Lower Thyroid Cancer Mortality in Patients Detected by Screening: A Meta-Analysis
- Affiliations
-
- 1Department of Internal Medicine, Hallym University Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea
- 2Department of Internal Medicine, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea
- 3Department of Internal Medicine, Nowon Eulji Medical Center, Eulji University, Seoul, Korea
- 4Department of Internal Medicine, Center for Thyroid Cancer, National Cancer Center, Goyang, Korea
- 5Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- 6Department of Molecular Medicine and Biopharmaceutical Sciences Graduate School of Convergence Science and Technology, Seoul National University, Seoul, Korea
- KMID: 2539823
- DOI: http://doi.org/10.3803/EnM.2023.1667
Abstract
- Background
Thyroid cancer screening has contributed to the skyrocketing prevalence of thyroid cancer. However, the true benefit of thyroid cancer screening is not fully understood. This study aimed to evaluate the impact of screening on the clinical outcomes of thyroid cancer by comparing incidental thyroid cancer (ITC) with non-incidental thyroid cancer (NITC) through a meta-analysis.
Methods
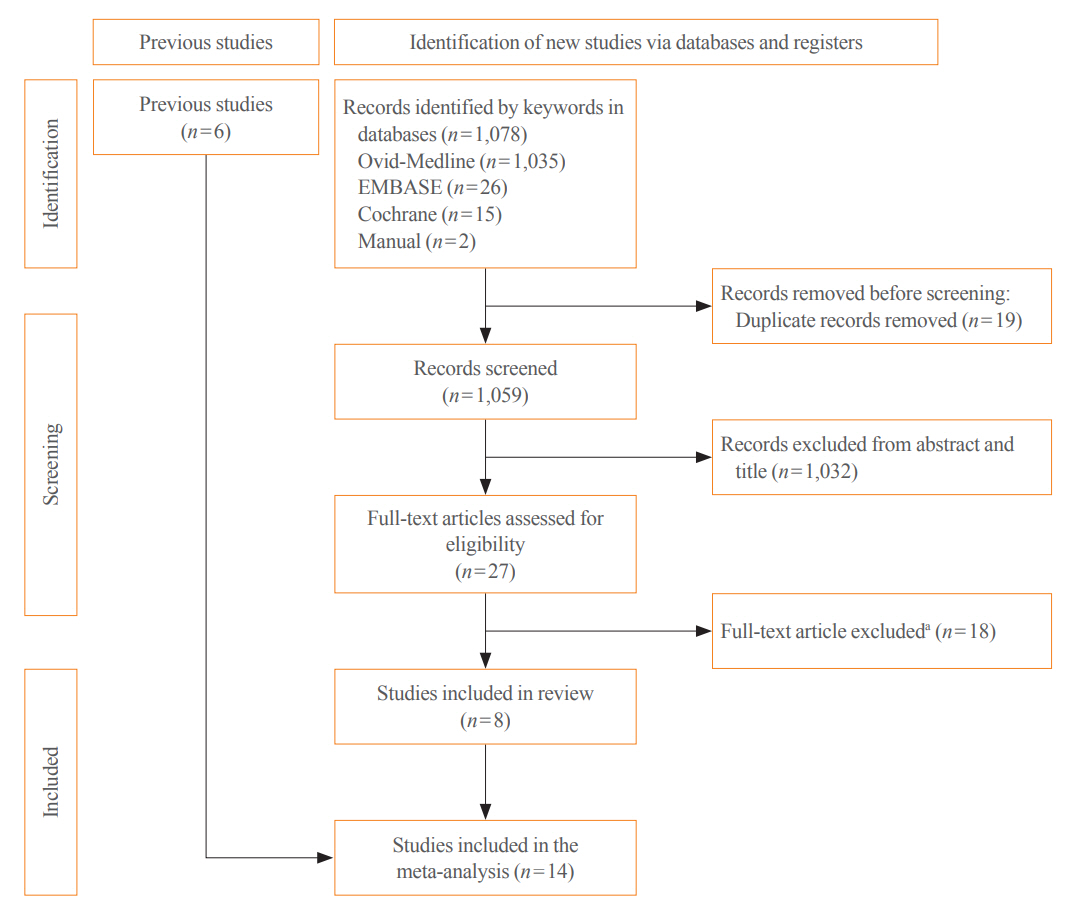
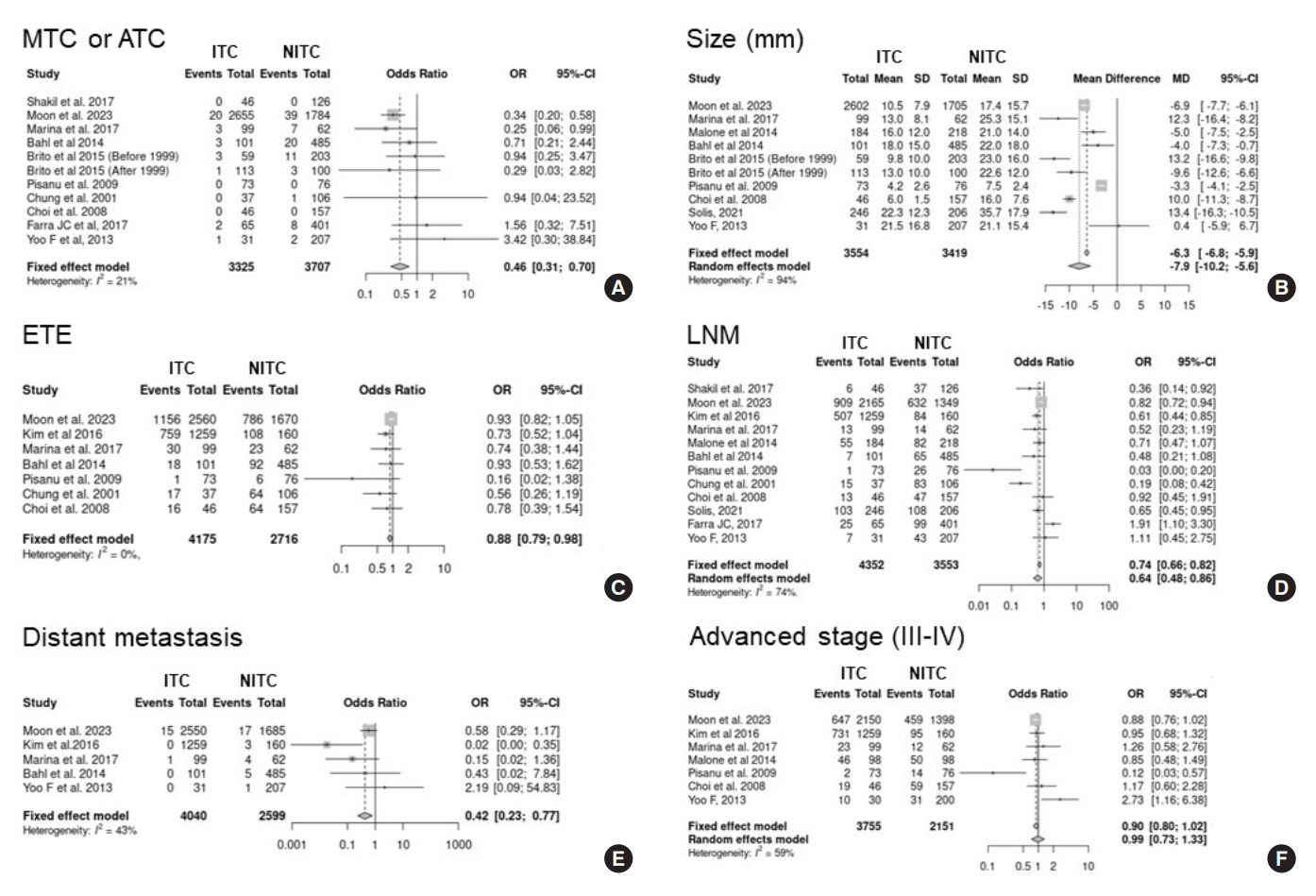
PubMed and Embase were searched from inception to September 2022. We estimated and compared the prevalence of high-risk features (aggressive histology of thyroid cancer, extrathyroidal extension, metastasis to regional lymph nodes or distant organs, and advanced tumor-node-metastasis [TNM] stage), thyroid cancer-specific death, and recurrence in the ITC and NITC groups. We also calculated pooled risks and 95% confidence intervals (CIs) of the outcomes derived from these two groups.
