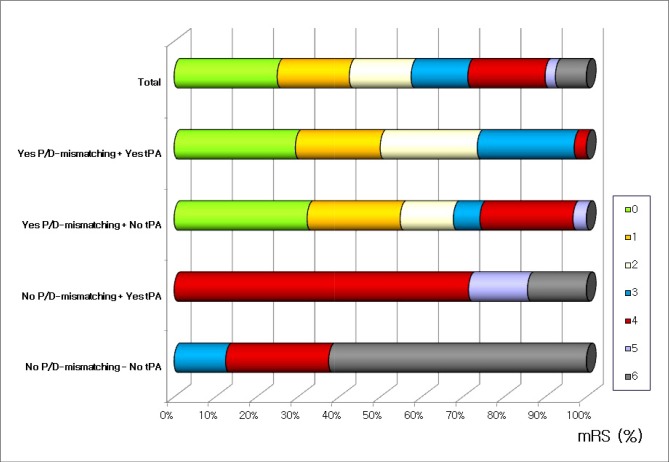
Recanalization rate was 81.0% in IV-tPA group, and it was 69.2% in non-tPA group (p = 0.017). While sICH were 19.9% and 25.6%, respectively (p = 0.328). Neurologic outcomes did not influence by IV-tPA administration or not. But according to the P/D-mismatching, the recanalization rate and sICH were 91.9% and 16.7% in the mismatched group and 46.7% and 46.7% in the matched group (p = 0.008 and p = 0.019, respectively).
CONCLUSION
For patients treated with IA-Tx with retrieval stent, IV-tPA infusion does not influence on the sICH, recanalization rate and neurologic outcomes. But P/D-mismatching was correlated well with sICH, recanalization rate and clinical outcomes.
Keyword
MeSH Terms
Figure
Reference
-
1. Albers GW, Thijs VN, Wechsler L, Kemp S, Schlaug G, Skalabrin E, et al. Magnetic resonance imaging profiles predict clinical response to early reperfusion: the diffusion and perfusion imaging evaluation for understanding stroke evolution (DEFUSE) study. Ann Neurol. 2006; 11. 60(5):508–517. PMID: 17066483.
Article2. Astrup J, Siesjö BK, Symon L. Thresholds in cerebral ischemia - the ischemic penumbra. Stroke. 1981; Nov-Dec. 12(6):723–725. PMID: 6272455.
Article3. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 1. 372(1):11–20. PMID: 25517348.4. Bhatia R, Shobha N, Menon BK, Bal SP, Kochar P, Palumbo V, et al. Combined full-dose IV and endovascular thrombolysis in acute ischaemic stroke. Int J Stroke. 2014; 12. 9(8):974–979. PMID: 23013039.
Article5. Broderick JP, Palesch YY, Demchuk AM, Yeatts SD, Khatri P, Hill MD, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013; 3. 368(10):893–903. PMID: 23390923.
Article6. Butcher K, Parsons M, Allport L, Lee SB, Barber PA, Tress B, et al. Rapid assessment of perfusion-diffusion mismatch. Stroke. 2008; 1. 39(1):75–81. PMID: 18063829.
Article7. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015; 3. 372(11):1009–1018. PMID: 25671797.
Article8. Ciccone A, Valvassori L, Nichelatti M, Sgoifo A, Ponzio M, Sterzi R, et al. Endovascular treatment for acute ischemic stroke. N Engl J Med. 2013; 3. 368(10):904–913. PMID: 23387822.
Article9. de Los Ríos la Rosa F, Khoury J, Kissela BM, Flaherty ML, Alwell K, Moomaw CJ, et al. Eligibility for intravenous recombinant tissue-type plasminogen activator within a population: the effect of the European Cooperative Acute Stroke Study (ECASS) III trial. Stroke. 2012; 6. 43(6):1591–1595. PMID: 22442174.10. del Zoppo GJ, Higashida RT, Furlan AJ, Pessin MS, Rowley HA, Gent M. PROACT: a phase II randomized trial of recombinant pro-urokinase by direct arterial delivery in acute middle cerebral artery stroke. PROACT Investigators. Prolyse in Acute Cerebral Thromboembolism. Stroke. 1998; 1. 29(1):4–11. PMID: 9445320.11. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 3. 372(11):1019–1030. PMID: 25671798.12. Grotta JC, Hacke W. Stroke neurologist's perspective on the new endovascular trials. Stroke. 2015; 6. 46(6):1447–1452. PMID: 25944328.
