Endocrinol Metab.
2023 Feb;38(1):146-155. 10.3803/EnM.2022.1582.
Sleep Duration and the Risk of Type 2 Diabetes: A Community-Based Cohort Study with a 16-Year Follow-up
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea
- 2Institute of Human Genomic Study, Korea University Ansan Hospital, Ansan, Korea
- 3BK21 FOUR R&E Center for Learning Health Systems, Korea University, Seoul, Korea
- KMID: 2539828
- DOI: http://doi.org/10.3803/EnM.2022.1582
Abstract
- Background
We aimed to investigate the moderating effects of obesity, age, and sex on the association between sleep duration and the development of diabetes in Asians.
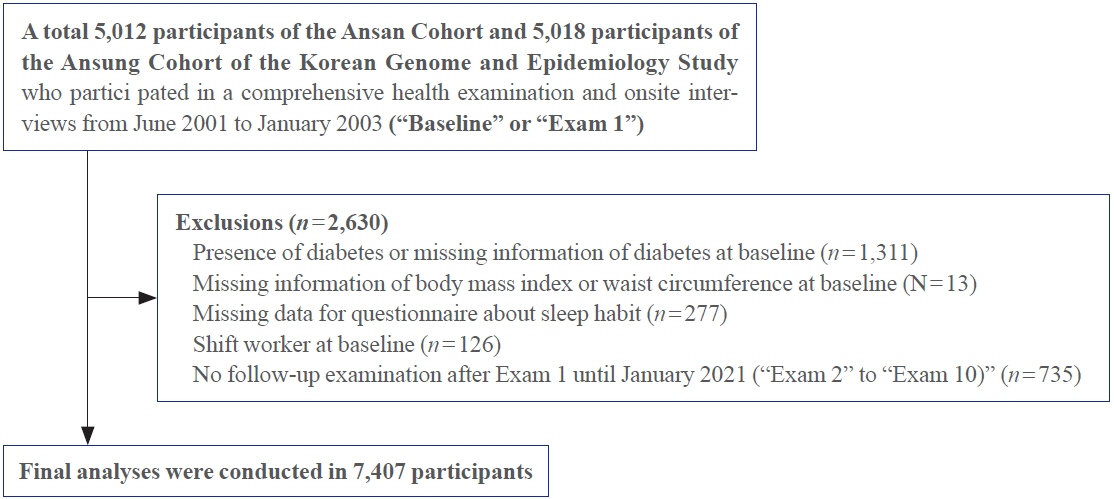
Methods
We analyzed data from a cohort of the Korean Genome and Epidemiology Study conducted from 2001 to 2020. After excluding shift workers and those with diabetes at baseline, 7,407 participants were stratified into three groups according to sleep duration: ≤5 hours/night, >5 to 7 hours/night (reference), and >7 hours/night. The Cox proportional hazards analyses were used to calculate the hazard ratios (HRs) and 95% confidence intervals (CIs) for incident type 2 diabetes mellitus (T2DM). Subgroup analyses were performed according to obesity, age, and sex.
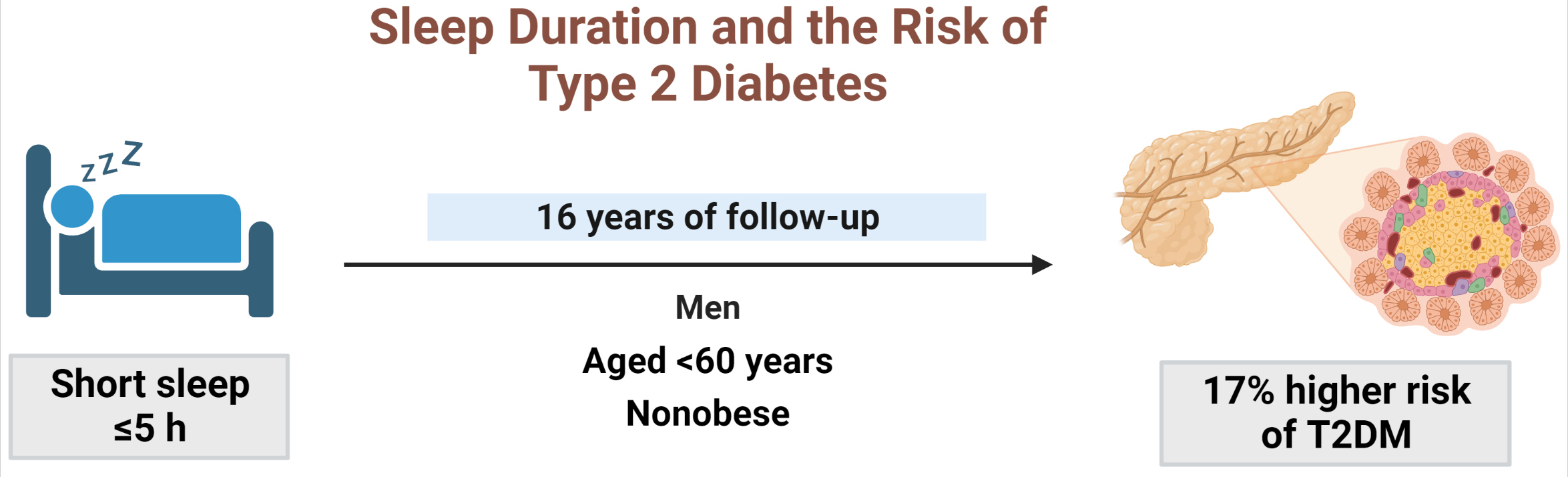
Results
During 16 years of follow-up, 2,024 cases of T2DM were identified. Individuals who slept ≤5 h/night had a higher risk of incident diabetes than the reference group (HR, 1.17; 95% CI, 1.02 to 1.33). The subgroup analysis observed a valid interaction with sleep duration only for obesity. A higher risk of T2DM was observed in the ≤5 hours/night group in non-obese individuals, men, and those aged <60 years, and in the >7 hours/night group in obese individuals (HRs were 1.34 [95% CI, 1.11 to 1.61], 1.22 [95% CI, 1 to 1.49], and 1.18 [95% CI, 1.01 to 1.39], respectively).
Conclusion
This study confirmed the effect of sleep deprivation on the risk of T2DM throughout the 16-year follow-up period. This impact was confined to non-obese or young individuals and men. We observed a significant interaction between sleep duration and obesity.