Results
From 1,078 studies screened, 14 were included. In comparison to NITC, the ITC group had a lower incidence of aggressive histology (odds ratio [OR], 0.46; 95% CI, 0.31 to 0.7), smaller tumors (mean difference, −7.9 mm; 95% CI, −10.2 to −5.6), lymph node metastasis (OR, 0.64; 95% CI, 0.48 to 0.86), and distant metastasis (OR, 0.42; 95% CI, 0.23 to 0.77). The risks of recurrence and thyroid cancer-specific mortality were also lower in the ITC group (OR, 0.42; 95% CI, 0.25 to 0.71 and OR, 0.46; 95% CI, 0.28 to 0.74) than in the NITC group.
Conclusion
Our findings provide important evidence of a survival benefit from the early detection of thyroid cancer compared to symptomatic thyroid cancer.
Keyword
Figure
Cited by 4 articles
-
Thyroid Cancer Screening: How to Maximize Its Benefits and Minimize Its Harms
Jung Hwan Baek
Endocrinol Metab. 2023;38(1):75-77. doi: 10.3803/EnM.2023.105.To Screen or Not to Screen?
Do Joon Park
Endocrinol Metab. 2023;38(1):69-71. doi: 10.3803/EnM.2023.104.The 2017 United States Preventive Services Task Force Recommendation for Thyroid Cancer Screening Is No Longer the Gold Standard
Ka Hee Yi
Endocrinol Metab. 2023;38(1):72-74. doi: 10.3803/EnM.2023.106.Cost-Utility Analysis of Early Detection with Ultrasonography of Differentiated Thyroid Cancer: A Retrospective Study on a Korean Population
Han-Sang Baek, Jeonghoon Ha, Kwangsoon Kim, Ja Seong Bae, Jeong Soo Kim, Sungju Kim, Dong-Jun Lim, Chul-Min Kim
Endocrinol Metab. 2024;39(2):310-323. doi: 10.3803/EnM.2023.1870.
Reference
-
1. Kim J, Gosnell JE, Roman SA. Geographic influences in the global rise of thyroid cancer. Nat Rev Endocrinol. 2020; 16:17–29.
Article2. Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA. 2006; 295:2164–7.
Article3. Pizzato M, Li M, Vignat J, Laversanne M, Singh D, La Vecchia C, et al. The epidemiological landscape of thyroid cancer worldwide: GLOBOCAN estimates for incidence and mortality rates in 2020. Lancet Diabetes Endocrinol. 2022; 10:264–72.
Article4. Li M, Dal Maso L, Vaccarella S. Global trends in thyroid cancer incidence and the impact of overdiagnosis. Lancet Diabetes Endocrinol. 2020; 8:468–70.
Article5. Lin JS, Bowles EJ, Williams SB, Morrison CC. Screening for thyroid cancer: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2017; 317:1888–903.6. Yi KH, Kim SY, Kim DH, Kim SW, Na DG, Lee YJ, et al. The Korean guideline for thyroid cancer screening. J Korean Med Assoc. 2015; 58:302–12.
Article7. US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, Curry SJ, Barry MJ, Davidson KW, et al. Screening for thyroid cancer: US Preventive Services Task Force recommendation statement. JAMA. 2017; 317:1882–7.8. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009; 339:b2535.