Article13. Hofmeijer J, Kappelle LJ, Algra A, Amelink GJ, van Gijn J, van der Worp HB. HAMLET investigators. Surgical decompression for space-occupying cerebral infarction (the Hemicraniectomy After Middle Cerebral Artery infarction with Life-threatening Edema Trial [HAMLET]): a multicentre, open, randomised trial. Lancet Neurol. 2009; 4. 8(4):326–333. PMID: 19269254.
Article14. IMS Study Investigators. Combined intravenous and intra-arterial recanalization for acute ischemic stroke: the Interventional Management of Stroke Study. Stroke. 2004; 4. 35(4):904–911. PMID: 15017018.15. IMS II Trial Investigators. The Interventional Management of Stroke (IMS) II Study. Stroke. 2007; 1. 38(7):2127–2135. PMID: 17525387.16. Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013; 3. 44(3):870–947. PMID: 23370205.17. Jüttler E, Schwab S, Schmiedek P, Unterberg A, Hennerici M, Woitzik J, et al. Decompressive Surgery for the Treatment of Malignant Infarction of the Middle Cerebral Artery (DESTINY): a randomized, controlled trial. Stroke. 2007; 9. 38(9):2518–2525. PMID: 17690310.18. Kim KT, Park JK, Kang SG, Cho KS, Yoo DS, Jang DK, et al. Comparison of the effect of decompressive craniectomy on different neurosurgical diseases. Acta Neurochir (Wien). 2009; 1. 151(1):21–30. PMID: 19096757.
Article19. Larrue V, von Kummer R R, Müller A, Bluhmki E. Risk factors for severe hemorrhagic transformation in ischemic stroke patients treated with recombinant tissue plasminogen activator: a secondary analysis of the European-Australasian Acute Stroke Study (ECASS II). Stroke. 2001; 2. 32(2):438–441. PMID: 11157179.20. Lees KR, Bluhmki E, von Kummer R, Brott TG, Toni D, Grotta JC, et al. Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet. 2010; 5. 375(9727):1695–1703. PMID: 20472172.
Article21. Lewandowski CA, Frankel M, Tomsick TA, Broderick J, Frey J, Clark W, et al. Combined intravenous and intra-arterial r-TPA versus intra-arterial therapy of acute ischemic stroke: Emergency Management of Stroke (EMS) Bridging Trial. Stroke. 1999; 12. 30(12):2598–2605. PMID: 10582984.22. Liebeskind DS. Trials of endovascular therapies or collaterals? Int J Stroke. 2013; 6. 8(4):258–259. PMID: 23692483.
Article23. Luby M, Warach SJ, Albers GW, Baron JC, Cognard C, Dávalos A, et al. Identification of imaging selection patterns in acute ischemic stroke patients and the influence on treatment and clinical trial enrollment decision making. Int J Stroke. 2016; 2. 11(2):180–190. PMID: 26783309.
Article24. Masdeu JC, Irimia P, Asenbaum S, Bogousslavsky J, Brainin M, Chabriat H, et al. EFNS guideline on neuroimaging in acute stroke. Report of an EFNS task force. Eur J Neurol. 2006; 12. 13(12):1271–1283. PMID: 17116208.
Article25. Mazighi M, Serfaty JM, Labreuche J, Laissy JP, Meseguer E, Lavallée PC, et al. Comparison of intravenous alteplase with a combined intravenous-endovascular approach in patients with stroke and confirmed arterial occlusion (RECANALISE study): a prospective cohort study. Lancet Neurol. 2009; 9. 8(9):802–809. PMID: 19647488.