Keyword
Figure
Cited by 1 articles
-
All That Glitters Is Not Gold: The Same Sleep Time, but Different Diabetogenic Outcomes
Bohye Kim, Obin Kwon
Endocrinol Metab. 2023;38(1):78-80. doi: 10.3803/EnM.2023.107.
Reference
-
1. Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022; 183:109119.
Article2. Hu FB, Manson JE, Stampfer MJ, Colditz G, Liu S, Solomon CG, et al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med. 2001; 345:790–7.
Article3. Itani O, Jike M, Watanabe N, Kaneita Y. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med. 2017; 32:246–56.
Article4. Gordon S, Vandelanotte C, Rayward AT, Murawski B, Duncan MJ. Sociodemographic and behavioral correlates of insufficient sleep in Australian adults. Sleep Health. 2019; 5:12–7.
Article5. Van Cauter E, Knutson KL. Sleep and the epidemic of obesity in children and adults. Eur J Endocrinol. 2008; 159 Suppl 1:S59–66.
Article6. Chattu VK, Manzar MD, Kumary S, Burman D, Spence DW, Pandi-Perumal SR. The global problem of insufficient sleep and its serious public health implications. Healthcare (Basel). 2018; 7:1.
Article7. Lu H, Yang Q, Tian F, Lyu Y, He H, Xin X, et al. A meta-analysis of a cohort study on the association between sleep duration and type 2 diabetes mellitus. J Diabetes Res. 2021; 2021:8861038.
Article8. Shan Z, Ma H, Xie M, Yan P, Guo Y, Bao W, et al. Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care. 2015; 38:529–37.
Article9. Antza C, Kostopoulos G, Mostafa S, Nirantharakumar K, Tahrani A. The links between sleep duration, obesity and type 2 diabetes mellitus. J Endocrinol. 2021; 252:125–41.
Article10. Maskarinec G, Jacobs S, Amshoff Y, Setiawan VW, Shvetsov YB, Franke AA, et al. Sleep duration and incidence of type 2 diabetes: the Multiethnic Cohort. Sleep Health. 2018; 4:27–32.
Article11. Leng Y, Cappuccio FP, Surtees PG, Luben R, Brayne C, Khaw KT. Daytime napping, sleep duration and increased 8-year risk of type 2 diabetes in a British population. Nutr Metab Cardiovasc Dis. 2016; 26:996–1003.