Article9. National Evidence-based Healthcare Collaborating Agency. Effectiveness of ultrasonographic screening for thyroid cancer 2012 [Internet]. Seoul: NECA;2023. [cited 2023 Feb 17]. Available from: https://neca.re.kr.10. Chooi JE, Ravindiran A, Balasubramanian SP. The influence of incidental detection of thyroid nodule on thyroid cancer risk and prognosis: a systematic review. Clin Endocrinol (Oxf). 2022; 96:246–54.11. Shakil J, Ansari MZ, Brady J, Xu J, Robbins RJ. Lower rates of residual/recurrent disease in patients with incidentally discovered thyroid carcinoma. Endocr Pract. 2017; 23:163–9.
Article12. Kim SH, Roh JL, Gong G, Cho KJ, Choi SH, Nam SY, et al. Differences in the recurrence and survival of patients with symptomatic and asymptomatic papillary thyroid carcinoma: an observational study of 11,265 person-years of follow-up. Thyroid. 2016; 26:1472–9.
Article13. Marina M, Ceda GP, Aldigeri R, Ceresini G. Causes of referral to the first endocrine visit of patients with thyroid carcinoma in a mildly iodine-deficient area. Endocrine. 2017; 57:247–55.
Article14. Pisanu A, Reccia I, Nardello O, Uccheddu A. Risk factors for nodal metastasis and recurrence among patients with papillary thyroid microcarcinoma: differences in clinical relevance between nonincidental and incidental tumors. World J Surg. 2009; 33:460–8.
Article15. Malone MK, Zagzag J, Ogilvie JB, Patel KN, Heller KS. Thyroid cancers detected by imaging are not necessarily small or early stage. Thyroid. 2014; 24:314–8.
Article16. Bahl M, Sosa JA, Nelson RC, Esclamado RM, Choudhury KR, Hoang JK. Trends in incidentally identified thyroid cancers over a decade: a retrospective analysis of 2,090 surgical patients. World J Surg. 2014; 38:1312–7.
Article17. Brito JP, Al Nofal A, Montori VM, Hay ID, Morris JC. The impact of subclinical disease and mechanism of detection on the rise in thyroid cancer incidence: a population-based study in Olmsted County, Minnesota during 1935 through 2012. Thyroid. 2015; 25:999–1007.
Article18. Kim H, Park SY, Jung J, Kim JH, Hahn SY, Shin JH, et al. Improved survival after early detection of asymptomatic distant metastasis in patients with thyroid cancer. Sci Rep. 2019; 9:18745.
Article19. Chung WY, Chang HS, Kim EK, Park CS. Ultrasonographic mass screening for thyroid carcinoma: a study in women scheduled to undergo a breast examination. Surg Today. 2001; 31:763–7.
Article20. Choi YJ, Park YL, Koh JH. Prevalence of thyroid cancer at a medical screening center: pathological features of screen-detected thyroid carcinomas. Yonsei Med J. 2008; 49:748–56.
Article21. Moon S, Lee EK, Choi H, Park SK, Park YJ. Survival comparison of incidentally found versus clinically detected thyroid cancers: an analysis of a nationwide cohort study. Endocrinol Metab (Seoul). 2023; 38:81–92.
Article22. Solis-Pazmino P, Salazar-Vega J, Lincango-Naranjo E, Garcia C, Koupermann GJ, Ortiz-Prado E, et al. Thyroid cancer overdiagnosis and overtreatment: a cross-sectional study at a thyroid cancer referral center in Ecuador. BMC Cancer. 2021; 21:42.23. Farra JC, Picado O, Liu S, Ouyang W, Teo R, Franco AM, et al. Clinically significant cancer rates in incidentally discovered thyroid nodules by routine imaging. J Surg Res. 2017; 219:341–6.
Article24. Yoo F, Chaikhoutdinov I, Mitzner R, Liao J, Goldenberg D. Characteristics of incidentally discovered thyroid cancer. JAMA Otolaryngol Head Neck Surg. 2013; 139:1181–6.
Article25. Marina M, Serra MF, Aldigeri R, Ceresini G. Incidental versus clinically diagnosed differentiated thyroid cancer in both adult and elderly subjects: histological characteristics and follow-up in a retrospective analysis from a single institution. Endocrine. 2020; 68:584–91.