Article26. Menon BK, Campbell BC, Levi C, Goyal M. Role of imaging in current acute ischemic stroke workflow for endovascular therapy. Stroke. 2015; 6. 46(6):1453–1461. PMID: 25944319.
Article27. Paciaroni M, Agnelli G, Corea F, Ageno W, Alberti A, Lanari A, et al. Early hemorrhagic transformation of brain infarction: rate, predictive factors, and influence on clinical outcome: results of a prospective multicenter study. Stroke. 2008; 8. 39(8):2249–2256. PMID: 18535273.28. Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke. 2007; 3. 38(3):967–973. PMID: 17272772.29. Riedel CH, Zimmermann P, Jensen-Kondering U, Stingele R, Deuschl G, Jansen O. The importance of size: successful recanalization by intravenous thrombolysis in acute anterior stroke depends on thrombus length. Stroke. 2011; 6. 42(6):1775–1777. PMID: 21474810.30. Saqqur M, Uchino K, Demchuk AM, Molina CA, Garami Z, Calleja S, et al. Site of arterial occlusion identified by transcranial Doppler predicts the response to intravenous thrombolysis for stroke. Stroke. 2007; 3. 38(3):948–954. PMID: 17290031.
Article31. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Solitaire™ with the Intention for Thrombectomy as Primary Endovascular Treatment for Acute Ischemic Stroke (SWIFT PRIME) trial: protocol for a randomized, controlled, multicenter study comparing the Solitaire revascularization device with IV tPA with IV tPA alone in acute ischemic stroke. Int J Stroke. 2015; 4. 10(3):439–448. PMID: 25777831.
Article32. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995; 12. 333(24):1581–1587. PMID: 7477192.33. Vahedi K, Vicaut E, Mateo J, Kurtz A, Orabi M, Guichard JP, et al. Sequential-design, multicenter, randomized, controlled trial of early decompressive craniectomy in malignant middle cerebral artery infarction (DECIMAL Trial). Stroke. 2007; 9. 38(9):2506–2517. PMID: 17690311.
Article34. Wardlaw JM, Murray V, Berge E, del Zoppo G, Sandercock P, Lindley RL, et al. Recombinant tissue plasminogen activator for acute ischaemic stroke: an updated systematic review and meta-analysis. Lancet. 2012; 6. 379(9834):2364–2372. PMID: 22632907.
Article35. Won YD, Lee TK, Kim YJ, Chun CW, Yoo DS, Jun SS. Clinical results of intraarterial thrombolysis according to tPA administration and perfusion/diffusion mismatching. Acta Neurochir (Wien). 2015; 3. 157(3):389–398. PMID: 25585838.
Article36. Yeatts SD, Martin RH, Coffey CS, Lyden PD, Foster LD, Woolson RF, et al. Challenges of decision making regarding futility in a randomized trial: the Interventional Management of Stroke III experience. Stroke. 2014; 5. 45(5):1408–1414. PMID: 24699059.37. Yoo DS, Kim DS, Cho KS, Huh PW, Park CK, Kang JK. Ventricular pressure monitoring during bilateral decompression with dural expansion. J Neurosurg. 1999; 12. 91(6):953–959. PMID: 10584840.
Article38. Yoo DS, Won YD, Huh PW, Shin HE, Kim KT, Kang SG, et al. Therapeutic results of intra-arterial thrombolysis after full-dose intravenous tissue plasminogen activator administration. AJNR Am J Neuroradiol. 2010; 9. 31(8):1536–1540. PMID: 20395391.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Acute Ischemic Stroke: Thrombolysis
- Recent advances in thrombolysis of acute ischemic stroke
- Thrombolytic Treatment of Acute Stroke
- Endovascular Stroke Therapy Focused on Stent Retriever Thrombectomy and Direct Clot Aspiration: Historical Review and Modern Application
- Emergent Double-barrel Bypass Shortly after Intravenous Administration of Recombinant Tissue Plasminogen Activator for Acute Ischemic Stroke