Article12. Wu IH, Heredia N, Dong Q, McNeill LH, Balachandran DD, Lu Q, et al. Sleep duration and type 2 diabetes risk: a prospective study in a population-based Mexican American cohort. Sleep Health. 2021; 7:168–76.
Article13. Beihl DA, Liese AD, Haffner SM. Sleep duration as a risk factor for incident type 2 diabetes in a multiethnic cohort. Ann Epidemiol. 2009; 19:351–7.14. Han X, Liu B, Wang J, Pan A, Li Y, Hu H, et al. Long sleep duration and afternoon napping are associated with higher risk of incident diabetes in middle-aged and older Chinese: the Dongfeng-Tongji cohort study. Ann Med. 2016; 48:216–23.
Article15. Hayashino Y, Fukuhara S, Suzukamo Y, Okamura T, Tanaka T, Ueshima H, et al. Relation between sleep quality and quantity, quality of life, and risk of developing diabetes in healthy workers in Japan: the High-risk and Population Strategy for Occupational Health Promotion (HIPOP-OHP) Study. BMC Public Health. 2007; 7:129.
Article16. Kita T, Yoshioka E, Satoh H, Saijo Y, Kawaharada M, Okada E, et al. Short sleep duration and poor sleep quality increase the risk of diabetes in Japanese workers with no family history of diabetes. Diabetes Care. 2012; 35:313–8.
Article17. Heianza Y, Kato K, Fujihara K, Tanaka S, Kodama S, Hanyu O, et al. Role of sleep duration as a risk factor for Type 2 diabetes among adults of different ages in Japan: the Niigata Wellness Study. Diabet Med. 2014; 31:1363–7.
Article18. Lou P, Zhang P, Zhang L, Chen P, Chang G, Zhang N, et al. Effects of sleep duration and sleep quality on prevalence of type 2 diabetes mellitus: a 5-year follow-up study in China. Diabetes Res Clin Pract. 2015; 109:178–84.
Article19. Cui S, Li Y, Chen Y, Ren P, Fan M, Yang X, et al. Association of sleep duration with risk of type 2 diabetes mellitus in a rural Chinese population: a nested case-control study. Sleep Breath. 2022; 26:2025–33.
Article20. Kim CW, Chang Y, Sung E, Ryu S. Sleep duration and progression to diabetes in people with prediabetes defined by HbA1c concentration. Diabet Med. 2017; 34:1591–8.21. Perry GS, Patil SP, Presley-Cantrell LR. Raising awareness of sleep as a healthy behavior. Prev Chronic Dis. 2013; 10:E133.
Article22. Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2010; 33:414–20.23. Nielsen LS, Danielsen KV, Sorensen TI. Short sleep duration as a possible cause of obesity: critical analysis of the epidemiological evidence. Obes Rev. 2011; 12:78–92.
Article24. Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010; 71:1027–36.
Article25. Wu Y, Zhai L, Zhang D. Sleep duration and obesity among adults: a meta-analysis of prospective studies. Sleep Med. 2014; 15:1456–62.
Article26. Jean-Louis G, Williams NJ, Sarpong D, Pandey A, Youngstedt S, Zizi F, et al. Associations between inadequate sleep and obesity in the US adult population: analysis of the national health interview survey (1977-2009). BMC Public Health. 2014; 14:290.
Article27. Yang YS, Han BD, Han K, Jung JH, Son JW; Taskforce Team of the Obesity Fact Sheet of the Korean Society for the Study of Obesity. Obesity fact sheet in Korea, 2021: trends in obesity prevalence and obesity-related comorbidity incidence stratified by age from 2009 to 2019. J Obes Metab Syndr. 2022; 31:169–77.
Article28. Chan JC, Malik V, Jia W, Kadowaki T, Yajnik CS, Yoon KH, et al. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA. 2009; 301:2129–40.29. Song Q, Liu X, Zhou W, Wang X, Wu S. Short-term changes in sleep duration and risk of type 2 diabetes: Kailuan prospective study. Medicine (Baltimore). 2016; 95:e5363.30. Kim NH, Cho NH, Yun CH, Lee SK, Yoon DW, Cho HJ, et al. Association of obstructive sleep apnea and glucose metabolism in subjects with or without obesity. Diabetes Care. 2013; 36:3909–15.