Article26. Oh CM, Kong HJ, Kim E, Kim H, Jung KW, Park S, et al. National epidemiologic survey of thyroid cancer (NEST) in Korea. Epidemiol Health. 2018; 40:e2018052.
Article27. Park S, Oh CM, Cho H, Lee JY, Jung KW, Jun JK, et al. Association between screening and the thyroid cancer “epidemic” in South Korea: evidence from a nationwide study. BMJ. 2016; 355:i5745.
Article28. Jung KW, Won YJ, Kong HJ, Oh CM, Cho H, Lee DH, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2012. Cancer Res Treat. 2015; 47:127–41.
Article29. Ahn HS, Kim HJ, Welch HG. Korea’s thyroid-cancer “epidemic”: screening and overdiagnosis. N Engl J Med. 2014; 371:1765–7.
Article30. Vaccarella S, Franceschi S, Bray F, Wild CP, Plummer M, Dal Maso L. Worldwide thyroid-cancer epidemic?: the increasing impact of overdiagnosis. N Engl J Med. 2016; 375:614–7.
Article31. Franceschi S, Vaccarella S. Thyroid cancer: an epidemic of disease or an epidemic of diagnosis? Int J Cancer. 2015; 136:2738–9.
Article32. Megwalu UC, Moon PK. Thyroid cancer incidence and mortality trends in the United States: 2000-2018. Thyroid. 2022; 32:560–70.
Article33. Nguyen QT, Lee EJ, Huang MG, Park YI, Khullar A, Plodkowski RA. Diagnosis and treatment of patients with thyroid cancer. Am Health Drug Benefits. 2015; 8:30–40.34. Shin JH, Baek JH, Chung J, Ha EJ, Kim JH, Lee YH, et al. Ultrasonography diagnosis and imaging-based management of thyroid nodules: revised Korean Society of Thyroid Radiology consensus statement and recommendations. Korean J Radiol. 2016; 17:370–95.
Article35. Ha EJ, Chung SR, Na DG, Ahn HS, Chung J, Lee JY, et al. 2021 Korean thyroid imaging reporting and data system and imaging-based management of thyroid nodules: Korean Society of Thyroid Radiology consensus statement and recommendations. Korean J Radiol. 2021; 22:2094–123.
Article36. Yi KH, Lee EK, Kang HC, Koh Y, Kim SW, Kim IJ, et al. 2016 Revised Korean Thyroid Association management guidelines for patients with thyroid nodules and thyroid cancer. Int J Thyroidol. 2016; 9:59–126.
Article37. Moon JH, Kim JH, Lee EK, Lee KE, Kong SH, Kim YK, et al. Study protocol of multicenter prospective cohort study of active surveillance on papillary thyroid microcarcinoma (MAeSTro). Endocrinol Metab (Seoul). 2018; 33:278–86.
Article38. Jeon MJ, Kang YE, Moon JH, Lim DJ, Lee CY, Lee YS, et al. Protocol for a Korean multicenter prospective cohort study of active surveillance or surgery (KoMPASS) in papillary thyroid microcarcinoma. Endocrinol Metab (Seoul). 2021; 36:359–64.
Article39. Prorok PC. Epidemiologic approach for cancer screening: problems in design and analysis of trials. Am J Pediatr Hematol Oncol. 1992; 14:117–28.40. Kramer BS, Brawley OW. Cancer screening. Hematol Oncol Clin North Am. 2000; 14:831–48.
Article41. Carlson MD, Morrison RS. Study design, precision, and validity in observational studies. J Palliat Med. 2009; 12:77–82.
Article42. Boyko EJ. Observational research: opportunities and limitations. J Diabetes Complications. 2013; 27:642–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thyroid cancer screening
- Evaluation of Mass Screening for Thyroid Cancer
- Screening of Thyroid Cancer and Management of Thyroid Incidentaloma
- Value of Ultrasonographic Mass Screening for Thyroid Carcinoma in Patients Undergoing a Breast Ultrasonography
- No Change in Complications Following Thyroidectomy Despite Increase in Thyroid Cancer Surgeries: A Meta-Regression Analysis