Article31. Baik I, Shin C. Prospective study of alcohol consumption and metabolic syndrome. Am J Clin Nutr. 2008; 87:1455–63.
Article32. Kim H, Yun CH, Thomas RJ, Lee SH, Seo HS, Cho ER, et al. Obstructive sleep apnea as a risk factor for cerebral white matter change in a middle-aged and older general population. Sleep. 2013; 36:709–15B.
Article33. Seo JA, Lee DY, Yu JH, Cho H, Lee SK, Suh S, et al. Habitual late sleep initiation is associated with increased incidence of type 2 diabetes mellitus in Korean adults: the Korean Genome and Epidemiology Study. Sleep. 2019; 42:zsz090.
Article34. Joo S, Lee S, Choi HA, Kim J, Kim E, Kimm K, et al. Habitual snoring is associated with elevated hemoglobin A1c levels in non-obese middle-aged adults. J Sleep Res. 2006; 15:437–44.
Article35. American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2018. Diabetes Care. 2018; 41(Suppl 1):S13–27.36. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985; 28:412–9.
Article37. Kim BY, Kang SM, Kang JH, Kang SY, Kim KK, Kim KB, et al. 2020 Korean Society for the Study of Obesity guidelines for the management of obesity in Korea. J Obes Metab Syndr. 2021; 30:81–92.
Article38. Schmidt MH. The energy allocation function of sleep: a unifying theory of sleep, torpor, and continuous wakefulness. Neurosci Biobehav Rev. 2014; 47:122–53.
Article39. Balbo M, Leproult R, Van Cauter E. Impact of sleep and its disturbances on hypothalamo-pituitary-adrenal axis activity. Int J Endocrinol. 2010; 2010:759234.
Article40. Van Cauter E, Holmback U, Knutson K, Leproult R, Miller A, Nedeltcheva A, et al. Impact of sleep and sleep loss on neuroendocrine and metabolic function. Horm Res. 2007; 67 Suppl 1:2–9.
Article41. Knutson KL, Spiegel K, Penev P, Van Cauter E. The metabolic consequences of sleep deprivation. Sleep Med Rev. 2007; 11:163–78.
Article42. Spiegel K, Knutson K, Leproult R, Tasali E, Van Cauter E. Sleep loss: a novel risk factor for insulin resistance and type 2 diabetes. J Appl Physiol (1985). 2005; 99:2008–19.
Article43. van Leeuwen WM, Lehto M, Karisola P, Lindholm H, Luukkonen R, Sallinen M, et al. Sleep restriction increases the risk of developing cardiovascular diseases by augmenting proinflammatory responses through IL-17 and CRP. PLoS One. 2009; 4:e4589.
Article44. Gutierrez-Repiso C, Soriguer F, Rubio-Martin E, Esteva de Antonio I, Ruiz de Adana MS, Almaraz MC, et al. Nighttime sleep duration and the incidence of obesity and type 2 diabetes: findings from the prospective Pizarra study. Sleep Med. 2014; 15:1398–404.
Article45. Stefan L, Sporis G, Kristicevic T, Knjaz D. Associations between sleep quality and its domains and insufficient physical activity in a large sample of Croatian young adults: a crosssectional study. BMJ Open. 2018; 8:e021902.
Article46. Kim J, Jo I. Age-dependent association between sleep duration and hypertension in the adult Korean population. Am J Hypertens. 2010; 23:1286–91.
Article47. Hairston KG, Bryer-Ash M, Norris JM, Haffner S, Bowden DW, Wagenknecht LE. Sleep duration and five-year abdominal fat accumulation in a minority cohort: the IRAS family study. Sleep. 2010; 33:289–95.
Article48. Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004; 27:1255–73.
Article49. Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008; 19:838–45.50. Kim JH, Jung DH, Kwon YJ, Lee JI, Shim JY. The impact of the sleep duration on NAFLD score in Korean middle-aged adults: a community-based cohort study. Sleep Med. 2019; 57:144–50.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Sleep Quality on the Development of Type 2 Diabetes in Primary Care Patients
- Impact of Sleep Duration on Decline in Kidney Function in Adult Patients with Hypertension: A Community-Based Prospective Cohort Study
- Sleep and Diabetes
- The Effect of Sleep Duration and Relief of Fatigue after Sleep on the Risk of Injury at School among Korean Adolescents
- Obstructive Sleep Apnea and Type 2 Diabetes